Abstract

Background
The role of thromboprophylaxis in solid organ malignancies is well established. Hematologic malignancies can also be associated with a considerable risk of thromboembolic complications. The incidence of these events is variable and is influenced by multiple factors. Limited data are available regarding the incidence of venous thromboembolism (VTE) in hospitalized acute leukemia (AL) patients. The management of symptomatic VTE in patients with AL can be challenging due to the increased risk of thrombocytopenia-related bleeding.
Methods
The Discharge summary Database (DAD) was used to extract post-admitted PE and DVT volumes in AL patients admitted to Princess Margaret Cancer Centre from 2007-2016. ICD-10-CA diagnosis codes for acute leukemia, and both PE and DVT events, were used. Only patients diagnosed with VTE at least 48 hours post-admission were included to restrict the cohort to patients that developed VTE during their admission.
Results
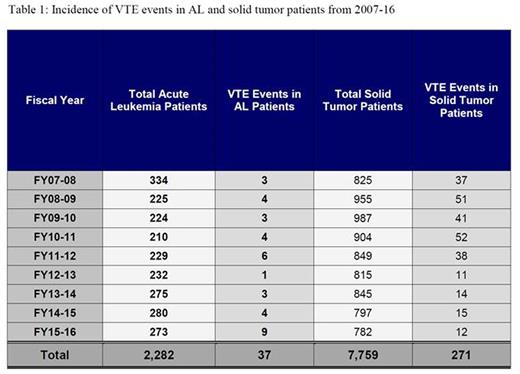
We analyzed a total of 10,041 patients that were admitted to Princess Margaret Cancer Centre during the 2007-2016 period. (Table 1) Of these, 7759 had a solid tumor diagnosis (271 VTE events, 3.4%) and 2282 patients had AL (1675 AML, 464 ALL, 144 APL). The AL patients (AML, ALL, APL) admitted to our Centre for chemotherapy or for the management of complications were further evaluated to determine VTE incidence and to evaluate its management in this setting. As of September 2012, patients with solid tumors treated at our Centre received standard thromboprophylaxis as part of an institutional in-patient (VTE) prophylaxis policy (IPP) that reduced the incidence of VTE from 4.8% (219/4520) to 1.6% (3239/52) before and after the policy was initiated, respectively. AL patients are not given prophylactic anticoagulation. 37 AL patients (22 AML, 10 ALL, and 5 APL; overall incidence 1.6%) developed symptomatic VTE (DVT only 23, PE only 8, DVT + PE 6). VTE was reported as central venous catheter related in 12/37 patients (32.4%). PE was detected in all cases by CT-PE. Median age of VTE patients was 53 years (range 32-77), with a median hospital stay of 35 days (range 2-144). Chemotherapy was given to 26 of the 37 patients that developed VTE, with 20 receiving initial induction chemotherapy. 17/37 (46%) patients had PLT<50.000/mm3 at VTE diagnosis. Full dose low molecular weight heparin with platelet transfusion support was used to treat 35/37 patients with acute VTE during the first month of treatment. 2/37 did not receive anticoagulation due to ongoing active bleeding. None of the treated patients experienced major bleeding.
Conclusions
In our experience, the incidence of VTE in AL patients during prolonged hospital stay is relatively low, raising questions about the need for routine VTE prophylaxis in this group. The relatively increased risk of VTE in AL patients receiving chemotherapy (particularly, induction chemotherapy), should prompt particular scrutiny in symptomatic patients.
Schuh:Amgen: Membership on an entity's Board of Directors or advisory committees. Yee:Novartis Canada: Membership on an entity's Board of Directors or advisory committees, Research Funding. Gupta:Incyte Corporation: Consultancy, Research Funding; Novartis: Consultancy, Honoraria, Research Funding. Schimmer:Novartis: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal