Abstract
Allogeneic hematopoietic stem cell transplantation (HSCT) can be a curative therapeutic option for patients with myelodysplastic syndromes (MDSs). However, the role of allogeneic HSCT is still controversial for older MDS patients.
Here we report the post-transplant outcomes in 88 older MDS patients (≥ 60 years) that were transplanted at MD Anderson Cancer Center with reduced intensity conditioning (RIC) from 2005 through 2015. In this cohort, the conditioning regimen were 1) intravenous busulfan in a dose calculated to target an average daily systemic exposure, represented by the area under the concentration versus time curve (AUC) of 4000 μMol-min ± 10% or 100 mg/m2 in combination with fludarabine 40 mg/m2 for 4 days or 2) melphalan 100-140 mg/m2 as a single dose with fludarabine 40 mg/m2 for 4 days. Donors were HLA matched related (MRD, n=48), matched unrelated (MUD, n=30) and haploidentical (n=10). Graft versus host disease (GVHD) prophylaxis in MRD and MUD recipients was tacrolimus (0.015 mg/kg) and methotrexate (5 mg/m2, 1,3,6,11 days). MUD recipients also received anti-thymocyte globulin (ATG) (4 mg/kg, in divided doses given on days -3, -2,-1) for GVHD prophylaxis. Post-transplant cyclophosphamide (50 mg/kg, 3-4 days), tacrolimus (0.015 mg/kg) and mycophenolate mofetil (MMF) (15 mg/kg) were used for GVHD prophylaxis in haploidentical donors.
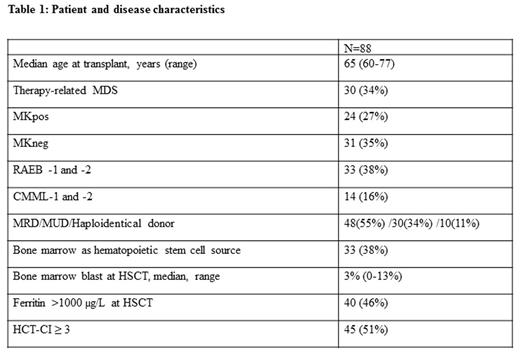
The median age was 65 (range, 60-77, Table 1). The study cohort had high-risk features including 30 patients (34%) with therapy-related MDS (tx-MDS) and 24 (27%) with monosomal karyotype-positive (MKpos) defined by Breems et al. Histological subtype at diagnosis was RAEB-1 and -2 in 33 (38%) and CMML in 14 (16%) patients. Hematopoietic stem cell comorbidity index (HCT-CI) was ≥3 in 45 (51%) patients. The median bone marrow blast count at HSCT was 3% (range, 0%-13%) in 87 patients.
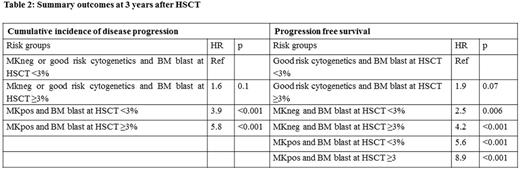
The median follow up of 36 survivors was 32 months (range, 6-98). Overall survival (OS), cumulative incidence of progression and transplant-related mortality (TRM) at 3 years was 41%, 26% and 35% respectively as presented in Table 2.
Univariate analyses using Cox's proportional hazards regression analysis showed that MKpos was the only prognostic factor for the cumulative incidence of progression. MKpos patients had higher incidence of progression compared with patient with good risk cytogenetics (including normal karyotype (n=23) and del(5q), del(12p), del(20q) (n=4)) (HR=9.5, 95% CI, 2.2-41, p=0.003) and with MKneg (HR= 3.3, 95% CI, 1.3-8.6, p=0.01). There was no significant difference between MKneg and CN (p=0.2). The univariate analyses showed that MKpos, MKneg, higher serum ferritin level at HSCT and HCT-CI≥3 were associated with inferior OS. Blast count at HSCT and age>65 were associated with worse survival but did not reach statistical significance.
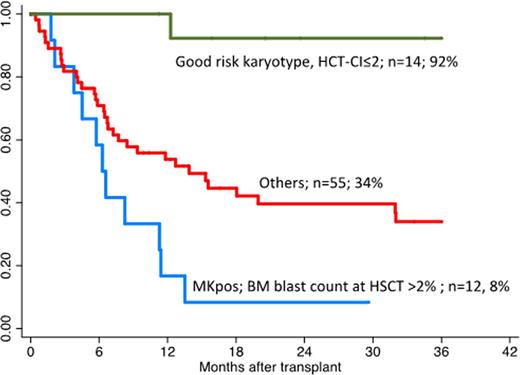
For multivariate analyses, we performed classification and regression tree (CART) analyses that enabled us to identify 3 risk groups for OS: 1) Poor risk group including patients with MKpos and BM blast >2% (n=12) with 3 year OS of 8%, 2) Good risk group including good risk cytogenetics with HCT-CI≤2 (n=14) with 3-year OS of 92%, and 3) intermediate risk group including rest of the group (n=55) with 3-year OS of 34% (Figure 1).
In conclusion, our results show that allogeneic HSCT with RIC is a feasible option in older MDS patients with OS of 41% at 3-years. Results are best in patients with low HCT-CI and good risk cytogenetics. TRM and disease progression remain major causes of failure and innovative strategies with better disease control while not increasing TRM are urgently needed in this cohort.
Overall survival by risk groups in older MDS patients after HSCT with RIC
ADDIN
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal