In this issue of Blood, two reports delineate tumor-specific factors associated with clinical responses to infusion of approved T-cell products genetically modified with a chimeric antigen receptor (CAR) targeting CD19 in patients with diffuse large B-cell lymphoma (DLBCL)1,2 (see figure). Jain et al comprehensively characterized the genomes of lymphoma tissue from patients who received CD19 CAR-T cells and report that genome-wide mutational signatures and patterns of structural alterations are associated with CAR-T cell response. Cherng et al evaluated circulating tumor DNA and show that a high focal copy number alterations (CNAs) score, denoting genomic instability, was the most significant pretreatment variable associated with poor response to CAR-T therapy or subsequent relapse.
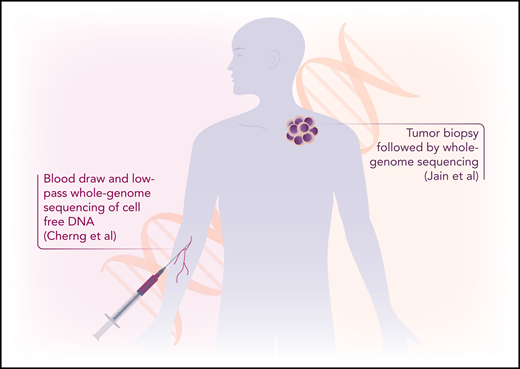
Two papers interrogate the lymphoma genome to learn causes of CAR-T failure in patients with diffuse B-cell lymphoma. Jain et al evaluate tumor biopsies with WGS, whereas Cherng et al perform low-pass WGS on circulating tumor DNA derived from peripheral blood. Professional illustration by Somersault18:24.
Two papers interrogate the lymphoma genome to learn causes of CAR-T failure in patients with diffuse B-cell lymphoma. Jain et al evaluate tumor biopsies with WGS, whereas Cherng et al perform low-pass WGS on circulating tumor DNA derived from peripheral blood. Professional illustration by Somersault18:24.
Autologous CD19 CAR-T cells have significant therapeutic benefit for patients with relapsed/refractory DLBCL, and 3 products have obtained Food and Drug Administration approval. Since the first approvals in 2017, the therapy has been used in several thousand patients, and “real-world” analyses confirmed the initial response rates of 50% to 80% reported in the studies that led to licensure.3-7 However, more than half of recipients experience relapse and disease progression, with prolonged disease responses in only ∼40%.3,7 Therefore, predictive factors for subsequent progression or relapse would be useful to identify patients who may benefit from combination therapies or additional consolidation strategies.
A number of studies have investigated the infused cell product or host immune system to identify factors associated with poor outcomes. These reports correlated serum inflammatory markers and T-cell exhaustion in either the CAR-19 products or the recipient with poor outcomes.8,9 The studies in this issue of Blood instead examined tumor-intrinsic factors that may lead to clinical CD19 CAR-T cell failures through whole-genome sequencing (WGS) of the tumor or low-pass WGS of cell-free DNA from plasma.
The first study from Jain et al at Moffitt Cancer Center and the University of Miami used WGS to assess tumor samples from 49 patients with DLBCL treated with axicabtagene ciloleucel and found that find that pretreatment presence of complex structural variants, APOBEC mutational signatures, and genomic damage from reactive oxygen species predicted CAR-19 resistance. In addition, the recurrent 3p21.31 chromosomal deletion containing the RHOA tumor suppressor was strongly enriched in patients who failed CAR-T therapy. Of note, reduced CD19 expression, which has been identified as a mechanism of failure in CD19 CAR-T cell therapy for acute lymphoblastic leukemia with tisagenlecleucel, did not affect responses in this study. One limitation of the WGS strategy used in this study is that it requires viable lymphoma tumor tissue and matched germline DNA.
Cell-free DNA provides an alternative strategy for evaluating tumor genetic changes10 and, in the second report, Cherng and colleagues at MD Anderson Cancer Center used a less-intensive assay requiring only a peripheral blood sample to evaluate CNAs. The authors undertook low-pass WGS of cell-free DNA from blood samples collected at the time of leukapheresis for product manufacture and analyzed samples from 122 patients (92% of whom received axicabtagene ciloleucel and 8% of whom received tisagenlecleucel). In multivariable analysis, Cherng et al found that a high focal CNAs score was the most significant pretreatment variable associated with inferior 3-month complete response rates and overall and progression-free survival. The study identified 34 unique focal CNAs, with deletion 10q23.3 leading to loss of FAS death receptor being the most prognostic for poor outcomes. By combining focal CNAs score with standard markers of increased tumor bulk (elevated lactate dehydrogenase and disease at >1 extranodal site), this study builds a risk model that may reliably stratify patients.
Both studies were retrospective and conducted at a single institution in 1 case and 2 institutions in the other, so require validation in other cohorts. In addition, both studies predominantly included patients who received axicabtagene ciloleucel. Whether these observations also apply to the other 2 commercial products thus remains to be seen. Nevertheless, these studies provide tumor-specific predictive factors that could be used to identify patients at high risk of relapse following CD19 CAR-T cells who may need additional therapies. Integrating these tumor-specific risk factors with other host and product factors that influence outcome may produce even stronger algorithms to predict success or failure.
Conflict-of-interest disclosure: The author has equity in Allovir and Marker Therapeutics, has served on advisory boards for Tessa Therapeutics, Novartis, Gilead, GSK, Kiadis, and Fresh Wind Biotechnologies, and received research support from Tessa Therapeutics and Kuur Therapeutics.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal