Abstract
Background: Post-transplantation cyclophosphamide (PTCy) is an effective strategy to prevent GVHD after haploidentical or HLA-matched related or unrelated donor hematopoietic stem cell transplantation (HSCT). Our study aim was to determine its efficacy in HLA-mismatched unrelated donor (MMUD) HSCT.
Methods: We included 113 consecutive adult patients with high risk hematological malignancies who underwent one-antigen MMUD (9/10-matched) bone marrow (BM) or peripheral blood (PB) HSCT after myeloablative or reduced-intensity conditioning at our institution from 2009-2013. Outcomes were compared between (a) conventional GVHD group (n=71) that received in-vivo T-cell depletion with ATG, tacrolimus and methotrexate and (b) PTCy group (n=41) that received PTCy (50 mg/kg/day IV on days 3 and 4) with tacrolimus and MMF. After exclusion of 29 patients with isolated HLA-DQ mismatches, a separate analysis was performed in 84 patients with 7/8 HLA-MUD HSCT; 38 patients received PTCy while 46 patients received conventional prophylaxis.
Results: Patients in the conventional group were marginally older (median 54 years; range 19-74) than those in the PTCy group (median 50 years; range 20-64). PB was used more frequently as a graft source in the conventional group (38% vs 17%, p=0.02). PTCy group included more patients with HLA class-I mismatches (87.8%) compared to conventional group (56.9%). There were no other differences between the groups.
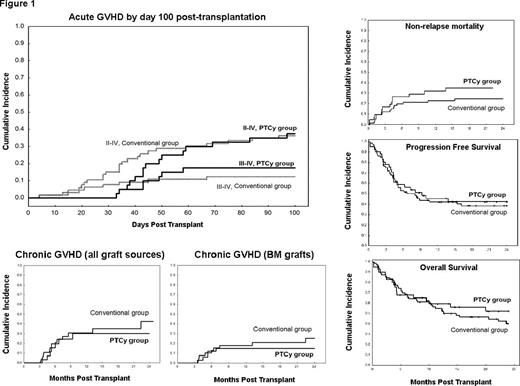
Incidence of grade II-IV (37% vs 36%, p=0.8) or grade III-IV (17% vs 12%, p=0.5) acute GVHD at day 100 post-transplant was not different between the groups. [Figure 1] Incidence of grade II-IV acute GVHD at day 30 was significantly lower after PTCy compared with conventional prophylaxis (0% vs 15%, p <0.001). Correspondingly, incidence of grade III-IV GVHD at day 30 was 0% in the PTCy group and 8% in the conventional group (p=0.08). Cumulative incidence of chronic GVHD was similar between the two groups at 6 months (20% vs 15%), 1-year (30% vs 31%) or 2-years (30% vs 42%). Risk factors analysis showed that use of PTCy was the sole independent predictor of lower risk of grade II-IV acute GVHD at day 30 (p=0.01). None of the risk factors evaluated, including PTCy use, were shown to predict the rate of grade II-IV acute GVHD within day 100. Two-year cumulative incidences of NRM (35% vs 25%), disease progression (20% vs 31%), DFS (42% vs 38%) and OS (52% vs 40%) were similar in the PTCy and the conventional groups, respectively. [Figure 1] Median times to neutrophil (18 vs. 12 days, p<0.001) and platelet (25.5 vs. 18 days, p=0.05) engraftment were prolonged in PTCy group. Disease recurrence/persistence was the leading cause of death in both groups, accounting for about 46% of all deaths. Subgroup analysis restricting to patients with BM grafts produced similar findings.
In patients with HLA class-I mismatch, PTCy was associated with significantly reduced risk of grade II-IV, but not grade III-IV, acute GVHD at day 30 (p=0.01). However, there were no differences in acute grade II-IV GVHD (HR 1.1, 95% C.I. 0.5-2.5, p=0.7) or acute grade III-IV GVHD (HR 1.5, 95% C.I. 0.4-5.4, p=0.5) by day 100 between the groups.
Comparing patients with 7/8-HLA-MUD HSCT, no patient in PTCy group developed acute GVHD at day 30 compared with 8 patients in conventional group (p=0.005). There were no differences in incidence of grade II-IV (HR 1, 95% C.I. 0.5-2.1, p=0.9) or grade III-IV (HR 1.1, 95% C.I. 0.3-3.3, p=0.9) acute GVHD at day 100, chronic GVHD at 6 months (HR 0.8, 95% C.I. 0.2-2.9, p=0.7), 1-year (HR 0.8, 95% C.I. 0.3-2.2, p=0.6) or 2-years (HR 0.7, 95% C.I. 0.2-1.9, p=0.5) between the groups.
Conclusion: Our results demonstrate that PTCy, tacrolimus and MMF for GVHD prophylaxis is safe and produced similar results as conventional prophylaxis in patients with one antigen HLA-MMUD HSCT.
Alousi:Therakos, Inc: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal