In this issue of Blood, Tang et al present the results of a large multicenter trial in pediatric acute lymphoblastic leukemia (ALL) that identifies prognostic factors for central nervous system (CNS) relapse and provides some intriguing observations on practical measures that may improve CNS control.1
The largest advance in survival rates for childhood ALL came with the recognition in the 1970s that eradication of disease in the CNS is vital for long-term cure.2 The original use of craniospinal irradiation has now largely been replaced with intensive intrathecal therapy with methotrexate alone or in combination with cytarabine, asparaginase, and corticosteroids. However, how much CNS-directed treatment is required, for which patients, and how best to deliver it, remain unsolved challenges 50 years on.
CNS leukemia is diagnosed by cerebrospinal fluid (CSF) cytology, with 3% to 5% of patients having positive cytology at diagnosis. However, data from animal models and postmortem studies suggest that most children have subclinical (cytology-negative) CNS infiltration.3 The inability of cytology to accurately measure CNS leukemia has led to universal use of prolonged intensive CNS-directed therapy, resulting in significant acute and chronic neurotoxic sequelae, including long-term cognitive deficits in 20% to 40% of patients.4 Despite recognition of the importance of treating the CNS, and the known toxicity of existing agents, no new classes of drugs for CNS leukemia have been licensed in the past half-century. Because cure rates now exceed 90%, using neurotoxic drugs in non-risk-adapted protocols is unacceptable and a paradigm shift in treating CNS ALL is required.
Tang et al report results from the CCCG-ALL-2015 trial, which recruited 7640 children aged 0 to 18 years across 20 major hospitals/medical centers in China. The study used upfront dexamethasone for 4 to 5 days before diagnostic lumbar puncture, general anesthesia (in 3/20 centers) and CSF flow cytometry (in 2/20 centers) to reduce the incidence of traumatic lumbar puncture and accurately ascertain the level of initial CNS involvement. Besides the known risk factors of T-cell immunophenotype, presenting white blood cell count, and high-risk cytogenetics for CNS relapse, they identified female sex, general anesthesia, and flow cytometry as protective factors. Their low rates of CNS relapse, despite omission of radiotherapy and inclusion of high-risk subgroups, might suggest a potential protective effect of steroids before diagnostic lumbar puncture. The latter finding supports another recent report from the Taiwan Pediatric Oncology Group that delayed lumbar puncture does not harm CNS control.5 These findings rightly focus attention on how to improve our treatment of the CNS.
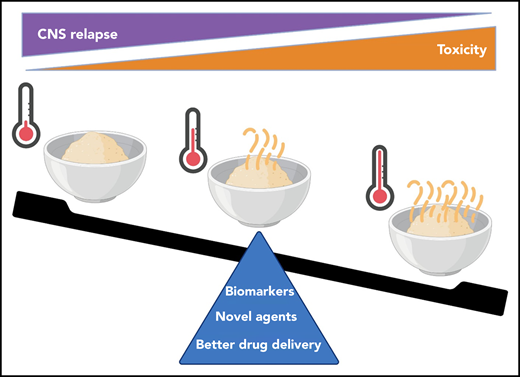
CNS-directed therapy is a delicate balance between toxicity and efficacy. Each child requires just enough therapy to prevent relapse (too cold) while avoiding toxicity (too hot). This will be achieved by accurate biomarkers, trials of less toxic agents, and ensuring that drugs efficiently reach their targets in the CNS.
CNS-directed therapy is a delicate balance between toxicity and efficacy. Each child requires just enough therapy to prevent relapse (too cold) while avoiding toxicity (too hot). This will be achieved by accurate biomarkers, trials of less toxic agents, and ensuring that drugs efficiently reach their targets in the CNS.
So, what are the current barriers to progress? First, the absence of clinically useful biomarkers prevents accurate risk stratification, resulting in universal use of intensive CNS-directed therapy. This therapy is likely to overtreat many children, exposing them to an unnecessary risk of toxicity. Conversely, a minority of children who go on to relapse in the CNS has clearly received insufficient treatment. Results from Tang et al confirm that cytomorphology is inadequate to accurately evaluate the CNS. Recent data from the Nordic Society of Pediatric Hematology and Oncology NOPHO-2008 trial also indicate that flow cytometry of diagnostic CSF samples is superior to cytomorphology for predicting CNS relapse.6 However, flow cytometry is not sensitive enough to track disease response over time. In the bone marrow minimal residual disease is used to identify children at high or low risk of relapse and modify therapy accordingly. We desperately need a minimal residual disease equivalent for CNS leukemia to allow us to tailor therapy. We want to reach a Goldilocks point: not too much, not too little, but just right for every child (see figure).
The lack of accurate biomarkers also hampers new drug development. Current intrathecal therapies usually rapidly clear visible leukemic cells in CSF but subclinical disease is likely to remain, explaining the need for prolonged intensive therapy. We are essentially “shooting blind” when treating the CNS. We need large numbers of patients and long follow-up to see the impact of new drugs on late CNS relapses, which are thankfully rare events. An ability to measure depth of remission at early time points would give a rapid surrogate end point. This would give confidence to treating clinicians and families when testing novel therapies that show promise in terms of reduced toxicity but still need to prove efficacy.
What about immunotherapy for the CNS? Unfortunately, many children with CNS involvement were excluded from early trials of chimeric antigen receptor-T cell therapy and blinatumomab because of concerns regarding neurological toxicity. Real-world data collection has established that chimeric antigen receptor T cells show some promise in this area,7 but larger studies are awaited.
Finally, delivering intrathecal therapy via lumbar puncture is a hit-or-miss game. Drug distribution is variable and position dependent; at least 10% of intrathecal treatments miss the subarachnoid space and previous traumatic lumbar puncture can result in fibrous tissue, further hampering CSF flow from the lumbar spine to the brain.8 The observation by Tang et al that use of general anesthesia appears to improve CNS control may be because of more accurate drug delivery. Unfortunately, rapid adoption of this approach is tempered by the recent observation that repeated general anesthesia in children with ALL is associated with increased neurotoxicity.9 Another approach is the use of Ommaya reservoirs, which abolish the need for general anesthesia, result in more predictable pharmacokinetics, and, perhaps surprisingly, were often preferred by patients and families.8 However, concerns regarding infection rates and difficulties in removing the device at the end of treatment have led to a low acceptance by treating physicians. Another possibility is to use systemic drugs with good CNS penetration. Indeed, one of the key advantages of switching from prednisolone to dexamethasone is the improved CNS control; however, dexamethasone is not without its own neurological and systemic toxicity. Interestingly, an increased focus on targeted drug delivery for brain tumors in children is driving innovation in CNS-delivery devices and novel routes of administration such as intranasal chemotherapy. Sharing of learning between the 2 communities will be important as we move forward.10
The time has come for an increased focus on how, where, and when we deliver CNS-directed therapy. Children with ALL deserve to have this done “just right.”
Conflict-of-interest disclosure: The authors declare no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal