Abstract
Background
The impact of cytomegalovirus (CMV) infection on the risk of relapse after Hematopoietic Cell Transplantation (HCT) remains controversial, with some studies demonstrating lower risk (Green et al, Blood 2013), while others demonstrating no impact (Schmidt-Hieber et al, Blood 2013), or lower relapse risk only in myeloablative (MA) (Manjappa et al, BBMT, 2014) or in reduced intensity conditioning (RIC) (Cichocki et al, ASH 2014) HCT. Furthermore, the majority of studies have used antigenemia for CMV monitoring, while there is limited data with the use of Quantitative Nucleic Acid Testing (QNAT).
Aim
To determine the impact of CMV infection, as detected by QNAT, on transplant-related outcomes for patients with acute myeloid leukemia (AML), stratified by MA or RIC HCT.
Methods
After IRB approval, consecutive adults with AML who underwent allogenic HCT from HLA-matched peripheral blood (PB) grafts at our institution between 2006 and 2014 were retrospectively reviewed. All grafts were T-cell replete. Early CMV infection was defined as any positive CMV result by PCR assay during the first 100 days post HCT. Relapse incidence (RI), non-relapse mortality (NRM), disease-free survival (DFS), and overall survival (OS) were compared between patients with and without CMV infection, and stratified according to MA or RIC. DFS and OS were estimated using the Kaplan-Meier method, and compared with log-rank test. Cumulative incidence of relapse and NRM were analyzed as competing events, using Gray's test. Multivariable analyses adjusting for patient's age, disease status at transplant, cytogenetic risk, and ABO incompatibility were performed using Cox's proportional hazards regression, and the Fine and Gray approach.
Results
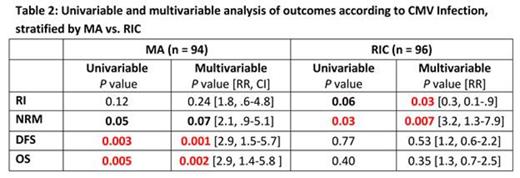
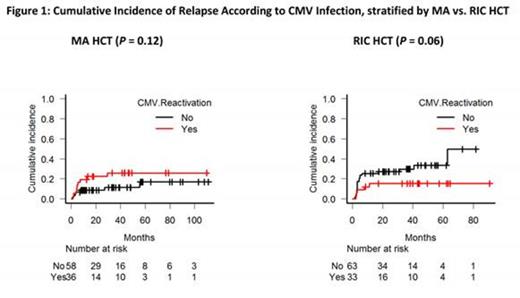
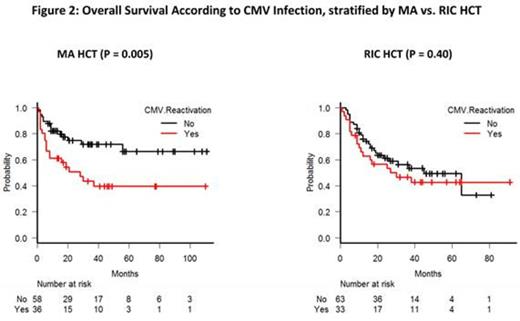
A total of 190 consecutive patients, including 94 (49%) MA and 96 (51%) RIC HCT were analyzed. Patients, disease, and transplant characteristics are shown in table 1. Of the 94 MA HCT (median age 45 y, 50% male), 66 (70%) received total body irradiation. After a median follow up of 18 m, 36 (38%) CMV infection, 16 (17%) relapses, 22 (23%) NRM and 35 (37%) deaths occurred in the MA group. Median time to CMV infection and to relapse in this group was 38 (range 8-241) and 140 (29-1690) days, respectively. Among the recipients of MA HCT, patients with early CMV infection showed no difference in the RI (figure 1), but had a significant trend towards higher NRM and significantly lower DFS and OS in both univariate and multivariable analysis (figure 2) (P values shown in table 2).
Among 96 RIC HCT (median age 59 y, 56% male), fludarabine plus melphalan was used in 62 (65%) and fludarabine plus busulfan in 34 (35%) patients. In this group, early CMV infection occurred in 33 (34%), relapse in 25 (26%), NRM in 25 (26%), and deaths in 46 (48%) patients after a median follow up of 21 m (1-91 m). Among the recipients of RIC HCT, median time to CMV infection and to relapse was 40 (17-175) and 291 (19-1971) days, respectively. In the RIC group, early CMV infection was associated with a significant trend towards lower RI (figure 1) and higher NRM in both univariable and multivariable analysis, but no difference in DFS and OS (figure 2).
Conclusion
Our study of a large homogenous group of AML patients who underwent a uniform HLA-matched PB HCT demonstrates a significantly lower risk of relapse associated with early CMV infection detected by QNAT following RIC, but not MA HCT. Early CMV infection in MA HCT is associated with higher NRM and therefore inferior survival, whereas in the RIC HCT, there is no impact on survival as the benefit of lower relapse is offset by the higher NRM.
Patients, disease and transplant characteristics according to CMV infection
| . | All Patients . | Patients with CMV Viremia . | Patients without CMV Viremia . | P value . |
|---|---|---|---|---|
| Patients, no (%) | 190 (100) | 69 (36) | 121 (64) | - |
| Median age, y (range) | 54 (18-72) | 54 (26-70) | 54 (18-72) | 0.75 |
| Male Patients, no (%) | 104 (55) | 30 (43) | 74 (61) | 0.02 |
| D/R CMV Serostatus, no (%) | <0.0001 | |||
| -/- | 29 (15) | 1 (1) | 28 (23) | |
| +/+ | 64 (34) | 35 (51) | 29 (24) | |
| +/- | 13 (7) | 1 (1) | 12 (10) | |
| -/+ | 84 (44) | 32 (47) | 52 (43) | |
| Conditioning | 0.65 | |||
| MA | 96 (51) | 33 (48) | 63 (52) | |
| RIC | 94 (49) | 36 (52) | 58 (48) | |
| Disease status at Transplant | 0.96 | |||
| CR1 | 129 (68) | 46 (67) | 83 (69) | |
| CR2 | 34 (18) | 13 (19) | 21 (17) | |
| Other | 27 (14) | 10 (14) | 17 (14) | |
| Cytogenetic | 0.65 | |||
| Favorable | 8 (4) | 2 (3) | 6 (5) | |
| Intermediate | 130 (68) | 46 (67) | 84 (69) | |
| Unfavorable | 52 (28) | 21 (30) | 31 (26) | |
| . | All Patients . | Patients with CMV Viremia . | Patients without CMV Viremia . | P value . |
|---|---|---|---|---|
| Patients, no (%) | 190 (100) | 69 (36) | 121 (64) | - |
| Median age, y (range) | 54 (18-72) | 54 (26-70) | 54 (18-72) | 0.75 |
| Male Patients, no (%) | 104 (55) | 30 (43) | 74 (61) | 0.02 |
| D/R CMV Serostatus, no (%) | <0.0001 | |||
| -/- | 29 (15) | 1 (1) | 28 (23) | |
| +/+ | 64 (34) | 35 (51) | 29 (24) | |
| +/- | 13 (7) | 1 (1) | 12 (10) | |
| -/+ | 84 (44) | 32 (47) | 52 (43) | |
| Conditioning | 0.65 | |||
| MA | 96 (51) | 33 (48) | 63 (52) | |
| RIC | 94 (49) | 36 (52) | 58 (48) | |
| Disease status at Transplant | 0.96 | |||
| CR1 | 129 (68) | 46 (67) | 83 (69) | |
| CR2 | 34 (18) | 13 (19) | 21 (17) | |
| Other | 27 (14) | 10 (14) | 17 (14) | |
| Cytogenetic | 0.65 | |||
| Favorable | 8 (4) | 2 (3) | 6 (5) | |
| Intermediate | 130 (68) | 46 (67) | 84 (69) | |
| Unfavorable | 52 (28) | 21 (30) | 31 (26) | |
Al-Kali:Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal