Abstract

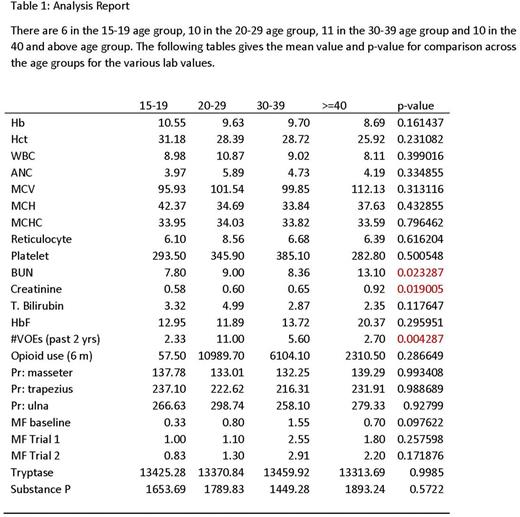
Vaso-occlusive episodes (VOE), are the most common cause of health care encounters and are considered to be a hallmark of sickle cell disease (SCD). It has been increasingly recognized that many SCD patients, especially adults experience daily chronic pain (PiSCES study). While adolescents and young adults experience mostly acute episodic nociceptive pain, a significant number of adults develop chronic neuropathic and centralized pain. Although the precise mechanisms underlying this age-related transition in pain phenotype are not clearly understood, some factors that contribute to this phenomenon include chronic inflammation, organ damage and opioid induced hyperalgesia. Vincent et al (Blood, 2013) showed that mast cell activation is an important contributor to neurogenic inflammation and chronic pain in a mouse model of SCD. In an observational translational study, we recently reported that SCD patients with chronic pain (those who report pain >50% of time) were older and had higher levels of mast cell activation markers, plasma tryptase and substance P, compared to SCD patients who did not have chronic pain (Kuei et al, Blood, 2015). We report here the results of a prospective study of SCD patients (SS and Sβ0 thal) in different age groups. We tested the hypotheses that i) evolution to chronic pain is an age-dependent phenomenon, with higher frequency in older subjects, and ii) serum tryptase and substance P levels can be used as markers of chronic pain. A total of 36 subjects with SCD from the patient population of Pediatric and Adult sickle cell clinics of the MCG Sickle Cell Center were enrolled; these included 6 subjects aged 15-19, and 10 adults each in the age groups of 20-29, 30-39, and ≥40, respectively. Informed consent was obtained. Information on the frequency of VOEs (hospitalizations and ED visits) in the last 2 years, presence of chronic pain, hydroxyurea (HU) exposure, opioid usage as morphine equivalents within the past year, CBC, retics, CMP and % Hb F were collected. Quantitative sensory testing (QST) was performed using three different modalities: pressure pain sensitivity using a hand held computerized algometer AlgoMed, Medoc, Israel); heat and cold sensitivity (Q-Sense, Medoc, Israel); and Von Frey monofilament for neuropathic pain. Plasma tryptase and substance P levels were assayed by ELISA using kits from Biomatik inc, and Enzo Life Sciences, respectively.
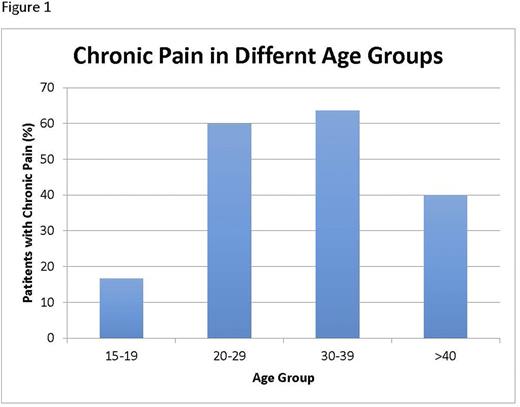
The results (lab tests, QST, VOEs, HU usage, plasma tryptase and substance P levels) are summarized in Table 1. Overall, there was an age dependent increase in the frequency of subjects with chronic pain; while 16.7% of patients in the 15-19 age group experienced chronic pain, this increased to 60.0% in the 20-29 year olds, and to 63.6% in those 30-39 years of age as shown in Figure 1. Among patients ≥40 years, 40.0% reported experiencing chronic pain. VOE frequency (average of last 2 years) was highest in the 20-29 age group (11.0/year) followed by 5.6 in the 30-39 age group. It was 2.57/year among 15-19 year olds, and 2.70/year in patients ≥40 years (p=0.004). Although Hb F and MCV was highest among ≥40 group (20.4%, and 112.1 fl, respectively), this did not reach statistical significance. As seen in the Table, BUN and creatinine showed a significant age dependent increase indicative of progressive organ damage. There was no significant difference between different age groups in other laboratory parameters, QST results, and plasma tryptase and substance P levels. The significant finding of this study is the higher frequency of VOEs in the 20-39 age group, compared to adolescents and patients 40 years and above. Although this finding is paralleled by a trend in opioid use, and frequency of chronic pain, these did not reach statistical significance in this relatively small group. The other interesting observation is the relatively mild course of disease in those ≥40 years of age (lower frequency of chronic pain, lower opioid use, lower VOE frequency). This seemingly paradoxical finding can be explained either by a survival advantage of the relatively mild patients, or a better adherence to HU, as suggested by higher MCV and Hb F in this group. The transition from adolescence to young adulthood is associated with a higher morbidity in SCD. Factors contributing to this phenomenon should be studied in a larger cohort.
Kutlar:Novartis Pharmaceuticals: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal