Abstract
Older adults represent the growing majority of patients diagnosed with hematologic disorders, yet they remain underrepresented on clinical trials. Older patients of the same chronologic age differ from one another with varying comorbidity and functional reserve. The concepts of frailty and resilience are important to patient-centered care and are patient and setting specific. The use of geriatric assessment to inform tailored decision making and management can personalize care for older adults with hematologic malignancies. This article will highlight available evidence to support the role of geriatric assessment measures to enhance quality of care for older adults diagnosed with hematologic malignancies.
Introduction
Older adults represent the growing majority of patients diagnosed with hematologic malignancies. Despite this, clinical trial evidence is limited for older adults because of their underrepresentation on therapeutic trials and the lack of representativeness of those who are enrolled.1 Providers and patients face challenges when considering treatment and management plans for older patients as a result of the higher prevalence of comorbid conditions, functional impairment (physical and cognitive), polypharmacy, and socioeconomic factors that can influence treatment outcomes.2 Despite a higher prevalence of these conditions with aging, they vary widely among patients of the same chronologic age. Personalized plans for treatment and survivorship are needed that account for the heterogeneity of aging and address patient-centric goals, such as maintenance of independence and quality of life.
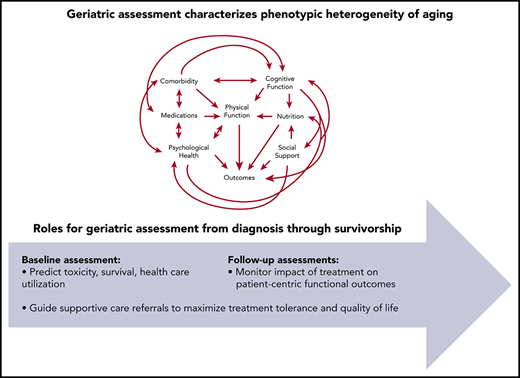
Geriatric assessment is a strategy to provide a multidimensional characterization of an older adult inclusive of the cardinal domains of functional status, physical health, socioenvironmental issues, and psychological health.3 The use of geriatric assessment can inform determination of fitness or frailty. Although “fitness” has no gold standard definition, in practice it may describe an older adult who is potentially robust enough to be treated similarly to a middle-aged patient. Frailty is a state of decreased physiologic reserve associated with adverse health outcomes commonly arising from decreased organ reserve, lack of activity, poor nutritional intake, stress, and/or physiologic changes of aging. In geriatrics, frailty is commonly assessed via a phenotype method (weight loss, weakness, slow gait speed, low physical activity, and exhaustion)4 or through a cumulative deficit burden strategy.5 Importantly, many patients may not meet criteria to be categorized as “fit” or “frail”. Common terminologies to describe these patients include “prefrail,” “unfit,” or “vulnerable.” Adding to the complexity is the fact that these characterizations can be dynamic and can change over time. In addition, the implications of vulnerability or frailty with respect to treatment tolerance differ depending upon the natural history of the hematologic condition and the intensity of the therapies required to treat it.
Accumulating evidence demonstrates the usefulness of geriatric assessment to enhance the prediction of treatment tolerance and benefit among older adults.3,6 Further, information gathered through these assessments can direct management to enhance resilience and mitigate risk. This article will review evidence to support integration of geriatric assessment into care for patients with hematologic malignancy and discuss how this approach can improve quality of care during active treatment and survivorship.
Case vignette
The patient is a 79-year-old woman referred to a hematology clinic with a new diagnosis of stage 3 diffuse large cell lymphoma. She developed symptoms of fatigue and weight loss, prompting a workup by her primary care doctor after noting adenopathy on examination. She presents with her son to discuss treatment. Her son recently read a newspaper editorial that discussed lack of inclusion of older adults on clinical trials. He is concerned about how treatment will be selected for his mother and wants to ensure that she is not undertreated because of her age. He states that “she is a vibrant woman who lives independently. She is doing very well for her age.” The patient adds that she is interested in therapy and is willing to consider all options; however, she worries about taking chemotherapy “at her age” because of its side effects. She emphasizes that maintaining her independence is a priority. She and her son want to know how to estimate her personal risks and benefits of therapy and to discuss strategies to best support her through treatment.
Making the case for using geriatric assessment to personalize care
Geriatric assessment detects unrecognized vulnerabilities
Multiple geriatric assessment tools have been evaluated in the hematology setting,7-16 and one was developed specifically for use among patients with hematologic conditions.17,18 Geriatric assessments most commonly assess the domains of physical function, cognitive function, comorbidity, socioeconomic issues, emotional health, polypharmacy, and nutritional status. Screening for geriatric syndromes, such as falls, are also routinely included (Table 1). Regardless of the specific tests used, results are consistent. The use of geriatric assessment can identify vulnerabilities that are otherwise missed across varied disease and treatment settings. A systematic review that evaluated geriatric assessment in hematologic malignancies (median age, 73 years) showed that the prevalence of geriatric impairments was high, despite general good oncology performance status. Among 13 studies with reported data, the median prevalence estimates of geriatric impairments were 26% for activities of daily living (ADLs; range, 8%-59%), 44% for instrumental ADLs (IADLs; range, 21%-81%), 19% for cognitive impairment (range, 0%-38%), 32% for depressive symptoms (range, 19%-94%), and 39% for impaired objective physical capacity (range, 12%-76%).15 Table 2 provides highlights from trials evaluating the utility of geriatric assessment in varied hematologic settings.7,8,10-12,14,19-24 The specific tests used varied to some extent across trials, with physical function and comorbidity most consistently captured.
Parameters commonly included in geriatric assessments
| Parameter . | Assessment/measure (example of screening tools) . |
|---|---|
| Physical function | Self-reported (ie, ADLs, IADLs, mobility questions, such as “Can you walk a block or a quarter mile?”) |
| Objectively measured (ie, walking speed, Timed Up and Go test, Short Physical Performance Battery [gait speed, balance testing, chair stands], grip strength) | |
| Cognitive function | Cognition screens (ie, Mini-Cog, Blessed Orientation Memory Concentration test, 5-word recall, Montreal Cognitive Assessment is used by geriatricians but is a longer test) |
| Capacity assessment | |
| Comorbidity | Total number of conditions |
| Comorbidity burden index (ie, Charlson Comorbidity Index, Cumulative Illness Rating Scale-Geriatric, Hematopoietic Cell Transplantation-Specific Comorbidity Index) | |
| Individual conditions (ie, diabetes, congestive heart failure, chronic obstructive pulmonary disease) | |
| Socioeconomic issues | Social support (ie, caregivers, transportation) |
| Income/financial challenges | |
| Psychological state | Depression (ie, Geriatric Depression Scale, Patient Health Questionnaire-9, Mental Health Inventory) |
| Distress (ie, Distress Thermometer) | |
| Anxiety (ie, Mental Health Inventory) | |
| Geriatric syndromes | Delirium (ie, Confusion Assessment Method) |
| Falls (ie, single-item screen; “How many falls in the past 6 months?”) | |
| Failure to thrive | |
| Polypharmacy | Number of medications (≥4 medications is a common cut-point for polypharmacy) |
| High-risk medications (ie, Beers criteria) | |
| Drug interactions (ie, drug-interaction software) | |
| Nutrition | Weight loss (ie, >10% from baseline) |
| Body mass index | |
| Access to nutritional support | |
| Nutrition screening tool (ie, Mini Nutritional Assessment) |
| Parameter . | Assessment/measure (example of screening tools) . |
|---|---|
| Physical function | Self-reported (ie, ADLs, IADLs, mobility questions, such as “Can you walk a block or a quarter mile?”) |
| Objectively measured (ie, walking speed, Timed Up and Go test, Short Physical Performance Battery [gait speed, balance testing, chair stands], grip strength) | |
| Cognitive function | Cognition screens (ie, Mini-Cog, Blessed Orientation Memory Concentration test, 5-word recall, Montreal Cognitive Assessment is used by geriatricians but is a longer test) |
| Capacity assessment | |
| Comorbidity | Total number of conditions |
| Comorbidity burden index (ie, Charlson Comorbidity Index, Cumulative Illness Rating Scale-Geriatric, Hematopoietic Cell Transplantation-Specific Comorbidity Index) | |
| Individual conditions (ie, diabetes, congestive heart failure, chronic obstructive pulmonary disease) | |
| Socioeconomic issues | Social support (ie, caregivers, transportation) |
| Income/financial challenges | |
| Psychological state | Depression (ie, Geriatric Depression Scale, Patient Health Questionnaire-9, Mental Health Inventory) |
| Distress (ie, Distress Thermometer) | |
| Anxiety (ie, Mental Health Inventory) | |
| Geriatric syndromes | Delirium (ie, Confusion Assessment Method) |
| Falls (ie, single-item screen; “How many falls in the past 6 months?”) | |
| Failure to thrive | |
| Polypharmacy | Number of medications (≥4 medications is a common cut-point for polypharmacy) |
| High-risk medications (ie, Beers criteria) | |
| Drug interactions (ie, drug-interaction software) | |
| Nutrition | Weight loss (ie, >10% from baseline) |
| Body mass index | |
| Access to nutritional support | |
| Nutrition screening tool (ie, Mini Nutritional Assessment) |
Selected trials highlighting prevalence of geriatric impairments among older patients with hematologic malignancies
| Disease type/setting . | No. patients . | ADLs, % . | IADLs, % . | Physical performance, % . | Cognitive, % . | Mood, % . | Comorbidity burden, % . | Nutritional status, % . |
|---|---|---|---|---|---|---|---|---|
| Chronic lymphocytic leukemia8 | 75 | n/a | 19 | 63 | 49 | n/a | 36 | n/a |
| Multiple myeloma10 | 869 | 14 | 18 | n/a | n/a | n/a | 17 | n/a |
| Acute myeloid leukemia20 | 54 | 48 | 41 | 54 | 32 | 39 | 46 | n/a |
| Acute myeloid leukemia/myelodysplastic syndrome7 | 195 | 34 | n/a | 55 | 9 | 14 | n/a | n/a |
| Myelodysplastic syndrome14 | 98 | 29 | 34 | 31 | 11 | 32 | 23 | 27 |
| Myelodysplastic syndrome19 | 455 | n/a | 45 | 35* | n/a | n/a | 58 | n/a |
| Non-Hodgkin lymphoma11 | 84 | 12 | n/a | n/a | n/a | n/a | 50 | n/a |
| Non-Hodgkin lymphoma22 | 143 | 18 | 21 | n/a | n/a | n/a | 56 | n/a |
| Non-Hodgkin lymphoma23 | 70 | n/a | n/a | n/a | 28 | 41 | n/a | 36 |
| Bone marrow transplantation (preallogeneic transplant evaluation, mixed population, age ≥ 50 y)12 | 203 | 7 | 40 | 33 | n/a | 56 | 55 | 58 |
| Bone marrow transplantation (preautologous transplant evaluation, age ≥ 50 y)24 | 184 | n/a | 36 | 15 | 3 | 35 | 33 | n/a |
| Disease type/setting . | No. patients . | ADLs, % . | IADLs, % . | Physical performance, % . | Cognitive, % . | Mood, % . | Comorbidity burden, % . | Nutritional status, % . |
|---|---|---|---|---|---|---|---|---|
| Chronic lymphocytic leukemia8 | 75 | n/a | 19 | 63 | 49 | n/a | 36 | n/a |
| Multiple myeloma10 | 869 | 14 | 18 | n/a | n/a | n/a | 17 | n/a |
| Acute myeloid leukemia20 | 54 | 48 | 41 | 54 | 32 | 39 | 46 | n/a |
| Acute myeloid leukemia/myelodysplastic syndrome7 | 195 | 34 | n/a | 55 | 9 | 14 | n/a | n/a |
| Myelodysplastic syndrome14 | 98 | 29 | 34 | 31 | 11 | 32 | 23 | 27 |
| Myelodysplastic syndrome19 | 455 | n/a | 45 | 35* | n/a | n/a | 58 | n/a |
| Non-Hodgkin lymphoma11 | 84 | 12 | n/a | n/a | n/a | n/a | 50 | n/a |
| Non-Hodgkin lymphoma22 | 143 | 18 | 21 | n/a | n/a | n/a | 56 | n/a |
| Non-Hodgkin lymphoma23 | 70 | n/a | n/a | n/a | 28 | 41 | n/a | 36 |
| Bone marrow transplantation (preallogeneic transplant evaluation, mixed population, age ≥ 50 y)12 | 203 | 7 | 40 | 33 | n/a | 56 | 55 | 58 |
| Bone marrow transplantation (preautologous transplant evaluation, age ≥ 50 y)24 | 184 | n/a | 36 | 15 | 3 | 35 | 33 | n/a |
Tests and thresholds for impairment varied for physical performance, cognitive function, mood, comorbidity burden, and nutritional status.
n/a, not assessed or reported.
Prevalence estimate refers to gait speed < 4.82 seconds.
Geriatric assessment measures clearly provide clinical information that should meaningfully inform care. These assessments are feasible to perform because most tests are self-administered by the patient and are low cost.17,20,25 The use of geriatric assessment is not limited to academic centers, because evidence has shown it to be feasible in community oncology clinics as well.26 A high-yield low-cost assessment strategy to address the heterogeneity inherent with chronologic aging provides a foundation upon which to discuss the role of geriatric assessment to enhance quality of care.
Case continued
The patient and her son are informed that that the survey she filled out asking questions about her symptoms, functional capacity, mood, and support will help to guide discussions and treatment planning. In addition, assessing her memory and mobility as part of her examination provides further information to help estimate resilience during treatment. The results of her geriatric assessment are as follows: independent in basic ADLs and IADLs, gait speed is brisk (4-meter walk in 3.8 seconds), negative screen for cognitive impairment, no depressive symptoms, no major comorbid conditions, no falls, and has excellent social support. She reports a 10-pound weight loss in the past months. She was exercising regularly until the past few weeks. The patient and her provider discuss results in the context of her diagnosis and treatment options. Her results suggest that she is a robust 79-year-old with her primary symptom attributable to her disease. She is interested in the implications of these data on outcomes.
Geriatric assessment can inform treatment tolerance
Predicting the risk of toxicity or tolerance to therapy for older adults is challenging, yet it is a key component of informed treatment decision making. Physicians and patients are often using data extrapolated from younger patients in clinical trials that do not adequately reflect the treatment experience of an older and potentially vulnerable or frail patient. Multiple studies have demonstrated the utility of geriatric assessment to predict treatment toxicity for older adults with cancer.27,28 In some studies evaluating hematologic malignancies, geriatric assessment measures have been independently associated with treatment toxicity.15 For example, in 869 older myeloma patients treated on clinical trials, a fitness score created from geriatric assessment variables (ADLs, IADLs, and Charlson Comorbidity Index) demonstrated that, compared with “fit” patients, those classified as “frail” were more likely to experience grade 3 or higher nonhematologic toxicity. Drug discontinuation for any cause (excluding progression or death) was higher in “unfit” and “frail” patients compared with “fit” patients.10 Studies evaluating the use of geriatric assessment in the setting of aggressive non-Hodgkin lymphoma have also shown an association between parameters detected by geriatric assessment and treatment tolerance.11,23 In a cohort study of older adults with myelodysplastic syndrome treated with azacitidine, geriatric assessment measures were associated with treatment discontinuation largely due to intolerance.14 Among older adults with multiple myeloma undergoing autologous stem cell transplantation, objectively measured physical function was associated with length of stay, whereas several geriatric assessment parameters (anxiety/depression, low grip strength, falls, and weight loss) were associated with a higher likelihood of readmission.29 Not all studies have shown an association between geriatric assessment parameters and toxicity risk,8 although impaired physical function and comorbidity burden appear to be the most consistent risk factors in those studies reporting an association.
Geriatric assessment predicts survival
Most studies evaluating the utility of geriatric assessment in hematologic malignancies have included overall survival as the primary outcome. Data are consistent across disease and treatment settings that parameters included in geriatric assessments can refine estimates of overall survival for older adults.30 Table 3 includes an overview of studies evaluating the added value of geriatric assessment measures to predict survival in various settings.7-10,12,14,19,21-24,29,31-34 Studies have differed in approach, with some evaluating summary scores based on several geriatric assessment measures and others investigating the independent role of specific vulnerabilities, such as comorbidity, physical function, cognitive function, and nutritional status. Vulnerabilities detected by geriatric assessment are associated with survival for patients with indolent and aggressive diseases, as well as for those receiving lesser vs more intensive therapies. The most consistent factors associated with survival across populations are measures of physical function beyond oncology performance status (either self-reported or objectively measured). Additional characteristics that are repeatedly represented are comorbidity burden, nutritional status, and cognitive impairment.30 Among self-reported functional measures, requiring assistance with IADLs has been one of the most consistent markers of vulnerability and can be easily incorporated into practice. Measuring physical function objectively (ie, gait speed, Timed Up and Go, Short Physical Performance Battery) can provide a more sensitive estimate of physical performance, identifying vulnerability that may not be self-reported. These measures are robustly associated with mortality in general geriatric populations and predict survival in certain hematologic disease settings.8,9,35,36 Gait speed and grip strength are 2 of the 5 parameters for assessment of frailty using the phenotypic approach.4 In practice, usual gait speed over a 4-m course is most straightforward to implement and is included in the Geriatric Assessment Hematology scale.17 Cognitive impairment also warrants increased attention when evaluating older adults with hematologic malignancies. Among older adults with blood cancers, cognitive impairment is common and has been associated with worse overall survival in several settings.8,9,37 Brief screening tests to consider in clinical practice include the Mini-Cog, a 5-word recall, or the Blessed Orientation Memory Concentration test.3,37 As indicated in Table 3, the optimal geriatric measures to use for risk stratification may differ from 1 setting to the next and will continue to be informed by ongoing and future clinical trials. However, regardless of setting, those patients who have no or minimal detectable vulnerabilities across multiple domains can be considered fit, whereas those with multiple concurrent vulnerabilities would be categorized as frail. This approach in practice provides a framework within which to have a personalized treatment discussion.
Selected trials highlighting predictive utility of geriatric assessment measures for older adults with hematologic malignancy
| Disease type/setting . | No. patients . | Outcomes predicted . | Measures . |
|---|---|---|---|
| Chronic lymphocytic leukemia8 | 75 | Overall survival | Low objective physical performance (Timed Up and Go) and cognition |
| Multiple myeloma10 | 869 | Overall survival, nonhematologic adverse events, treatment discontinuation | Composite fitness score (ADLs, IADLs, comorbidity, age) |
| Acute myeloid leukemia9 | 74 | Overall survival | Low objective physical function (Short Physical Performance Battery) and cognition |
| Acute myeloid leukemia/myelodysplastic syndrome7 | 195 | Overall survival | ADLs and fatigue in nonintensively treated patients |
| Myelodysplastic syndrome14 | 98 | Overall survival and treatment duration. | IADLs and comorbidity associated with overall survival. IADLs, cognition, and low objective physical function (Timed Up and Go) associated with treatment duration. |
| Myelodysplastic syndrome19 | 455 | Overall survival | Clinical frailty score and comorbidity |
| Non-Hodgkin lymphoma22 | 143 | Overall survival | IADLs and comorbidity |
| Non-Hodgkin lymphoma32 | 173 | Overall survival | Composite fitness score (ADLs, IADLs, comorbidity, age) |
| Non-Hodgkin lymphoma33 | 99 | Overall survival, response rates, progression-free survival | IADLs, composite score (albumin, comorbidity, age) |
| Non-Hodgkin lymphoma23 | 70 | Overall survival, early discontinuation of chemotherapy | Nutritional status associated with both outcomes |
| Hodgkin lymphoma33 | 48 | Progression-free survival | Loss of IADLs |
| Bone marrow transplantation (mixed population)12 | 203 | Overall survival | IADLs, gait speed, comorbidity, mental health |
| Bone marrow transplantation (mixed population)24 | 184 | Overall survival | IADLs, physical subscale of Functional Assessment of Cancer Therapy Bone Marrow Transplant |
| Bone marrow transplantation (mixed population, allogeneic transplantation)21 | 106 | Overall survival | Low objective physical performance (Timed Up and Go), fatigue |
| Bone marrow transplantation (multiple myeloma)29 | 100 | Hospital readmission, hospital length of stay | Decreased grip strength, anxiety/depression, falls, and weight loss associated with readmission. Objective (Short Physical Performance Battery) and self-reported physical function associated with length of stay. |
| Mixed population (myelodysplastic syndrome, leukemia, multiple myeloma, lymphoma)34 | 314 | Overall survival, unplanned hospitalization | Slower gait speed associated with increase mortality and unplanned hospitalizations |
| Lower grip strength associated with shorter survival |
| Disease type/setting . | No. patients . | Outcomes predicted . | Measures . |
|---|---|---|---|
| Chronic lymphocytic leukemia8 | 75 | Overall survival | Low objective physical performance (Timed Up and Go) and cognition |
| Multiple myeloma10 | 869 | Overall survival, nonhematologic adverse events, treatment discontinuation | Composite fitness score (ADLs, IADLs, comorbidity, age) |
| Acute myeloid leukemia9 | 74 | Overall survival | Low objective physical function (Short Physical Performance Battery) and cognition |
| Acute myeloid leukemia/myelodysplastic syndrome7 | 195 | Overall survival | ADLs and fatigue in nonintensively treated patients |
| Myelodysplastic syndrome14 | 98 | Overall survival and treatment duration. | IADLs and comorbidity associated with overall survival. IADLs, cognition, and low objective physical function (Timed Up and Go) associated with treatment duration. |
| Myelodysplastic syndrome19 | 455 | Overall survival | Clinical frailty score and comorbidity |
| Non-Hodgkin lymphoma22 | 143 | Overall survival | IADLs and comorbidity |
| Non-Hodgkin lymphoma32 | 173 | Overall survival | Composite fitness score (ADLs, IADLs, comorbidity, age) |
| Non-Hodgkin lymphoma33 | 99 | Overall survival, response rates, progression-free survival | IADLs, composite score (albumin, comorbidity, age) |
| Non-Hodgkin lymphoma23 | 70 | Overall survival, early discontinuation of chemotherapy | Nutritional status associated with both outcomes |
| Hodgkin lymphoma33 | 48 | Progression-free survival | Loss of IADLs |
| Bone marrow transplantation (mixed population)12 | 203 | Overall survival | IADLs, gait speed, comorbidity, mental health |
| Bone marrow transplantation (mixed population)24 | 184 | Overall survival | IADLs, physical subscale of Functional Assessment of Cancer Therapy Bone Marrow Transplant |
| Bone marrow transplantation (mixed population, allogeneic transplantation)21 | 106 | Overall survival | Low objective physical performance (Timed Up and Go), fatigue |
| Bone marrow transplantation (multiple myeloma)29 | 100 | Hospital readmission, hospital length of stay | Decreased grip strength, anxiety/depression, falls, and weight loss associated with readmission. Objective (Short Physical Performance Battery) and self-reported physical function associated with length of stay. |
| Mixed population (myelodysplastic syndrome, leukemia, multiple myeloma, lymphoma)34 | 314 | Overall survival, unplanned hospitalization | Slower gait speed associated with increase mortality and unplanned hospitalizations |
| Lower grip strength associated with shorter survival |
Geriatric assessment predicts health care utilization
Health care utilization, particularly time spent in the hospital, is a key concern for patients and the health care system. For patients, families, and providers, an unplanned hospitalization factors into “treatment tolerance.” The negative consequences of hospitalization on functional outcomes and independence can be profound. Hospitalization length and readmission rates are also costly quality indicators for health care systems. Identifying patients who are more likely to experience a hospitalization provides an opportunity to inform patients regarding the risks of therapy, as well as to develop care pathways to minimize these risks if anticipated. Recent studies have demonstrated an association between vulnerabilities detected on geriatric assessment and health care utilization.29,30,38 In a cohort study of 464 adults aged 75 years or older with hematologic malignancies at a large tertiary care center, dependence in IADLs (present in 27%) was associated with a greater than twofold increased odds of emergency room visits and hospitalizations.30 In another study of older patients who received autologous stem cell transplantation, readmission rates were higher among those patients with anxiety/depression, lower hand-grip strength, falls, or weight loss detected on geriatric assessment.29 Most studies have not captured health care utilization as an outcome, which presents an opportunity for future trials.
Case continued
The patient is interested in proceeding with chemotherapy (rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) after discussion of risks and benefits. She asks how she will be monitored during treatment. She is particularly concerned about maintaining her functional status.
Geriatric assessment as an outcome: enhancing understanding of treatment tolerance and benefit
Most studies evaluating geriatric assessment in hematologic malignancies have addressed its role in risk prediction; however, measuring how patients feel and function continues to be relevant during the course of treatment and into survivorship. Geriatric assessment can be used to characterize treatment tolerance and benefit. For example, repeated assessments of function (physical, cognitive), emotional well-being, and nutritional status can supplement symptom reporting and disease response assessments. Functional independence and quality of life are important outcomes for older adults, although they are rarely captured on therapeutic clinical trials. A review of >1200 clinical trials in hematologic malignancies from the National Institutes of Health trial registry found that quality of life and functional capacity were reported objectives in only 8% and 0.7% of trials, respectively.39 The value of repeat geriatric assessment was shown in a small prospective study of older adults with acute myeloid leukemia.40 This analysis (N = 49) evaluated the effect of intensive induction therapy on physical, cognitive, and emotional health and found that self-reported and objectively measured physical function declined significantly postinduction therapy. By contrast, cognitive function was stable, and emotional health improved. Repeat assessments have also been used for older adults undergoing stem cell transplantation.21,29 For example, postallogeneic stem cell transplantation geriatric assessment characterized declines in physical function, nutritional status, quality of life, and trajectory of recovery over 6 months.21 These data provide a better understanding of the treatment experience and provide targets for interventions to improve treatment tolerance.
Geriatric assessment can guide personalized supportive care
Optimized quality of care for older cancer patients depends on enhancing the prediction of treatment outcomes, as well as on personalized management strategies that are designed to enhance treatment tolerance and resilience. Data from geriatric assessment can guide supportive care to address vulnerabilities whenever possible. Consensus statements exist to provide a framework to match interventions to impairments detected.41 Examples include referrals to ancillary providers, such as physical and occupational therapists, dieticians, social workers, or psychologists, to address concerns related to physical function, nutritional status, socioeconomic concerns, or emotional health, respectively.42 Referral to a geriatrician to develop and manage an intervention plan is an attractive strategy, although access to geriatricians remains limited in many settings.43 An example of this paradigm was tested in a study evaluating a nurse-led geriatric assessment for older adults with myelodysplastic syndrome receiving low-intensity therapy. After screening, the following interventions were recommended upon geriatric consultation: changes in medications (59%), investigation of comorbid conditions (62%), social support referral (35%), nutritional counseling/referral (37%), cognitive evaluation (59%), physical therapy referral or counseling (40%), and referral to psychologist (13%).14 The use of mobile health technology may provide a user-friendly approach to gather geriatric assessment data and map results to supportive care interventions.44 Another area of active research is testing interventions to maintain physical function during and after therapies. Several studies have demonstrated the feasibility of physical activity interventions among older adults with hematologic malignancies. Larger efficacy trials may provide data to incorporate new supportive care paradigms designed to optimize the maintenance of physical function into treatment plans for older adults.45-48
Case continued
The patient and her provider discuss opportunities to optimize her supportive care during treatment. She is referred to a dietician to maximize her nutritional status. Repeat abbreviated geriatric assessments will be done intermittently during treatment, with an emphasis on monitoring her physical function to prompt early referrals to therapists as needed. The patient and her son are reassured and appreciate the personalized care plan.
Geriatric assessment adds value: provider and patient perspectives
Are geriatric assessment data useful to providers? Studies indicate that providers change initial treatment plans in up to a third of patients when provided with geriatric assessment data for their patients. A systematic review of the effect of geriatric evaluation on treatment recommendations showed that, after receiving results, oncologists changed initial treatment plans to recommend less intensive therapy for approximately one quarter of patients (26%), as well as more intensive treatment for 13% of patients.49 Receipt of geriatric assessment data also improves the quality of patient–provider discussions. This was demonstrated in a preliminary report from a large cluster randomized trial (N = 544 from 31 practices in the United States) that randomized sites to performing a primarily patient-administered geriatric assessment vs usual care. Among those sites performing geriatric assessment, providers were given a summary of results for individual patients, as well as a list of recommended interventions. The outcome was improved communication. Sites randomized to geriatric assessment recorded significantly more discussions about age-related issues and had more discussions rated as higher quality. These discussions led to approximately twice as many interventions. Importantly, this translated into higher patient satisfaction.50 Several large ongoing studies are underway to test whether geriatric assessment–guided interventions lead to decreased toxicity, lower rates of hospitalization, improved function and quality of life, and prolonged survival.41 To date, these types of outcomes have been shown to improve in older adults without cancer. Data specific to hematologic diseases remain limited but are expected in the coming years.
Next steps: implementation and beyond
Data are sufficient to support the use of geriatric assessment in hematology practice.3 Information gained can inform treatment decisions, management, and communication. There is no single gold standard assessment measure; instead, there are many options from which to choose depending upon preferences, resources, and setting. Most assessments are primarily self-administered, although clinical staff can be trained to facilitate administration of cognition testing and objective physical testing (ie, gait speed). Although most evidence supports the use of geriatric assessment at baseline for initial treatment decision making, additional assessments during or after treatment, at the time of a new treatment decision, or yearly during survivorship can help to guide care for older adults.
The next steps will include evaluating strategies for implementation into practice and to incorporate geriatric assessment consistently in clinical trials. Studies of geriatric assessment–guided treatment and supportive care interventions are needed to ensure that quality of care can be maximized for each older patient in accordance with their goals and values.
Authorship
Contribution: H.D.K. reviewed the literature and wrote the manuscript.
Conflict-of-interest disclosure: H.D.K. declares no competing financial interests. Off-label drug use: None disclosed.
Correspondence: Heidi D. Klepin, Comprehensive Cancer Center, Wake Forest Health Sciences, Medical Center Blvd, Winston-Salem, NC 27157; e-mail: hklepin@wakehealth.edu.
This article was selected by the Blood and Hematology 2019 American Society of Hematology Education Program editors for concurrent submission to Blood and Hematology 2019. It is reprinted in Hematology Am Soc Hematol Educ Program. 2019;2019:53-58.