Abstract
Background. Similar probabilities of survival have been reported for patients transplanted from Matched Unrelated Donor (MUD), Umbilical Cord Blood (UCB) or Haploidentical (Haplo) donors as alternative hematopoietic stem cell sources. However, few studies have compared these results with those obtained in patients transplanted from HLA Id-siblings (Id-sib). Moreover, all reported studies are retrospective and the criteria of donor selection were not predefined. We report the intention to treat (ITT) analysis results on 238 patients with high-risk acute myeloid leukemia (AML) prospectively transplanted according to the policy of the Rome Transplant Network (RTN), a metropolitan transplant program established in Rome in 2006.
Patients and Methods. For AML patients eligible to an allogeneic transplant, the RTN policy consists of an algorithm of donor choice based on a hierarchy according to the following criteria: 1) HLA identical sibling; 2) MUD ≥8/10 HLA 3) UCB as single unit selected on the base of cell dose and number of HLA disparities (0-1/6 HLA: TNC ≥2.5x107/kg and CD34 ≥1x105/kg; 2/6 HLA: TNC ≥3.5x107/kg and CD34 ≥2x105/kg); 4) G-CSF primed, unmanipulated bone marrow Haplo donor. Myeloablative (MAC) or reduced intensity (RIC) TBF (Tiothepa, Busulfan, Fludarabine) conditioning regimen was identical for all patients, GVHD prophylaxis was uniform for each categories. of transplant
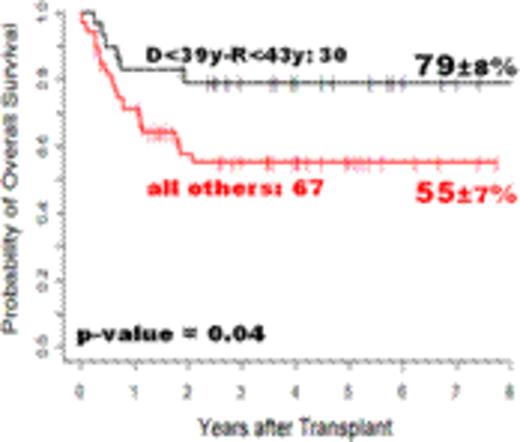
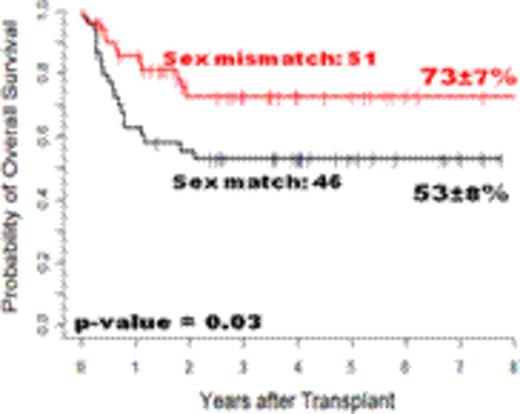
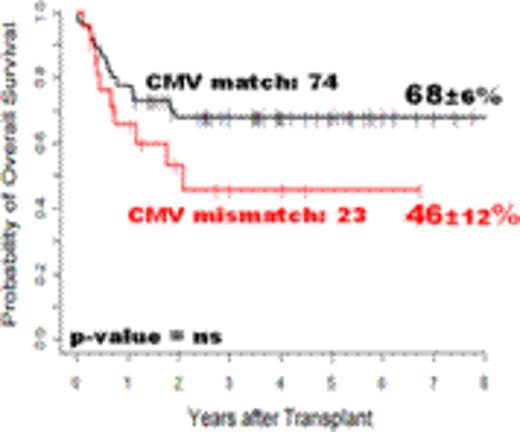
Results. From January 2006 to December 2014, 238(89%) out of 303 adult patients candidates to an allogeneic transplant for high-risk AML were considered eligible. Overall, a donor was available for 205 (86%) of 238 eligible patients. At time of the analysis, 17 of these 205 patients (8%) had lost the transplant eligibility and 4 (2%) were still scheduled for transplant, therefore 184/205 (90%) patients with an available donor were finally transplanted from Id-sib (n=76), MUD (n=38), UCB (n=17) or Haplo (n=53) donors. The 8-yrs overall survival (OS) of the 238 eligible patients from time of HLA typing and of the 184 transplanted patients from time of the graft was 40±4%and 43±4%, respectively. By excluding the low number of UCB recipients (n=17), the OS was particularly dismal for the 34 patients transplanted in advanced disease phase (7±4% at 4 yrs), whereas for the 132 patients transplanted in early (CR1+ CR2) phase the 8-yr OS was 56±5%: 58±7% for 61 HLA Id-sib, 50±8% for 40 Haplo and 63±10% for 27 MUD recipients (P=NS). The OS of patients transplanted in early phase was 63±5% for 97 patients receiving MAC and 33±9% for RIC recipients. For these 97 patients, the survival by type of donor was 62±10% either for 47 Id-sib or 28 Haplo and 70±10% for 22 MUD recipients (P=NS). The results were analyzed by various donor/recipient (D/R) combinations such as age, sex and CMV status. The median donor age was 39 years (range, 18-70) and the median patient age was 43 years (range, 16-59): the 8-yr OS of patients (n=30) with younger D/R combination (D<39y-R<43y) was79±9%, significantly higher than 55±7% observed for the other D/R combinations (P=0.04). The 4 D/R sex combinations were homogeneously distributed among Id-sib, MUD and Haplo recipients: for 51 sex mismatched (DM/RF; DF/RM) patients the 8-yr OS was 73±7%, significantly higher than the 53±8% rate observed for 46 sex matched patients (P=0.03). Finally, the 8-yr OS by D/R CMV status was 68±6% for 74 D/R CMV matched and 46±12% for D/R CMV mismatched patients (P=NS). In multivariate analysis, the factors influencing survival were D/R age (P=0.059), D/R sex (P=0.03) and D/R CMV status (P=0.04). The donor source (Id-sib vs MUD vs Haplo) did not affect survival (P=NS).
Conclusions. RTN policy allowed donor identification in 86% of all eligible AML patients and allowed an allogeneic transplant to be carried out in 90% of them with no substantial differences in terms of long-term survival between initially eligible (ITT analysis) and definitively transplanted patients. Only the definition of a specific transplant policy and the ITT analysis allow to evaluate the real impact of a transplant program. As the probability of survival is not substantially different comparing different donor stem cell sources, the final conclusion which can be drawn from our study is that for patients with AML undergoing an allogeneic transplant, the HLA matching is unlikely to remain the first criterion for donor identification. Other factors such as D/R age, sex and CMV status should drive the search for the best donor.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal