Abstract
Background: Classical Hodgkin lymphoma (cHL) displays near-universal genetic deregulation of PD-1 ligand expression, and relapsed/refractory (R/R) cHL is uniquely sensitive to PD-1 blockade. However, such treatment for patients (pts) who relapse after or are ineligible for autologous stem cell transplantation (ASCT) appears to be rarely, if ever, curative. Deploying PD-1 blockade early after ASCT could leverage the remodeling immune landscape and minimal residual disease state to increase the cure rate of ASCT. We therefore conducted a phase 2 multi-center single-arm study of the anti-PD-1 monoclonal antibody pembrolizumab (pembro) in pts with chemosensitive R/R cHL after ASCT. Another arm of this study enrolled pts with R/R DLBCL and will be presented separately.
Methods: Adult pts with R/R cHL who had received 2-3 lines of prior therapy and ASCT and who were chemosensitive prior to ASCT were enrolled on this study. In addition to meeting standard eligibility criteria for pembro treatment, pts had to have recovered from ASCT toxicities and begin study treatment within 60 days of stem cell infusion (goal within 21 days). They received pembro 200mg IV every 3 weeks for 8 cycles. PET-CT scans were obtained at post-ASCT baseline, after 3 and 7 cycles, then at 12 and 18 months post-ASCT. The primary endpoint was the progression-free survival rate (PFS) at 18 months after ASCT, assessed using International Harmonization Project 2007 criteria.
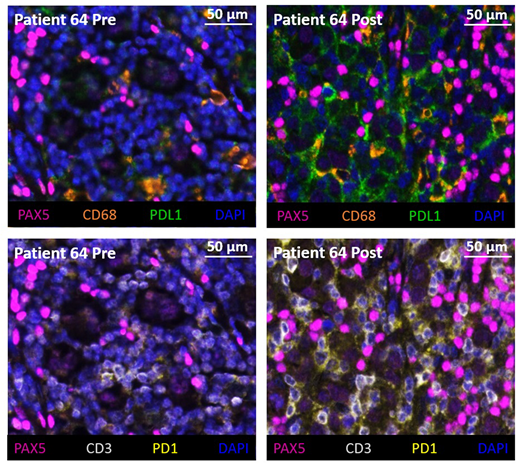
Results: 31 pts were enrolled and 1 withdrew consent before starting treatment. Among the 30 eligible patients, median age was 33 (20-69). 26 pts (87%) were high-risk by virtue of primary refractory disease (57%), relapse within 12 months (17%), extranodal disease at relapse (27%) or absence of metabolic CR at ASCT (10%). At study baseline post-ASCT, 97% were in CR. 24 pts (80%) completed 8 cycles of pembro per protocol. 6 pts (20%) stopped pembro early for pt choice (n=2, including 1 pt with gr2 pneumonitis) or toxicity (n=4, including 2 pts with gr3 hepatitis, 1 with g3 pneumonitis, 1 with g2 diplopia). 9 pts (30%) experienced a total of 28 gr3 or higher adverse events (AEs). The most common gr4 AE was neutropenia (10%). 3 patients (10%) experienced 7 gr3-4 AEs at least probably related to pembro (gr3 diarrhea and gr3 eosinophilic colitis in 1 pt, gr3 leukopenia and gr4 neutropenia in 1 pt, gr3 leukopenia and gr3 ALT and AST elevation in 1 pt). 11 pts (37%) experienced at least one immune-related AE of gr2 or higher severity: pneumonitis (n=2 gr2, n=1 gr3), thyroid dysfunction (n=1 gr2), transaminitis (n=2 gr3), colitis/diarrhea (n=1 gr2, n=2 gr3), rash (n=2 gr2), pulmonary hemorrhage (n=1 gr3), arthritis (n=1 gr2), and increased creatinine (n=1 gr2). There was no treatment-related death. Among the 30 eligible pts, 2 were lost to follow-up after their 12m assessments (both in CR). 27 pts (90%) were evaluable for the primary endpoint (the last pt is still in follow-up and results will be updated for the meeting). 6 patients (20%) relapsed at a median of 8 months (3-18) from ASCT, and all other evaluable patients were in CR at the 18m timepoint. The KM estimate of 18m PFS for high-risk patients was 78% (95%CI 54-91). The 18m overall survival was 100%. Tumor biopsies from a pt who progressed on study demonstrated an increase in the %age of PD1+ T cells at progression, as well as an increase in the %age of PD-L1+ macrophages and PD-L1+ Reed-Sternberg cells (Figure). Other correlative studies including immune reconstitution and MRD analyses are ongoing.
Conclusions: Pembrolizumab administered after ASCT in patients with R/R cHL has a safety profile that appears similar to its use in the R/R setting, although possibly with a higher rate of neutropenia. The 18-month progression-free rate in this high-risk cohort compares favorably with previous published studies, and supports the hypothesis that PD-1 blockade in this setting may increase the efficacy of ASCT. This should be tested in a randomized trial.
Armand:Pfizer: Consultancy; Affimed: Consultancy, Research Funding; Otsuka: Research Funding; Merck: Consultancy, Research Funding; Infinity: Consultancy; Adaptive: Research Funding; Bristol-Myers Squibb: Consultancy, Research Funding; Roche: Research Funding; Tensha: Research Funding. Chen:Incyte: Consultancy, Membership on an entity's Board of Directors or advisory committees; Takeda Pharmaceuticals: Consultancy; Magenta Therapeutics: Consultancy; REGiMMUNE: Consultancy. LaCasce:Humanigen: Consultancy, Honoraria; Research to Practice: Speakers Bureau; Bristol-Myers Squibb: Other: Data safety and monitoring board; Seattle Genetics: Consultancy, Honoraria. Jacobson:Pfizer: Consultancy; Humanigen: Consultancy; Precision Bioscience: Consultancy; Novartis: Consultancy; Kite: Consultancy; Bayer: Consultancy. Jacobsen:Merck: Consultancy; Seattle Genetics: Consultancy. Rodig:Bristol-Meyers-Squibb: Research Funding; KITE Pharma: Research Funding; Affimed Inc.: Research Funding; Merck & Co., Inc.: Research Funding. Shipp:AstraZeneca: Honoraria; Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bayer: Research Funding; Merck: Research Funding. Herrera:BMS: Consultancy, Research Funding; Merck: Consultancy, Research Funding; Genentech: Consultancy, Research Funding; Pharmacyclics: Consultancy, Research Funding; KiTE Pharma: Consultancy, Research Funding; Seattle Genetics: Research Funding; Immune Design: Research Funding; Astra Zeneca: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal