Abstract
Introduction:
Renal insufficiency (RI) in newly diagnosed multiple myeloma (NDMM) represents a poor prognostic factor (Knudsen, Hjorth, and Hippe 2000). Recent clinical trials have demonstrated that patients treated with novel agents, particularly proteasome inhibitors, may experience renal recovery with improvement in overall survival (Dimopoulos et al. 2013; Gonsalves et al. 2015). The majority of patients in these trials were Caucasians, although multiple myeloma is twice as common in African Americans (AA) as it is in Caucasians. Moreover, AA have a 5 times higher rate of stage 4 chronic kidney disease (CKD) and end-stage-renal-disease (ESRD) in the United States compared to Caucasians. The cause for this disparity is thought to be multifactorial, including a higher incidence of comorbidities such as diabetes and hypertension among AAs (Williams and Pollak 2013; Grams et al. 2013). There is currently a dearth of evidence regarding renal recovery in AA receiving therapy for MM. The goal of this study is to compare renal recovery between AA and non AA patients following initial treatment for NDMM.
Methods:
We performed a retrospective chart review of patients with NDMM at Rush University Medical Center from January 1, 2005 to August 1, 2016. 690 charts were selected and reviewed; patients who were on hemodialysis for alternative reasons prior to diagnosis, had a GFR > 90, or for whom records were incomplete were excluded. 118 patients with NDMM and a GFR < 90 (corresponding to National Kidney Foundation's chronic kidney disease stage 2 or worse) at the time of diagnosis were identified. Continuous variables were compared between the two groups using the Mann-Whitney U test, and binary variables were compared using Fisher's exact test.
Results:
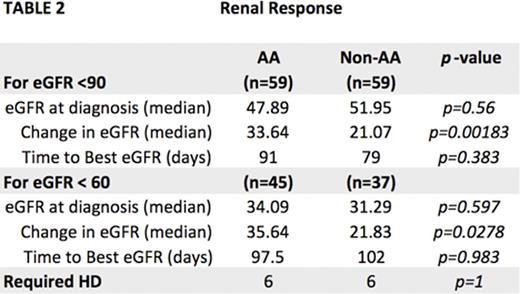
We compared 59 AA and 59 non AA patients with RI at the time of diagnosis of MM. Both groups were comparable by age, gender, ISS and high risk cytogenetics. The degree of RI at the time of diagnosis was similar: median GFR at diagnosis was 47.89 in the AA group and 51.95 in the non AA group (p=0.56). Hypertension was more common in the AA group (78% vs. 52.5%, p=0.0064), while other comorbidities were statistically comparable.
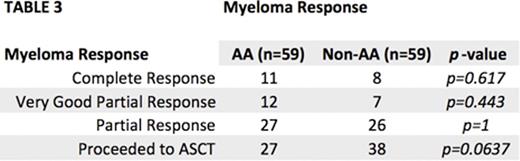
The majority of patients were treated with a bortezomib-based regimen (86.4% for the AA group and 84.7% for the non AA group, p=1). MM response rates to induction therapy were similar: very good partial response (VGPR) or better was achieved in 39% of AA and 25.4% of non AA (p=0.17). 45.8% of AA patients underwent autologous stem cell transplant (ASCT) compared to 64.4% of non-AA (p=0.0637, see table 3). 80% of AA and 88% of non AA patients received bisphosphonates (see table 1).
Although median GFR at the time of diagnosis of MM was similar between the AA and non AA groups (47.89 vs. 51.95, p=0.56), the median absolute change in estimated GFR after initial therapy was significantly higher in the AA group (+33.64) vs. the non-AA group (+21.07, p=0.00183). This difference remained whether the baseline GFR at diagnosis was <90 or <60 (see table 2). The median time to best renal response was 91 days in AA and 79 days in non-AA (p=0.383).
Conclusions:
This is the first study to analyze disparities in renal dysfunction and recovery between AA and non-AA patients with NDMM. We demonstrate that in our institution AA patients with NDMM treated in the era of novel agents have greater improvement in renal function in comparison to non AA patients. Given that renal recovery in NDMM impacts overall survival, this finding suggests that further studies should be done to explore differences in the epidemiology and disease biology that could account for the racial disparities in renal dysfunction and recovery.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal