Abstract
Asciminib, a first-in-class allosteric inhibitor of BCR::ABL1 kinase activity, is now approved for the treatment of patients with chronic-phase chronic myeloid leukemia who failed 2 lines of therapy or in patients with the T315I mutation. Promising attributes include high specificity and potency against BCR::ABL1, activity against most kinase domain mutations, and potential for combination therapy with ATP-competitive tyrosine kinase inhibitors. Clinicians now have expanded third-line options, which in most cases will involve a choice between asciminib and ponatinib.
Introduction
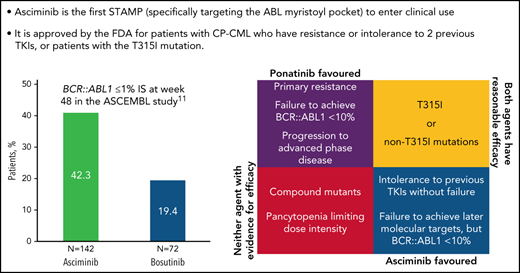
In October 2021, the Food and Drug Administration granted accelerated approval for a first-in-class allosteric myristoyl inhibitor, asciminib, to treat patients with chronic-phase chronic myeloid leukemia (CML) with resistance or intolerance to 2 prior lines of tyrosine kinase inhibitor (TKI) therapy, and for patients with the T315I mutation.1 Similar submissions are currently before regulatory agencies in other jurisdictions. This drug, previously known as ABL001 in its development program, works by binding to the myristoyl pocket of the BCR::ABL1 protein (note recent recommendation from HUGO Gene Nomenclature Committee to use BCR::ABL1 in place of BCR-ABL1 or BCR/ABL1).2 The N-terminus myristoyl group of ABL1, encoded by exon 1, usually binds in this pocket, enabling autoinhibition. This self-regulation is lost with the formation of BCR::ABL1. Asciminib binding, independent of the ATP-binding pocket where all other currently available TKIs bind, mimics the myristoyl pocket interaction and inhibits BCR::ABL1 activity.3,4 Structural analysis suggests relatively specific drug binding to BCR::ABL1, ABL1, and ABL2, with very little off-target binding.5 Pharmacokinetic studies after a single dose of 40 mg suggest it is not significantly affected by renal or hepatic dysfunction, although further data and clinical experience is awaited at other dosing levels.6 Given its theoretical mechanism of action, Novartis has coined the term STAMP (Specifically Targeting the ABL Myristoyl Pocket) to differentiate it from ATP-pocket binding TKIs currently in use.7
Asciminib entered clinical development in the phase 1 CABL001X2101 study, which enrolled patients with CML with either resistance or intolerance to 2 or more previous TKIs. Patients in cohorts were treated with asciminib monotherapy or in combination with either imatinib 400 mg per day, nilotinib 300 mg twice a day, or dasatinib 100 mg daily combined with asciminib at doses up to 40 mg twice a day per 80 mg daily. The first 150 patients treated with monotherapy tolerated the treatment well. Despite assignments of asciminib ranging from 10 mg to 200 mg twice a day, the majority of the adverse events reported were of grade 1 or 2, without a maximum tolerated dose being reached. Asymptomatic elevations in the lipase or amylase level, rash, and constitutional symptoms were the most common adverse events. Even in this relatively heavily pretreated group (85% having previously failed 3 or more TKIs), early efficacy was evident, with a major molecular response (MMR; BCR::ABL1 ≤0.1% on the International Scale [IS]) being achieved or maintained by 12 months in 48% of the evaluable patients.8 This study also included an expanded cohort of patients with the T315I mutation, treated with a higher dose of asciminib, 200 mg twice a day. As of April 2020, results for 52 T315I patients were reported, with 41% of patients having achieved MMR after 24 weeks. Of note, activity was observed in T315I patients after ponatinib failure, with a 24-week MMR rate of 29% (as compared with 57% in ponatinib-naive patients).9
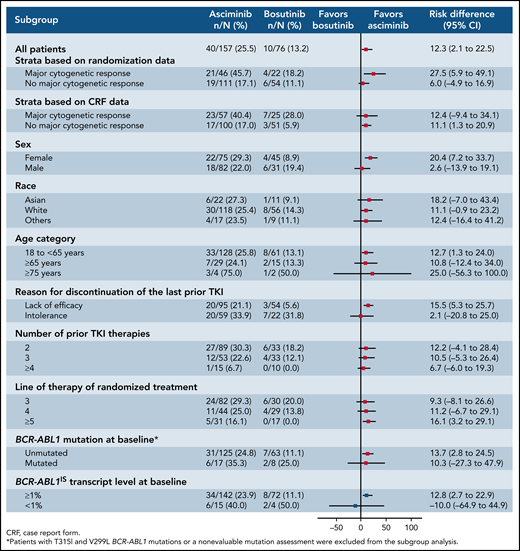
The encouraging phase 1 data were followed by the ASCEMBL study, which enrolled 233 patients previously treated with 2 or more TKIs, and were randomized in a 2:1 ratio to asciminib 40 mg twice a day vs bosutinib 500 mg daily. The primary end point, MMR at 24 weeks, was achieved by 25% (95% confidence interval [CI]: 19% to 33%) in the asciminib arm as compared with 13% (95% CI: 6.5% to 23%; P = .029) in the bosutinib arm.10 In subgroup analyses, there was a trend favoring asciminib treatment in patients regardless of numbers of previous lines of treatment. Asciminib was superior in patients who discontinued their last TKI because of lack of efficacy (Figure 1). Importantly, treatment was discontinued in 71% of patients assigned to bosutinib by week 48, mostly because of adverse events or lack of efficacy, as compared with 33% of patients assigned asciminib at the same time point, again suggesting that asciminib is relatively well tolerated and efficacious, even in this heavily pretreated group.11 Pharmacokinetically, the currently recommended single daily dose of 80 mg is largely equivalent to 40 mg twice a day. The recommended dosing for patients with the T315I mutation remains 200 mg twice a day.
Subgroup analysis of MMR at 24 months for patients who participated in the ASCEMBL study. Data are presented as a Forest plot, with a trend favoring asciminib in most demographic and prognostic subgroups. Reproduced from Réa et al.10
Subgroup analysis of MMR at 24 months for patients who participated in the ASCEMBL study. Data are presented as a Forest plot, with a trend favoring asciminib in most demographic and prognostic subgroups. Reproduced from Réa et al.10
How should clinicians integrate asciminib into their practice? Even before the introduction of asciminib, there were a number of TKIs to choose from. These drugs have been remarkably successful clinically, regarded as a paradigm for how small molecule inhibitors can transform cancer therapy. They have allowed the majority of patients with chronic-phase CML to enjoy life expectancy approaching age-matched controls.12,13 However, better options are needed for the 20% to 30% of patients who experience therapeutic failure. These patients fall into 2 broad categories, commonly referred to as treatment resistant and treatment intolerant, although significant overlap often exists.
The best documented cause of TKI resistance is kinase domain mutations. Aside from asciminib, all other BCR::ABL1 inhibitors bind to the kinase domain of the BCR::ABL1 protein. This denies ATP its usual binding site, interfering with phosphorylation of substrate proteins and subsequent downstream prosurvival and proliferative signals. More than 50 of these point mutations have been observed.14 This problem has partially been overcome through rational drug design, and introduction of increasingly potent BCR::ABL inhibitors. However, the more resistant mutations, including Y253H, E255K/V, F359V/C/I, F317L, and G250E, still demand careful drug selection.14 Importantly, the “gatekeeper” T315I mutation will confer resistance to all approved TKIs except the third-generation drug ponatinib. Compound mutations, where >1 kinase mutation is manifested on the same BCR::ABL1 molecule, such as the E255K/T315I combination, confer resistance even to ponatinib.15
Aside from frank treatment resistance, patients may discontinue treatment owing to toxicity. Alternatively, patients may decide to continue with therapy, but with significant adverse impact on quality of life. There are also risks of delayed toxicity with cumulative treatment, which may be associated with long-term morbidity or mortality. The adverse event profile of the commonly used TKIs is relatively well known. For imatinib, gastrointestinal irritation leading to nausea and diarrhea is common, as are muscle cramping and edema. These side effects do not lead to serious morbidity, but do have significant impact on quality of life and often lead to imatinib dose reduction or cessation.16 The incidence of adverse events for dasatinib, a second-generation drug, is lower than imatinib, although a cumulative risk of pleural effusion of 25% to 40% with the former can be clinically significant, sometimes leading to dasatinib discontinuation.17 Perhaps more importantly, there is an increased risk of arterial occlusive disease associated with the more potent second- and third-generation TKIs compared with imatinib, manifested as peripheral arterial occlusive disease, ischemic heart disease, or strokes.18 In the phase 3 randomized ENESTnd study that enrolled newly diagnosed patients with chronic-phase CML, the rate of cardiovascular events in patients treated with nilotinib 300 mg twice a day was 16.5% at 10 years, as compared with 3.6% in imatinib-treated patients.19 Ponatinib-associated arteriopathy is potentially a greater concern, with recently published data from the OPTIC study demonstrating a clear dose-toxicity relationship between this drug and treatment-related arterial occlusive disease. Importantly, OPTIC demonstrated that dose deescalation to 15 mg daily, as soon as a molecular response (<1% BCR::ABL1 IS) is achieved, can minimize arteriopathy while maintaining response in most cases.20
The Food and Drug Administration’s approval of asciminib is a welcome additional option to ponatinib, which already has an indication for chronic-phase CML in the third-line setting, or in any patient with T315I. No current data exist to directly compare the safety or efficacy of the 2 drugs, and the best option for each patient is therefore an individualized decision based on clinical judgment and patient preference (Table 1). Ponatinib and high-dose asciminib appear to be equally efficacious in the context of the T315I mutation. Although detailed information is lacking, the efficacy for the 2 agents can also be inferred for other individual mutations, with the exception of relative resistance conferred by the F359 mutation against asciminib. Certain compound mutations, if verified, will likely confer resistance to both drugs.
Recommendations for treatment of chronic-phase CML with treatment resistance or intolerance in the third line
| Clinical category . | Case example . | Relevant data . | Comment . | Strength of evidence and urgency for further clinical trials . |
|---|---|---|---|---|
| Asciminib preferred | ||||
| Intolerance to previous TKI therapy. Molecular response achieved | Patient who has received imatinib, nilotinib, and dasatinib and developed significant intolerance or toxicity to each TKI | Phase 1 asciminib study; ASCEMBL, 42% MMR at 6 mo in intolerant cohort | ASCEMBL supports superiority of asciminib over bosutinib in this setting. Very limited role for ponatinib in this setting. Other TKIs may also be appropriate depending on individual circumstances | Good level of evidence. Less urgent priority for further clinical trials |
| Treatment failure (failure to achieve mol targets) but responsive disease (eg, BCR::ABL1 ≤10% or in MCyR) | >1% BCR::ABL1 after 12 mo of imatinib, still >1% after further 6 mo of nilotinib | ASCEMBL, patients in MCyR achieved 46% MMR by 6 mo | These patients are TKI sensitive and may benefit from the greater potency and tolerability of asciminib compared with the current 2-G TKI they are receiving. May be safer option than ponatinib | More data needed. High priority for randomized study of ponatinib vs asciminib |
| Ponatinib preferred | ||||
| BCR::ABL1 >10% (IS) | No cytogenetic and/or molecular response after 6 mo of imatinib followed by 6 mo of nilotinib, patient being considered for an allograft | In OPTIC, patients >10% BCR::ABL1 at study entry (45-mg group) 51% achieved MMR by 3 y In ASCEMBL, patients >10% BCR::ABL1 at baseline: 17% MMR at 24 wk | Both TKIs active in this setting; ponatinib may have an advantage because of its activity against other kinases that might be contributing to resistance pathways | More data needed. OPTIC and ASCEMBL have very different trial designs and follow-up. High priority for randomized study of ponatinib vs asciminib indicated. Combination TKI + asciminib may also be effective |
| Both asciminib and ponatinib may be acceptable | ||||
| T315I mutation | Poor response to 1st-line dasatinib and loss of response after 12 mo with 70% T315I mutation | OPTIC: 60% achieved MMR on ponatinib 45-mg arm by 3 y CABL001X2101: asciminib 200 mg twice a day: 41% MMR after 24 wk | Unclear whether efficacy is superior for either ponatinib vs asciminib. Tolerability may also be similar at the asciminib 200-mg twice daily dose | Longer follow-up needed for asciminib. High priority for randomized study of ponatinib vs asciminib |
| Non-T315I kinase domain mutations | Poor response to 1st-line nilotinib and loss of response after 12 mo with E255K mutation | Non-T315I mutation data incomplete. Only 13% of ASCEMBL patients had a history of kinase domain mutations | Data pending for individual mutations. F359 may confer resistance to asciminib; higher dose of 200 mg twice a day may be necessary | More data needed on individual mutations; preference may depend on specific mutation. Low frequency of specific mutation and clinical heterogeneity a challenge for clinical studies |
| Neither asciminib nor ponatinib particularly effective | ||||
| Compound kinase domain mutations | Poor response to 1st-line dasatinib and loss of response after 12 mo with compound T315I/E255K mutation | Clinical data suggesting lack of efficacy for ponatinib Only 3 patients in ASCEMBL had multiple mutations | In vitro evidence that combination of asciminib plus ponatinib may be effective in this setting (see text) | No clinical evidence. Exploratory trials of combination ponatinib plus asciminib indicated. Asciminib combined with other TKIs may also be effective |
| TKI resistance in the setting of marked cytopenia | Patient who has failed 2 or more TKIs with extended interruptions for severe neutropenia and thrombocytopenia | No published data | This is one of the most challenging settings; an allograft may be the only effective therapy | No evidence exists. Exploratory trials indicated |
| Clinical category . | Case example . | Relevant data . | Comment . | Strength of evidence and urgency for further clinical trials . |
|---|---|---|---|---|
| Asciminib preferred | ||||
| Intolerance to previous TKI therapy. Molecular response achieved | Patient who has received imatinib, nilotinib, and dasatinib and developed significant intolerance or toxicity to each TKI | Phase 1 asciminib study; ASCEMBL, 42% MMR at 6 mo in intolerant cohort | ASCEMBL supports superiority of asciminib over bosutinib in this setting. Very limited role for ponatinib in this setting. Other TKIs may also be appropriate depending on individual circumstances | Good level of evidence. Less urgent priority for further clinical trials |
| Treatment failure (failure to achieve mol targets) but responsive disease (eg, BCR::ABL1 ≤10% or in MCyR) | >1% BCR::ABL1 after 12 mo of imatinib, still >1% after further 6 mo of nilotinib | ASCEMBL, patients in MCyR achieved 46% MMR by 6 mo | These patients are TKI sensitive and may benefit from the greater potency and tolerability of asciminib compared with the current 2-G TKI they are receiving. May be safer option than ponatinib | More data needed. High priority for randomized study of ponatinib vs asciminib |
| Ponatinib preferred | ||||
| BCR::ABL1 >10% (IS) | No cytogenetic and/or molecular response after 6 mo of imatinib followed by 6 mo of nilotinib, patient being considered for an allograft | In OPTIC, patients >10% BCR::ABL1 at study entry (45-mg group) 51% achieved MMR by 3 y In ASCEMBL, patients >10% BCR::ABL1 at baseline: 17% MMR at 24 wk | Both TKIs active in this setting; ponatinib may have an advantage because of its activity against other kinases that might be contributing to resistance pathways | More data needed. OPTIC and ASCEMBL have very different trial designs and follow-up. High priority for randomized study of ponatinib vs asciminib indicated. Combination TKI + asciminib may also be effective |
| Both asciminib and ponatinib may be acceptable | ||||
| T315I mutation | Poor response to 1st-line dasatinib and loss of response after 12 mo with 70% T315I mutation | OPTIC: 60% achieved MMR on ponatinib 45-mg arm by 3 y CABL001X2101: asciminib 200 mg twice a day: 41% MMR after 24 wk | Unclear whether efficacy is superior for either ponatinib vs asciminib. Tolerability may also be similar at the asciminib 200-mg twice daily dose | Longer follow-up needed for asciminib. High priority for randomized study of ponatinib vs asciminib |
| Non-T315I kinase domain mutations | Poor response to 1st-line nilotinib and loss of response after 12 mo with E255K mutation | Non-T315I mutation data incomplete. Only 13% of ASCEMBL patients had a history of kinase domain mutations | Data pending for individual mutations. F359 may confer resistance to asciminib; higher dose of 200 mg twice a day may be necessary | More data needed on individual mutations; preference may depend on specific mutation. Low frequency of specific mutation and clinical heterogeneity a challenge for clinical studies |
| Neither asciminib nor ponatinib particularly effective | ||||
| Compound kinase domain mutations | Poor response to 1st-line dasatinib and loss of response after 12 mo with compound T315I/E255K mutation | Clinical data suggesting lack of efficacy for ponatinib Only 3 patients in ASCEMBL had multiple mutations | In vitro evidence that combination of asciminib plus ponatinib may be effective in this setting (see text) | No clinical evidence. Exploratory trials of combination ponatinib plus asciminib indicated. Asciminib combined with other TKIs may also be effective |
| TKI resistance in the setting of marked cytopenia | Patient who has failed 2 or more TKIs with extended interruptions for severe neutropenia and thrombocytopenia | No published data | This is one of the most challenging settings; an allograft may be the only effective therapy | No evidence exists. Exploratory trials indicated |
In the absence of a kinase domain mutation, the current data and the greater body of clinical experience would favor ponatinib in the context of frank resistance. Ponatinib has also demonstrated efficacy in advanced-phase CML and Philadelphia-positive acute lymphoblastic leukemia in the third-line setting. The PACE study showed similar cytogenetic and molecular responses achieved in each of these subgroups regardless of the T315I status,21 and many of the responders continue to derive benefit at 5 years.22 With a dosing regimen adapted from OPTIC that appears to minimize vascular toxicity while still being effective, ponatinib can now be prescribed with greater confidence for patients requiring third- (or later) line therapy.20
Asciminib may be preferred in patients with significant vascular risk factors, or a history of cardiovascular disease, or in patients with previously documented toxicities that are expected to be related to the class of ATP-competitive TKIs. Asciminib may also be the preferred choice in patients who have failed to achieve time-dependent molecular targets, but appear to be TKI responsive. It is not uncommon to identify adverse events that lead to dose interruptions or reductions, and such patients commonly show features of both intolerance and resistance. Noting the discontinuation rate in the ASCEMBL study, asciminib may be better tolerated in this setting, allowing patients to resume full-dose intensity. Although the current data suggest asciminib has a relatively favorable safety profile, this view may evolve as long-term data become available, as the true incidence of toxicities such as arterial occlusive disease and pleural effusion may only emerge with prolonged treatment. Algorithms for toxicity management will be further refined with newly acquired data through current and subsequent clinical trials, and cumulative experience.
Given the superiority of asciminib over bosutinib in the third- and later-line settings, the potential value of asciminib in the second-line setting, beyond the specific scenario of patients with the T315I mutation, will need to be addressed. This is particularly relevant in the setting of treatment failure after frontline treatment with a second generation TKI. The relevant comparator here would usually be ponatinib, and a randomized trial will be needed to clarify the optimal treatment pathway. Clinical trials are currently underway to explore additional indications for asciminib. The largest, and arguably most important of these is the ASC4FIRST phase 3 study, which randomizes newly diagnosed patients with chronic-phase CML to asciminib 80 mg daily, vs a TKI selected at the physician’s discretion (NCT04971226).23 Combining an ATP-pocket binding TKI with an STAMP is also an attractive strategy: although the phase 1 CABL001X2101 study reported a promising efficacy signal when asciminib is combined with imatinib, nilotinib, or dasatinib, confirmatory data are necessary from well-designed studies to determine the optimal combinations. There are convincing in vitro data to suggest that asciminib, even at nanomolar concentrations, will restore ponatinib sensitivity in a compound mutant Y253H/T315I model. Crystallography data demonstrated that ponatinib docking in the ATP-binding pocket will stabilize asciminib binding in the myristoyl pocket, which in turn further stabilizes ponatinib binding.24 Clinical translation of such synergy through dose de-escalation may be of benefit in patients anticipated to have ponatinib-related toxicity. Such combinations may also be attractive in advanced-phase CML and Philadelphia-positive acute lymphoblastic leukemia, or in patients with kinase domain mutations, where increased potency of BCR::ABL1 inhibition is warranted.24,25 TKI/asciminib combinations are also being tested as consolidation therapy in the setting of treatment-free remission (NCT04838041).
With further clinical experience, the likelihood and modes of asciminib failure may also become apparent. Already, several resistance mechanisms are anticipated. Overexpression of drug efflux mechanisms may decrease intracellular concentration of all BCR::ABL inhibitors, including asciminib.26 Myristoyl pocket mutations have either been reported clinically (A337T, P465S, V468F)4,10 or anticipated from in vitro models (A344P).24 Combination treatments may potentially make it much less likely that a single mutation will cause treatment failure. In time, we will no doubt learn to use this promising new drug to its full potential. In the short term, it is incumbent on CML clinicians to carefully consider the relative merits of asciminib vs ponatinib in their most challenging cases.
Authorship
Contribution: D.T.Y., T.P.H., and N.S. gathered the data and wrote the manuscript.
Conflict-of-interest disclosure: T.P.H. receives research funding and honoraria from Novartis, BMS, and Takeda. N.S. receives research funding from Novartis. D.T.Y. receives research funding and honoraria from BMS and Novartis, and honoraria from BMS, Novartis, Takeda, Pfizer, and Amgen.
Correspondence: Timothy P. Hughes, Precision Medicine Theme, South Australian Health and Medical Research Institute, North Terrace, Adelaide, SA 5000, Australia; e-mail: tim.hughes@sahmri.com.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal