Abstract
Background: The hyper-CVAD regimen is an effective frontline regimen for de novo adult ALL. Expression of CD20 was identified as an adverse prognostic factor, associated with a higher incidence of relapse, lower 3-year complete remission duration (CRD) and lower 3-year overall survival (OS) rate. The addition of rituximab to the hyper-CVAD regimen in pts with CD20-positive ALL (≥20% expression by multicolor flow cytometry - FCI) improved outcome with 3-year CRD and OS rates by 68% and 65%, respectively. Ofatumumab (HuMax-CD20) targets a membrane proximal small-loop epitope on the CD20 molecule and was found to be more potent than rituximab in promoting complement-dependent cytotoxicity in vitro. Ofatumumab's safety and efficacy has been proven in chronic lymphocytic leukemia. Therefore a combination of the hyper-CVAD regimen and ofatumumab may be associated with better response rates, higher 3-year CRD and overall survival rates.
Methods: Pts with newly diagnosed ALL and pts who received one prior course of chemotherapy received 4 courses of hyper-CVAD (fractionated cyclophosphamide, vincristine [VCR], doxorubicin, dexamethasone; the odd courses 1, 3, 5, 7); ofatumumab was given on courses 1 and 3, and 4 courses of MTX-Ara-C (methotrexate-cytarabine; the even courses 2, 4, 6, 8); ofatumumab was given on courses 2 and 4. This treatment would be followed by POMP (6-mercaptopurine, MTX, VCR, prednisone) maintenance therapy for approximately 30 months, interrupted by intensifications months 6, 7 and 18, 19 with MTX/Pegylated asparaginase and hyper-CVAD-ofatumumab. Central nervous system prophylaxis with MTX and ara-C was administered. When indicated local radiotherapy was administered in patients with bulky mediastinal disease
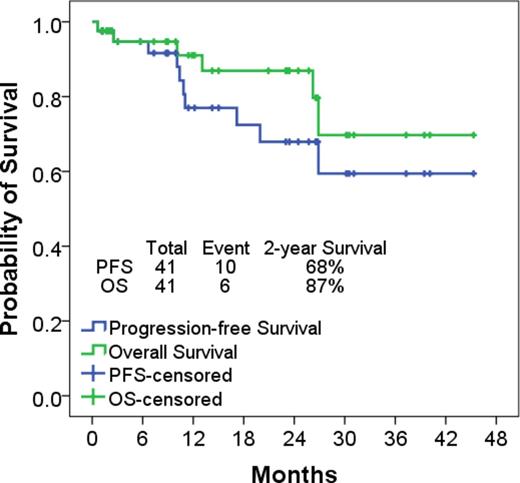
Results: To date 37 pts with de novo ALL and 4 pts in complete remission (CR) previously treated (2 with prior cycle of hyper-CVAD, 1 post fludarabine-cytarabine based regimen, 1 with cyclophosphamide and dexamethasone) have received a median of 6 cycles (1-8) of therapy. Median age is 46 years (32-71). Median WBC at diagnosis was 5.4 x 109/L (1 -202 x 109/L). CD20 expression above 20% was found in 27 pts (66%), between 10 and 20% in 3 (7%) and below 10% in 11 (27%). 2 pts (5%) had concomitant CNS disease at diagnosis. Among the 34 pts with evaluable baseline cytogenetic analysis, 20 (49%) were abnormal. All but one pt (97%) achieved a CR after cycle 1 (4 pts were in CR at the start); 1 pt died of septic shock and multiple organ failure at day 21 of cycle 1. Thirty-eight (95%) pts achieved minimal residual disease (MRD) negativity as assessed by FCI; of whom 23 (64%) achieved MRD negativity after induction. Ten (27%) pts did not receive the full 8 planned courses of induction-consolidation; 16 (43%) pts are receiving maintenance in CR; 4 (11%) pts finished all treatment; 5 (%) pts were referred to allogeneic stem cell transplantation due to multiple cytogenetic abnormalities and delay in achieving negative MRD. Median time to neutrophil and platelet recovery for cycle 1 was 18 and 22 days after induction chemotherapy, respectively. Grade ≥ 3 toxicity included increase of LFT's in 13 pts (32%), increase of bilirubin in 7 (17%), nausea/vomiting in 4 (10%), mucositis in 3 (7%), neuropathy in 3 (7%), and thrombotic events in 1 (2%). Febrile neutropenia episodes during induction and consolidation cycles were reported at rates of 67% and 89%, respectively. With a median follow up of 15 months (1-45), 35 pts are alive; 6 pts relapsed and one had molecular relapse only. Six pts died: 1 at C1D22 of sepsis and intracranial bleed; 1 at C3D17 of sepsis and multiple organ failure; 1 at maintenance C16D35 of sepsis; 1 of relapse post ASCT; 1 post salvage therapy for minimal residual disease relapse; 1 of progressive disease after relapse. The 2-year PFS and OS rates were 68% and 87% respectively.
Conclusion: The combination of hyper-CVAD with ofatumumab is safe and highly effective in pts with CD20-positive ALL.
Patient characteristics and outcome
| . | N (%)/Median [range] N=41 . | |
|---|---|---|
| Age (yrs) | 44 [22-71] | |
| Sex | Male | 25 (61) |
| Female | 16 (39) | |
| PS | 0-1 | 38 (93) |
| 2-3 | 3 (7) | |
| WBC (x 109/L) | 5.4 [0.7-201.7] | |
| CNS disease positivity | 2 (5) | |
| CD20 + (%) | 1-10 | 9 (22) |
| 10-20 | 3 (7) | |
| >20 | 27 (66) | |
| Pos | 2 (5) | |
| CG | Diploid | 14 (34) |
| Abnormal | 20 (49) | |
| IM/ND | 7 (17) | |
| Response | CR | 37/38 (97) |
| CR after induction | 37/38 (97) | |
| MRD at CR | 23/36 (64) | |
| MRD overall | 38/40 (95) | |
| Early death | 1 (3) | |
| . | N (%)/Median [range] N=41 . | |
|---|---|---|
| Age (yrs) | 44 [22-71] | |
| Sex | Male | 25 (61) |
| Female | 16 (39) | |
| PS | 0-1 | 38 (93) |
| 2-3 | 3 (7) | |
| WBC (x 109/L) | 5.4 [0.7-201.7] | |
| CNS disease positivity | 2 (5) | |
| CD20 + (%) | 1-10 | 9 (22) |
| 10-20 | 3 (7) | |
| >20 | 27 (66) | |
| Pos | 2 (5) | |
| CG | Diploid | 14 (34) |
| Abnormal | 20 (49) | |
| IM/ND | 7 (17) | |
| Response | CR | 37/38 (97) |
| CR after induction | 37/38 (97) | |
| MRD at CR | 23/36 (64) | |
| MRD overall | 38/40 (95) | |
| Early death | 1 (3) | |
Cortes:Teva: Research Funding; BerGenBio AS: Research Funding; Pfizer: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Ariad: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Astellas: Consultancy, Research Funding; Ambit: Consultancy, Research Funding; Arog: Research Funding; Celator: Research Funding; Jenssen: Consultancy. Chahoud:American Society of Hematology (ASH): Other: 2015 HONORS Award recipient. Verstovsek:Incyte Corporation: Research Funding. Konopleva:Novartis: Research Funding; AbbVie: Research Funding; Stemline: Research Funding; Calithera: Research Funding; Threshold: Research Funding. O'Brien:Pharmacyclics LLC, an AbbVie Company: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal