Abstract
INTRODUCTION: The Bruton's tyrosine kinase (BTK) inhibitor ibrutinib is a covalent inhibitor of BTK, a member of the B-cell receptor (BCR) signaling pathway and induces objective clinical responses in the majority of CLL patients (Byrd et al., NEJM 2013). Interestingly this drug also inhibits L2-inducible T cell kinase (ITK), an essential enzyme for the development and effector function of Th2 and Th17 cells, and has been shown to shift the balance towards a Th1 response. The purpose of the study was to determine how ibrutinib influences the Th1/Th17/T regulatory cell response, expression of immune checkpoint blockade molecules on T cells and the functional pathogen-specific T cell recovery.
METHODS: Here we present data from a clinical trial of ibrutinib versus ibrutinib + rituximab in previously treated patients (NCT02007044). Peripheral blood and serum were collected at baseline, 3 months and 6 months during therapy. Multicolor flow cytometry was used to characterize B cell subsets, T-cell subsets, expression of PD-1, PD-L1 and CTLA-4 and T-cell effector function. For statistical analysis of pre-treatment to on-treatment measurements the paired Student t-test was used.
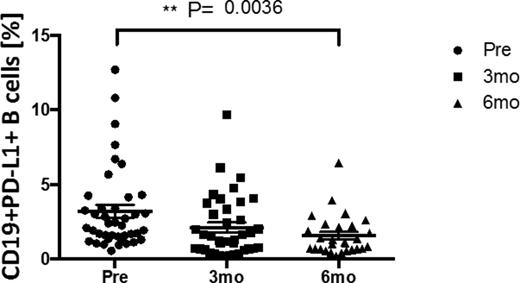
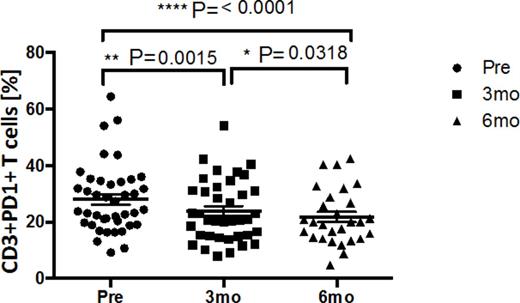
RESULTS: Here we report on the phenotypic and functional recovery of immune subsets in 41 CLL patients treated with ibrutinib (n=17) or ibrutinib + rituximab (n=25). Both PD-1 and PD-L1 were expressed at high levels on CLL cells. Interestingly, by 3 and 6 months, there was a significant decrease in PD-1 expression from a pre-treatment median of 15% to 4% (at 3 months) and 3% (at 6 months; P<0.0001). Similarly, PD-L1 levels decreased from 5% to 3% and 2% respectively (P=0.004) (Fig. 1). We next sought to determine the functional impact of ibrutinib therapy on T cell subsets and function. After an initial reduction from a pretreatment level of4800/µL to 3000/µL at 3 months (P=0.003), CD3+ T cells increased to 4000 (µL) by 6 months; P=0.03. This was associated with a significant down-regulation of PD-1 expression on T cells from 28% pre-treatment to 24% and 21% at 3 and 6 months respectively (Fig.2 ) (P<0.0001). A significant reduction in the frequencies of regulatory T cells (Teg) (8% vs. 7% vs 6% respectively; P=0.004) was also documented. Ibrutinib has been reported to skew the T cell response toward a Th1 profile. We stimulated PBMC with PMA/Inomycin and performed intracellular staining for IFN-γ, IL-2, TNF-α and IL-17. Following ibrutinib therapy, there was a significant improvement in the CD8+ IFN-γ (P=0.04) and TNF-α response (P=0.01), and a reduction in the CD4+IL-17 response. To understand the functional relevance of these results, we are currently analyzing the CD8+ T cell response to stimulation with CEF (epitopes derived from CMV, EBV and Influenza) as a surrogate for pathogen-specific T cell recovery.
CONCLUSION:
Based on these data we propose that ibrutinib therapy can modulate the T cell response through multiple mechanisms which include (i) direct inhibition of ITK and skewing of the T cell response toward a Th1 profile; (ii) reduction in PD1/PDL1 expression on B and T cells and (iii). suppression of Tregs. It is unclear how ibrutinib influences the PD1/PDL1 interaction and whether this is a direct effect of the drug on essential components of B and T cell-receptor signaling or whether it is an indirect effect related to a reduction in the leukemia burden. Mechanistic studies to understand how ibrutinib modulates the PD1/PL1 axis are currently underway.
Ibrutinib therapy is associated with a reduction in PDL1 expression on the surface of CD19+ B cells.
Ibrutinib therapy is associated with a reduction in PDL1 expression on the surface of CD19+ B cells.
Ibrutinib therapy is associated with a reduction in PD1 expression on the surface of CD3+ T cells.
Ibrutinib therapy is associated with a reduction in PD1 expression on the surface of CD3+ T cells.
Burger:Pharmacyclics LLC, an AbbVie Company: Research Funding. Wierda:Glaxo-Smith-Kline Inc.: Research Funding; Celgene Corp.: Consultancy. Rezvani:Pharmacyclics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal