Abstract
Introduction
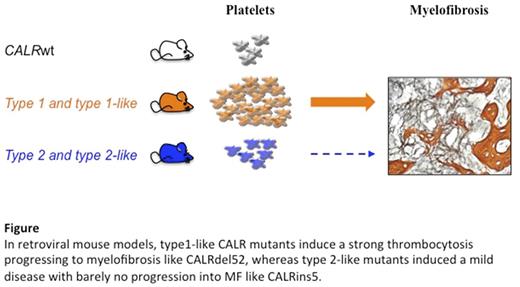
The acquisition of somatic mutations in the hematopoietic stem cell (HSC) compartment leading to the constitutive activation of the JAK-STAT signaling pathway drives the development of myeloproliferative neoplasms (MPNs). After the gain-of-function mutation JAK2 V617F, the second most frequent driver mutations inducing 30% of essential thrombocythemia and mylofibrosis (MF) are located in the calreticulin (CALR) gene. The two most frequent CALR mutations are a deletion of 52 base pairs (del52) L367fs*46 also called type 1 and an insertion of 5 base pairs (ins5) K385fs*47 or type 2. They represent together more than 80% of all CALR mutations. In retroviral mouse models CALR mutants induce a thrombocytosis, but to a lesser extent in presence of ins5 compared to del52. Moreover, del52 mice evolved more frequently into MF than ins5 mice, mimicking what is observed in patients. Many other rare mutations of CALR exist and each represents less than 2% of CALR mutations in patients. They are structurally classified as type 1- and type 2-like CALR mutations according to the absence or presence of a residual wild-type calcium-binding motif and the modification of the alpha helix structure but it is not known whether they are equally functionally related to CALRdel52 and CALRins5, respectively.
Material and Methods
We modeled two type 1-like mutations, del34 (E369fs*50) and del46 (L367fs*48) and of one type 2-like mutation del19 (K374fs*50) in cell lines and in mice by bone marrow transplantation after retroviral transduction with CALR mutation constructs.
Result
In Ba/F3 cell lines, all CALR mutants specifically activated cytokine-independent cell growth in presence of the thrombopoietin (TPO) receptor (MPL) with close efficiency, and induced a constitutive activation of JAK2 and STAT5/3/1 in a similar way.
Lethally irradiated mice that were engrafted with bone marrow transduced with the wild-type (CALR wt) or the different CALR mutations developed pure thrombocytosis but to a much lesser extent in presence of type 2 and type 2-like CALR mutations. The thrombocytosis was associated with megakaryocyte hyperplasia in the bone marrow and in the spleen seen by Von Willebrand factor immunostaining and flow cytometry. In contrast to type 2-like mice, type 1-like mice developed a MF after 10 months of engraftment associated with splenomegaly, a marked osteogenesis in bone marrow and a thickening of reticulin fiber network seen in histology.
Like observed for type 1 mutant, type 1-like CALR mutations induced an expansion at early stage of hematopoiesis compare to type 2 and type 2-like mutations with a significant increased frequency in immature SLAM, LSK and MkP progenitors. Altogether, type 1-like CALR mutants harbor a stronger phenotype than the type 2-like recapitulating thrombocytosis and progression to MF.
Thus, type 1-like and type 2-like CALR mutants structurally and functionally resemble type 1 and type 2, respectively. The mechanisms responsible for these differences remain to be determined and could be related to a MPL independent process.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal