Abstract
Background:Morphologic complete remission (CR) is the gold standard for assessing response in acute myelogenous leukemia (AML). CR with incomplete count recovery (CRi) and CR with incomplete platelet recovery (CRp) are associated with inferior overall survival post induction therapy (Walter et al, JCO 2010 and Chen et al, JCO 2015). Furthermore, residual cytogenetic disease is associated with a higher relapse compared with patients with cytogenetic CR (CCR; Chen et al, JCO 2011). There is a paucity of literature regarding the impact of CRi, CRp and CCR prior to allogeneic transplantation.
Aim:To study the impact of CRi, CRp and CCR and their impact on relapse incidence (RI), non-relapse mortality (NRM) and overall survival (OS) in reduced intensity allogeneic stem cell transplantation (RIC-SCT).
Methods:After due IRB approval, patients (pts) with acute myelogenous leukemia (AML) or myelodysplastic syndrome (MDS) who received RIC-SCT at our institution between 2008-2014 were identified. All clinical and pathologic data were retrospectively extracted. CR, CRi, CRp and CCR were defined in accordance to the international working group definition. Categorical and continuous variables were analyzed using Pearson's chi-squared and Wilcoxon/Kruskal-Wallis, respectively. Survival estimates were calculated using the kaplan-meier and log-rank test. RI was estimated on a competing event analysis using Grey's model. Cox proportional regression was used to compute hazard ratios (HR).
Results:
A. Baseline characteristics: A total of 134 patients were identified. A total of 70 (52%) were in CR, 40 (30%) in CRi and 24 (18%) in CRp. 129 patients had evaluable cytogenetic data pre-SCT; 81 (63%) were in CCR and 48 (37%) had persistent cytogenetic disease. Baseline patient, disease and transplant characteristics stratified by peripheral count recovery pre-SCT are shown (Table 1). Significantly more patients in CR had higher KPS, higher proportion AML diagnosis, more likely to be in first complete remission (CR1), higher rate of cytogenetic CR and a higher proportion of minor ABO mismatched donor. No other significant variables were identified between the three cohorts.
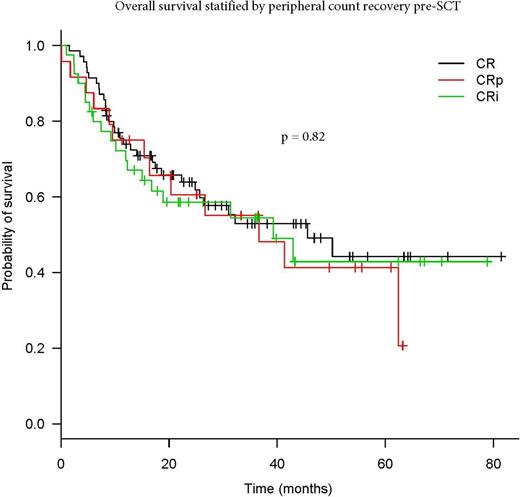
B. Transplant outcomes: Median follow up of the entire cohort was 41.9 months and the 2-yr OS, RI and NRM were 61.7%, 25.7% and 21.9%. Patients in CR, CRi and CRp had a similar 2-year rates of RI (26.3%, 18.4% and 28.9%, respectively; p = 0.66), 2-year NRM (20.5%, 38.8% and 22.1%, respectively; p = 0.18) and 2-year OS (61.8%, 55.1% and 58.6%, respectively; p = 0.82). RI was significantly lower for patients in CCR pre-SCT with HR 0.25 (95% CI 0.11-0.51 p = 0.0001) without a difference in overall survival HR 0.68 (0.41-1.15; p = 0.14). However, we observed a similar RI in CR, CRi and CRp patients who had persistent cytogenetic disease pre-SCT (p = 0.55). The outcome remained similar between strata after excluding MDS patients (data not shown).
Conclusion: We observed equivalent post-transplant outcomes between CR, CRi and CRp despite the presence of persistent cytogenetic disease. This suggests that RIC SCT had a role in mitigating the negative prognosis associated incomplete hematologic recovery. These findings have implications as physicians may not need to postpone SCT to await count recovery. This important question should be further validated in a larger cohort of patients.
Al-Kali:Novartis: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal