Abstract

Despite recent advances, treatment of elderly patients with AML remains a challenge because of adverse disease biology, comorbidities and therapy related toxicities. The balance between effectivity and toxicity of treatment strategies play a key role. Since comparative studies are lacking, a prospective randomized trial was designed among German AML study groups with different treatment strategies to compare outcome.
Patients ≥60 years with all AML subtypes except M3 were randomized up-front to a common standard arm (CSA) (10%) and to study specific arms (90%) of the AMLCG or the OSHO. The CSA consisted of one or two inductions of araC 100 mg/m2/d continuous IV (CI) d 1-7 d and daunorubicin (dauno) 60 mg/m2/d IV d 3, 4, 5 and two courses of araC 1 g/m2/d BID IV d 1, 3 and 5 as consolidation (Mayer RJ et al, NEJM 1994). The AMLCG study arm randomized TAD (araC 100 mg/m2/d CI d1-2 followed by BID d 3-8, dauno 60 mg/m2/d IV d 3-5 and 6-thioguanine 100 mg/m2/d po BID d 3-9) and HAM [araC 1 mg/m2/d IV BID d 1-3 and mitoxantrone (mito) 10 mg/m2/d IV d 3-5] versus two courses of HAM with any 2nd course only given if blasts persisted ± G-CSF. Two courses of TAD were given as consolidation followed by maintenance chemotherapy over three years. The OSHO study arm included araC 1 g/m²/d BID IV d 1 + 3 + 5 + 7 and mito 10 mg/m2/d IV d 1 - 3 for one or two induction courses and ara-C 500 mg/m² BID 1h IV d 1 + 3 + 5 in combination with mito10 mg/m2/d IV d 1 + 2 as consolidation. Pegfilgrastim 6 mg s.c. was applied on day 10 of induction and on d 8 of consolidation. The study was approved by the IRB and registered at clinicaltrials.gov (NCT01497002 and NCT00266136). Written informed consent was obtained from all patients prior to randomization.
Between April 1st, 2005 and May 26th, 2015 1286 patients were assigned randomly to the CSA (n=132) or to the study groups arm (n=1154). After excluding 139 patients (10.8%), 1147 patients were eligible for analysis, 1120 with follow-up for overall survival (OS) and 1079 for complete remission (CR) analysis. Baseline characteristics of all eligible patients showed median ages of 68 (60-82) years for the CSA and 69 (60-87) and 70 (60-85) years in the study arms A and B, respectively (p=0.05). Proportions of patients with secondary AML differed significantly between study arms (A: 42%, B: 30%, CSA: 36%; p=0.003). The CSA had less flt3 wildtype/npm1 wildtype patients (31%) vs. arm A (51% p=0.040) and arm B (58%, p=0.0455). No differences were observed with respect to cytogenetic risk groups, white blood cell counts, LDH, and npm1 mutant/ flt3-wildtype or mutant.
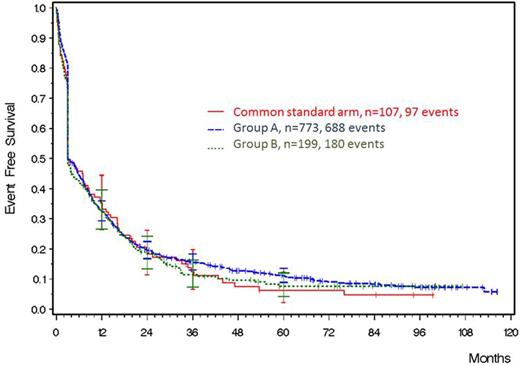
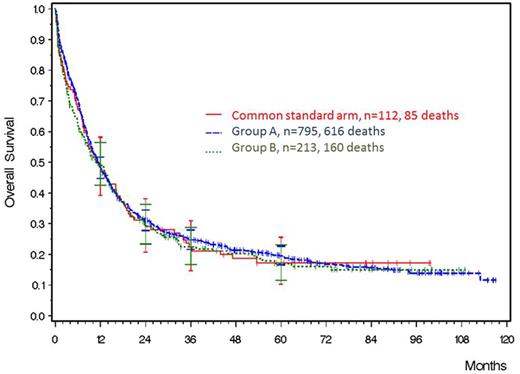
The primary endpoint event free survival (EFS) did not differ between the CSA and study group strategies. Three-year EFS was 12.4% (95% CI: 6.7 - 19.9%) in the CSA, 15.6% (95% CI: 13.1 - 18.3%) in group A and 11.4% (95% CI, 7.4% to 16.4%) in group B (n.s.;Fig.1). With a median follow-up of 67 months, OS did not differ significantly between CSA and study group regimens. The 3-year survival probability was 22.3% (95% CI: 14.7-30.9%) in the CSA, 24.7% (95% CI: 21.6-27.9%) in group A and 22.4% (95% CI, 16.7% - 18.3%) in group B (Fig.2).
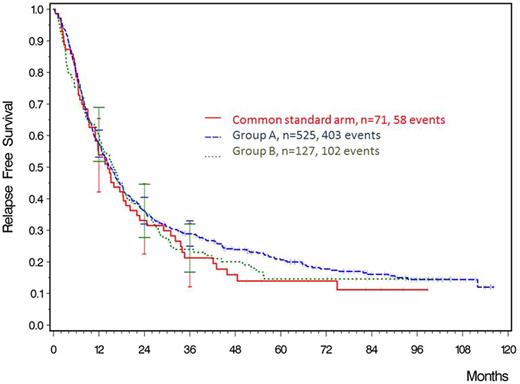
CR status after 90 days of therapy was evaluated as secondary endpoint. The proportion of patients in CR in the CSA [51% (95% CI: 42-61%)] was comparable to the 50% (95% CI: 47-54%) and 48% (95% CI: 41-55%) of the study group arms (p=n.s.). Persistent leukemia was seen in 16% (95% CI: 10-24%) in the CSA vs 17% (95% CI: 14-19%) and 12% (95% CI: 8-17%) in groups A and B, respectively (both p= n.s.). A total of 226 patients died within 90 days of treatment, 24% (95% CI: 17-33%) in CSA, 19% in group A (95% CI: 16-22%) and 27% (95% CI: 21-33%) in group B; CSA vs A p=0.1859, CSA vs B p=0.5902). Death without AML was 3% in CSA, 2% in group A and 3% in group B, death with AML was 9% in CSA, 6% in group A and 5% in group B and death from indeterminate cause was 12% in CSA, 11% in group A and 20% in group B. Three-year relapse free survival (RFS) was 21.3% (95% CI: 12.2 - 31.0) in the CSA, 28.9% (95% CI: 24.9 -33.0%) in group A and 24.0% (95% CI: 16.8 - 31.9) in group B (both p=n.s.; Fig.3).
In multivariate analysis independent variables for EFS and OS were age, type of disease, cytogenetic group and WBC count, but not the allocation to one of the treatment arms. Age and cytogenetic group were determinants for RFS.
Conclusion
A strictly prospective comparison of different treatment strategies in patients with AML did not show clinically relevant outcome differences when compared to a common standard arm.
Niederwieser:Novartis Oncology Europe: Research Funding, Speakers Bureau; Amgen: Speakers Bureau. Hoffmann:Novartis Oncology Europe: Research Funding. Al-Ali:Celgene: Consultancy, Honoraria, Research Funding; Novartis: Consultancy, Honoraria, Research Funding. Hegenbart:Pfizer: Other: Travel grant; Janssen: Honoraria, Other: Travel grant. Sayer:Riemser Pharma: Consultancy. Hochhaus:BMS: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Pfizer: Honoraria, Research Funding; ARIAD: Honoraria, Research Funding. Fischer:Novartis: Consultancy, Honoraria. Dreger:Novartis: Consultancy; Janssen: Consultancy; Gilead: Consultancy; Gilead: Speakers Bureau; Roche: Consultancy; Novartis: Speakers Bureau. Hiddemann:Roche: Membership on an entity's Board of Directors or advisory committees; Genentech: Other: Grants; Roche: Other: Grants.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal