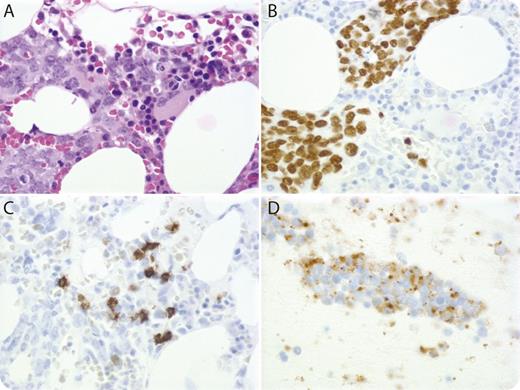
A 77-year-old woman with a remote smoking history presented with progressive dyspnea, chest discomfort, and hypoxia. Computed tomography showed extensive mediastinal, hilar, and perisplenic adenopathy. Her laboratory work was notable for thrombocytopenia (platelets = 77 K/μL), mild anemia (hemoglobin = 11.2 g/dL), high lactate dehydrogenase (4325 IU/L), and hyperuricemia (11.2 mg/dL). Because of a concern for high-grade lymphoma, the patient underwent bone marrow (BM) biopsy, which showed extensive infiltration by atypical cells (panel A) immunoreactive for thyroid transcription factor-1 (panel B) and chromogranin (weakly), and nonimmunoreactive for CD20 (panel C), CD3, CD34, and CD117. Flow cytometric analysis revealed a small population of CD20(dim)CD5+CD23+ B cells, positive for clonal immunoglobulin heavy chain gene rearrangement by polymerase chain reaction, suggestive of monoclonal B-cell lymphocytosis. Fine needle aspiration biopsy of a mediastinal lymph node confirmed the diagnosis of small cell lung cancer (SCLC) (panel D; chromogranin immunostain). The patient started chemotherapy with carboplatin and etoposide but died from tumor lysis syndrome.
BM involvement is common in SCLC, but because of a lack of independent prognostic value, it is not a routine part of SCLC staging. On the other hand, SCLC can mimic high-grade lymphoma, especially when it presents with extensive nodal and/or BM involvement without an identifiable primary lesion, in which cases, BM biopsy can be valuable for differential diagnosis.
A 77-year-old woman with a remote smoking history presented with progressive dyspnea, chest discomfort, and hypoxia. Computed tomography showed extensive mediastinal, hilar, and perisplenic adenopathy. Her laboratory work was notable for thrombocytopenia (platelets = 77 K/μL), mild anemia (hemoglobin = 11.2 g/dL), high lactate dehydrogenase (4325 IU/L), and hyperuricemia (11.2 mg/dL). Because of a concern for high-grade lymphoma, the patient underwent bone marrow (BM) biopsy, which showed extensive infiltration by atypical cells (panel A) immunoreactive for thyroid transcription factor-1 (panel B) and chromogranin (weakly), and nonimmunoreactive for CD20 (panel C), CD3, CD34, and CD117. Flow cytometric analysis revealed a small population of CD20(dim)CD5+CD23+ B cells, positive for clonal immunoglobulin heavy chain gene rearrangement by polymerase chain reaction, suggestive of monoclonal B-cell lymphocytosis. Fine needle aspiration biopsy of a mediastinal lymph node confirmed the diagnosis of small cell lung cancer (SCLC) (panel D; chromogranin immunostain). The patient started chemotherapy with carboplatin and etoposide but died from tumor lysis syndrome.
BM involvement is common in SCLC, but because of a lack of independent prognostic value, it is not a routine part of SCLC staging. On the other hand, SCLC can mimic high-grade lymphoma, especially when it presents with extensive nodal and/or BM involvement without an identifiable primary lesion, in which cases, BM biopsy can be valuable for differential diagnosis.
For additional images, visit the ASH IMAGE BANK, a reference and teaching tool that is continually updated with new atlas and case study images. For more information visit http://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal