To the editor:
Essential thrombocythemia (ET), polycythemia vera, and primary myelofibrosis constitute a group of hematological disorders classically identified as BCR-ABL–negative myeloproliferative neoplasms (MPNs).1,2 Our understanding of the etiology of MPNs has benefited from the identification of somatic mutations in several genes, explaining >90% of the cases.3-6 Thus, somatic mutations in JAK2 are present in 60% of MPN cases, CALR mutations have been described in up to 30% of ET and primary myelofibrosis, and MPL mutations in up to 5% of cases.1,2 Genomic and clonogenic analysis have confirmed that MPNs arise through the acquisition of somatic mutations in any of these genes or other less frequently mutated genes. Nevertheless, it is still unclear how the myeloproliferative disorder progresses from the appearance of the driver mutation to the first clinical manifestations.
In this work, we report for the first time a case of apparent intraplacental spread of an MPN-precursor hematopoietic stem cell clone between 2 monozygotic twins that developed ET symptoms at 16 years of age. Although a case of primary thrombocythemia in monozygotic twins has been described,7 whole genome sequencing (WGS) of granulocytic cells from the 2 twins allowed us to provide molecular evidence for the monoclonal origin of them. In addition, we found a very low mutation burden, with all somatic mutations being originated before spreading to the other twin.
The index case (twin A) is a 16-year-old female who presented incidental thrombocytosis (913 × 109/L) in routine analysis after suffering herpes zoster infection and hemorrhagic diathesis. Bone marrow biopsy revealed hypercellular marrow with increased megakaryocytes. Hematological analysis performed on her monozygotic twin (twin B) also confirmed thrombocytosis (801 × 109/L). Molecular analysis of samples at diagnoses discarded the presence of JAK2 mutation p.V617F but revealed the presence of the same CALR gene 52-bp deletion (p.L367fs*46) in genomic DNA obtained from blood samples. None of the parents carried the mutation, nor was it detected on CD3+ purified lymphocytes from the affected siblings. The finding of twins developing clonal thrombocytosis synchronously early on in life, together with its low prevalence among adolescents,8,9 suggested the existence of either genetic predisposition, or a direct transfer in utero of a mutated precursor clone from 1 sister to the other. To investigate which of those scenarios was responsible for the simultaneous detection of MPN, WGS was performed on purified granulocytes from both twins, as well as on T cells used as germ-line control as previously described,5,6 in order to identify somatic mutations and germ-line variants in both patients. Research was approved by the hospital ethical committee, with informed consent. We achieved a callability, the proportion of the genome covered by at least 15 reads, of >97%, and somatic mutations and germ-line variants were identified using Sidrón.10
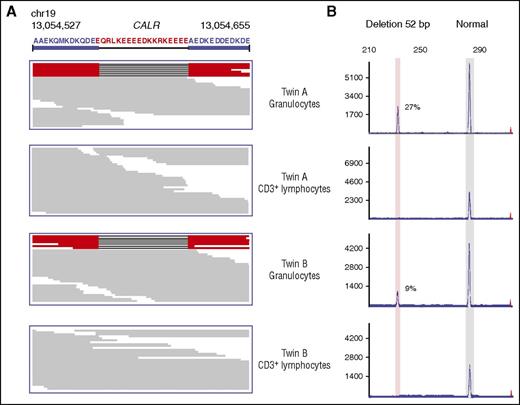
We identified a total of 22 and 20 somatic mutations in twins A and B, respectively, indicating a very low mutation burden (0.006 mutations per Mb), similar to previous studies.5 Interestingly, the only coding mutation identified was the previously described 52-bp deletion in CALR (p.L367fs*46), known as type I mutation.5,6 Both twins shared the same mutation, which was further confirmed by fragment analysis using a 5′-fluorescein–labeled primer, resulting in 27% and 9.7% of mutant allele frequency in the granulocyte fraction, and no mutant reads were detected in T cells either by WGS or fragment analysis (Figure 1).
Identification of the type I CALR mutation in the granulocyte fraction of both twins. (A) Results from next-generation sequencing showing the presence of the same 52-bp deletion in the coding region of the CALR gene in DNA obtained from granulocytes but not from CD3+ lymphocytes. (B) DNA fragment analysis using a 5′-fluorescein–labeled primer confirmed the presence of 27% and 9.7% mutant alleles in the granulocyte component in both sisters, while absent in CD3+ lymphocytes.
Identification of the type I CALR mutation in the granulocyte fraction of both twins. (A) Results from next-generation sequencing showing the presence of the same 52-bp deletion in the coding region of the CALR gene in DNA obtained from granulocytes but not from CD3+ lymphocytes. (B) DNA fragment analysis using a 5′-fluorescein–labeled primer confirmed the presence of 27% and 9.7% mutant alleles in the granulocyte component in both sisters, while absent in CD3+ lymphocytes.
To determine whether the MPN clone arose independently or was originated in 1 sister and transferred in utero to the other sister, we polymerase chain reaction amplified and verified by an orthogonal sequencing technique (IonTorrent) all somatic mutations identified by WGS. We verified as somatic 19/22 and 19/20 of the mutations identified by WGS, and comparison of them confirmed that 100% of the verified somatic mutations (19/19) were shared between both patients (Table 1), a fraction highly unlikely to be attributed by chance (P < 10−123). None of these mutations were predicted to have functional consequences with the exception of the one affecting CALR, and all were present in nonconserved regions. These data provide strong evidence for the common origin of both clones, and to our knowledge, represent the first description of an in utero spreading of MPN precursor cells. Although transplacental transfer constitutes the most likely mechanism by which a mutant clone spread in 2 monozygotic twins, it cannot be ruled out a potential origin of the CALR mutation in yolk sac–derived hematopoietic stem cells during the first days of development.
List of somatic mutations identified in granulocytes from both twins
| Chromosome . | Position . | Reference . | Observed . | Mutant allele frequency % . | Closest gene . | |
|---|---|---|---|---|---|---|
| Twin A . | Twin B . | |||||
| 1 | 60 028 846 | C | T | 18.8 | 13.2 | FGGY (intron) |
| 1 | 178 889 445 | C | T | 19.6 | 14.8 | RALGPS2 (3′UTR) |
| 1 | 195 666 189 | T | C | 24.4 | 18.0 | Intergenic |
| 2 | 59 413 647 | C | T | 24.2 | 16.3 | Intergenic |
| 3 | 146 823 333 | G | A | 21.7 | 13.9 | Intergenic |
| 4 | 21 220 824 | T | C | 23.0 | 15.5 | KCNIP4 (intron) |
| 5 | 44 576 207 | T | G | 31.1 | 16.8 | BRCAT107 (>60 kb) |
| 6 | 138 206 013 | C | T | 30.6 | 16.9 | TNFAIP3 (>1 kb) |
| 8 | 36 036 908 | T | C | 16.8 | 11.1 | Intergenic |
| 8 | 138 269 950 | T | C | 24.0 | 16.0 | Intergenic |
| 10 | 67 342 909 | T | A | 23.3 | 14.6 | LINC01515 (intron) |
| 11 | 79 595 399 | T | C | 23.4 | 14.8 | Intergenic |
| 11 | 124 507 473 | C | T | 21.6 | 15.6 | SIAE (intron) |
| 12 | 12 600 820 | G | A | 30.6 | 23.3 | LOH12CR1 (intron) |
| 18 | 14 979 286 | G | T | 26.3 | 19.4 | LINC01443 (>5 kb) |
| 20 | 42 682 983 | C | G | 20.7 | 13.2 | TOX2 (p.A232A) |
| X | 26 322 338 | C | T | 22.6 | 14.7 | MAGEB5 (>90 kb) |
| X | 77 085 754 | G | T | 22.6 | 14.3 | MAGT1 (intron) |
| 19 | 13 054 564 | — | del52bp | 21.3 | 14.1 | CALR (p.L367fs*46) |
| Average | 23.5 | 15.6 | ||||
| Chromosome . | Position . | Reference . | Observed . | Mutant allele frequency % . | Closest gene . | |
|---|---|---|---|---|---|---|
| Twin A . | Twin B . | |||||
| 1 | 60 028 846 | C | T | 18.8 | 13.2 | FGGY (intron) |
| 1 | 178 889 445 | C | T | 19.6 | 14.8 | RALGPS2 (3′UTR) |
| 1 | 195 666 189 | T | C | 24.4 | 18.0 | Intergenic |
| 2 | 59 413 647 | C | T | 24.2 | 16.3 | Intergenic |
| 3 | 146 823 333 | G | A | 21.7 | 13.9 | Intergenic |
| 4 | 21 220 824 | T | C | 23.0 | 15.5 | KCNIP4 (intron) |
| 5 | 44 576 207 | T | G | 31.1 | 16.8 | BRCAT107 (>60 kb) |
| 6 | 138 206 013 | C | T | 30.6 | 16.9 | TNFAIP3 (>1 kb) |
| 8 | 36 036 908 | T | C | 16.8 | 11.1 | Intergenic |
| 8 | 138 269 950 | T | C | 24.0 | 16.0 | Intergenic |
| 10 | 67 342 909 | T | A | 23.3 | 14.6 | LINC01515 (intron) |
| 11 | 79 595 399 | T | C | 23.4 | 14.8 | Intergenic |
| 11 | 124 507 473 | C | T | 21.6 | 15.6 | SIAE (intron) |
| 12 | 12 600 820 | G | A | 30.6 | 23.3 | LOH12CR1 (intron) |
| 18 | 14 979 286 | G | T | 26.3 | 19.4 | LINC01443 (>5 kb) |
| 20 | 42 682 983 | C | G | 20.7 | 13.2 | TOX2 (p.A232A) |
| X | 26 322 338 | C | T | 22.6 | 14.7 | MAGEB5 (>90 kb) |
| X | 77 085 754 | G | T | 22.6 | 14.3 | MAGT1 (intron) |
| 19 | 13 054 564 | — | del52bp | 21.3 | 14.1 | CALR (p.L367fs*46) |
| Average | 23.5 | 15.6 | ||||
UTR, untranslated region.
The fact that both twins were born with a CALR p.L367fs*46 mutated clone, but no symptoms were observed for >16 years, provides new insights into the biology of MPNs. Thus, it shows that a MPN precursor hematopoietic stem cell clone can be present in the bone marrow for almost 2 decades before disease manifestation. So far, only prenatal acute lymphoblastic leukemia or acute myeloid leukemia precursor mutated HSCs had been described, resulting in a very fast disease progression in months or a few years from birth.11-13
The growth of the same MPN clone in 2 independent bodies for 16 years provides an excellent opportunity to identify additional mutations that could have contributed to disease progression. However, after sequencing at high coverage (>10 000×) all amplicons containing somatic mutations identified in either granulocyte fraction as clonal or subclonal (up to 50% of neoplastic cells), we were unable to detect any differential mutation between samples. This suggests that MPN cells have been extremely stable during this time, as only the initial somatic mutations originated in utero could be found after 16 years of development. This confirms a very low mutational activity of these cells that might explain the low mutational burden observed in MPN in this study and others.5,6 Nevertheless, errors during DNA replication might have resulted in novel mutations in transferred MPN cells. These mutations should be detectable as clonal or subclonal in the blood of the recipient twin if the number of transferred cells was low. As we were unable to identify specific mutations for each individual, this suggests that the number of MPN precursor cells transferred in utero was sufficiently large. Therefore, any individual de novo mutation would have been effectively diluted in the pool of neoplastic cells, making them undetectable by WGS of pooled cells. In any case, the absence of additional mutations, including structural variants or copy number alterations, confirms that the mutation in CALR is sufficient to develop ET.14
However, the factors influencing the latency of the disease are still unknown. Our results rule out genetic alterations as a mechanism involved in latency, as no additional mutations could be detected in any of the clonal cells evolving independently for >16 years. These data provide a basis for further studies aimed at identifying factors influencing disease latency, including epigenetic alterations or the influence of the microenvironment. These studies might lead to a better understanding of MPN evolution, as well as potential strategies to prevent or delay disease development. The recent finding of JAK2 mutations in umbilical cord hematopoietic stem cells15 might underestimate the number of MPN cases originated in utero. In addition, the finding that transplacental transfer can occur in myeloproliferative diseases is also relevant when a twin is diagnosed with this pathology at an early age, suggesting that examination of the other twin might result in an early diagnosis, facilitating a close surveillance of patient evolution.
Authorship
Acknowledgments: This work was supported by a grant from the Spanish Ministry of Economy and Competitiveness (SAF2013-45836-R). R.V.-M. and J.G.-A. are supported by fellowships from the Spanish Ministry of Education. The authors thank Fundación Caja Rural de Asturias for financial collaborative support to Laboratorio de Oncología Molecular (HUCA). The Instituto Universitario de Oncología is supported by Fundación Bancaria Caja de Ahorros de Asturias, Spain. The authors are also very grateful to the patients who have participated in this study.
Contribution: R.V.-M. and J.G.-A. performed the analysis of somatic and germ-line mutation; A.S.P., D.A.P., and I.S. processed samples and performed validation analysis; S.M.L. contributed to sample collection and clinical annotation; and M.B. and X.S.P. designed the study and prepared the final manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Xose S. Puente, Departamento de Bioquímica y Biología Molecular, Facultad de Medicina, Universidad de Oviedo, C/ Fernando Bongera s/n, 33006 Oviedo, Spain; e-mail: xspuente@uniovi.es; and Milagros Balbín, Laboratorio de Oncología Molecular, Hospital Universitario Central de Asturias, C/ Roma s/n, 33011 Oviedo, Spain; e-mail: mbalbin@hca.es.
References
Author notes
R.V.-M. and J.G.-A. contributed equally to this study.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal