Key Points
Cell-free mtDNA is elevated in the peripheral blood and BM of patients with myeloma compared with those of healthy controls.
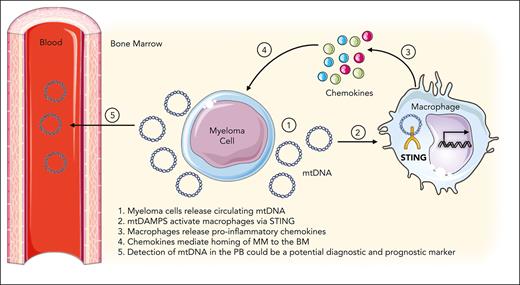
Myeloma-derived mtDNA remodels the BM microenvironment through its effect of STING activation in myeloma-associated macrophages.
Abstract
Mitochondrial damage–associated molecular patterns (mtDAMPs) include proteins, lipids, metabolites, and DNA and have various context-specific immunoregulatory functions. Cell-free mitochondrial DNA (mtDNA) is recognized via pattern recognition receptors and is a potent activator of the innate immune system. Cell-free mtDNA is elevated in the circulation of trauma patients and patients with cancer; however, the functional consequences of elevated mtDNA are largely undefined. Multiple myeloma (MM) relies upon cellular interactions within the bone marrow (BM) microenvironment for survival and progression. Here, using in vivo models, we describe the role of MM cell–derived mtDAMPs in the protumoral BM microenvironment and the mechanism and functional consequence of mtDAMPs in myeloma disease progression. Initially, we identified elevated levels of mtDNA in the peripheral blood serum of patients with MM compared with those of healthy controls. Using the MM1S cells engrafted into nonobese diabetic severe combined immunodeficient gamma mice, we established that elevated mtDNA was derived from MM cells. We further show that BM macrophages sense and respond to mtDAMPs through the stimulator of interferon genes (STING) pathway, and inhibition of this pathway reduces MM tumor burden in the KaLwRij-5TGM1 mouse model. Moreover, we found that MM-derived mtDAMPs induced upregulation of chemokine signatures in BM macrophages, and inhibition of this signature resulted in egress of MM cells from the BM. Here, we demonstrate that malignant plasma cells release mtDNA, a form of mtDAMPs, into the myeloma BM microenvironment, which in turn activates macrophages via STING signaling. We establish the functional role of these mtDAMP-activated macrophages in promoting disease progression and retaining MM cells in the protumoral BM microenvironment.
Introduction
Despite significant advances made in the treatment of multiple myeloma (MM), relapse from chemorefractory clones is inevitable, and most people diagnosed with MM will eventually die of the disease.1-3 These observations are attributable, in part, to the highly immunoprotective and chemoprotective nature of the bone marrow (BM) microenvironment, in which the malignant plasma cells proliferate and evolve. The BM microenvironment is a complex and highly organized tissue that physiologically supports the lifelong production of blood cells from hematopoietic stem cells (HSCs). HSCs reside in niches within the BM and are regulated through interactions with multiple cell types in the microenvironment, regulated by direct cell-cell contact, growth factors, cytokines, and chemokines.4-6 Macrophages are phagocytic immune cells present in most tissues that exhibit plasticity and heterogeneity depending on their location. Within the BM, macrophages are split into several distinct populations with different functions, including regulating HSC maintenance and quiescence, supporting red cell development, and negatively regulating the HSC pool in response to infection.5,7-9 In blood cancer, depletion of macrophages prevents engraftment of tumor cells in the BM. Moreover, tumor-associated macrophages seem to be more broadly and fundamentally involved in progression and metastasis, which across a range of cancers is linked to poorer clinical outcomes, in a diverse spectrum of tumor microenvironments.10,11 In myeloma, increased numbers of tumor-associated macrophages have been described in the BM of patients with MM with active disease,12,13 and these cells exert a number of protumoral functions, including chemotherapy resistance, tumor retention in the BM, angiogenesis, proliferation, and immunosuppression.12-14 Collectively, these studies show the protective effects of macrophages on myeloma; however, how and why macrophages maintain myeloma within the BM are not well understood.
Mitochondrial damage–associated patterns (mtDAMPs) include proteins, lipids, metabolites, and DNA and have various context-specific immunoregulatory functions.15,16 mtDAMPs have come into focus as mediators of inflammation, with mitochondrial DNA (mtDNA) being the most documented.16,17 Cell-free mtDNA contains islands of unmethylated cytosine-guanine dinucleotide (CpG) motifs, which are recognized via pattern recognition receptors and are potent activators of the innate immune system.18 mtDNA has been identified as a potential biomarker for cancer because of its ease of detection in blood and noninvasive sample collection.19 Elevated levels of mtDNA in the blood have been observed in many disease states, from depression to prostate cancer; however, most of the literature on this has been essentially observational. In myeloma, studies have shown mtDNA copy number is elevated in the presymptomatic state monoclonal gammopathy of undetermined significance and patients with MM;20 but to date, no studies have reported the functional consequences of increased mtDNA in MM. Furthermore, mtDNA has been shown to activate the stimulator of interferon genes (STING) via cyclic guanosine monophosphate–adenosine monophosphate synthase (cGAS).21,22 The cGAS-STING signaling pathway is a key mediator of inflammation caused by infection, cellular stress, or tissue damage. The cGAS-STING pathway detects and regulates the cellular response toward microbial and host-derived DNAs.23
To further elucidate the protumoral cellular interactions between malignant plasma cells and the BM microenvironment, here we present data that describe the role of MM cell–derived mtDAMPs in the BM microenvironment, their role in STING pathway activation in macrophages, and the mechanism and functional consequence of mtDAMPs on MM disease progression.
Materials and methods
Primary tissue collection
Primary MM samples were obtained from BM aspirates of patients with MM at the Norfolk and Norwich University Hospitals NHS Foundation Trust after informed consent and under the approval of the UK Health Research Authority and East of England Research Ethics Committee (Integrated Research Application System project ID: 33753). In addition, CD34+ cells were isolated from human cord blood from patients undergoing elective cesarean sections, and peripheral blood (PB) samples were collected from patients with myeloma or healthy controls after informed consent. Cell isolation was performed via density-gradient centrifugation of samples using Histopaque-1077 (Millipore Sigma). All cells were cultured in Dulbecco’s modified Eagle medium supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin and incubated at 37°C with 5% CO2 humidity.
Animals
Nonobese diabetic severe combined immunodeficient gamma mice (NOD. Cg-Prkdcscid Il2rgtm1Wjl/SzJ [NSG]) and C57BL/KaLwRij were purchased from Jackson Laboratory (Bar Harbor, ME). C57BL/6J and CBA mice were purchased from Charles River Laboratories (Wilmington, MA). Mice were housed under specific pathogen-free conditions in a containment level 3 disease modeling unit. All animal work was carried out in accordance with the Animal Scientific Procedures Act 1986, following UK Home Office regulations. Mice of both genders were used in experiments and were between 6 and 12 weeks of age.
NSG mice were treated with 25 mg/kg busulfan intraperitoneally every day for 3 days before the IV tail vein injection of 2 × 105 MM1s cells. The cells were allowed to engraft over a period of 3 weeks. Blood samples were taken by tail vein bleed, and the serum was analyzed by real-time quantitative polymerase chain reaction (qPCR) to analyze the presence of mtDNA. Engraftment was observed by flow cytometry through analysis of human CD38+ cells in the BM.
C57BL/KaLwRij mice were tail vein–injected with 1 × 106 5TGM1–green fluorescent protein (GFP)/luciferase (LUCI) cells. Throughout any experiment, in vivo bioluminescence imaging (Bruker In Vivo Xtreme) was used to monitor tumor progression. Blood samples were taken by tail vein bleed at various intervals for downstream analysis. At the end point, BM was extracted for further analysis.
In vivo STING inhibition migration assay
C57BL/KaLwRij mice were engrafted with 1 × 106 5TGM1(GFP+ LUCI+) cells and engrafted for 34 days. On day 34, PB samples were taken before treatment with H-151 (750 nM) administered intraperitoneally after 24 hours, another PB sample was taken to be analyzed by flow cytometry for 5TGM1(GFP+) presence.
In vivo macrophage depletion
C57BL/KaLwRij mice were engrafted with 1 × 106 murine 5TGM1(GFP+ LUCI+) cells via IV injection. Thirteen days postengraftment, mice were intraperitoneally injected with 150 μL of either control or clodronate-loaded liposomes (Clophosome-A, Stratech, United Kingdom). After 24 hours, the mice were euthanized, and the BM and PB were isolated for analysis. Flow cytometry was used to analyze the BM macrophage population (GR1−, CD115LO/INT, F4/80+) and 5TGM1(GFP+) content in the PB and BM to assess 5TGM1 cell homing.
Statistics
GraphPad Prism, version 9 for macOS (GraphPad Software), was used to compare statistical significance. Because of the variability in the data, a statistical comparison of in vivo work was performed without the assumption of normal distribution. Therefore, nonparametric statistical tests were used. For statistical comparison between groups of 2, a Mann-Whitney U test was performed. A Kruskal-Wallis test followed by Dunn multiple comparisons was carried out for the comparison of groups >2. The Wilcoxon-matched pairs signed rank test was used for statistical analysis between matched samples. Differences among groups were considered significant when P < .05.
Study approval
All animal work used in this study was carried out in accordance with regulations set by the UK Home Office and the Animal Scientific Procedures Act 1986. Nonmalignant and malignant hematopoietic cells were collected at the Norfolk and Norwich University Hospitals NHS Foundation Trust. Studies were performed after approval from the UK Health Research Authority research ethics committee (reference 07/H0310/146).
Results
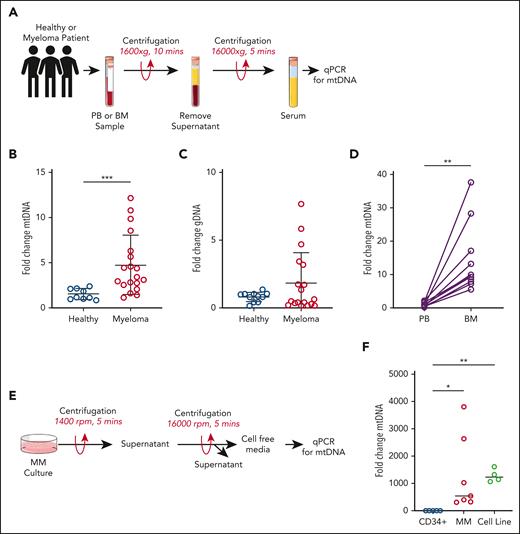
Cell-free mtDNA is elevated in MM
To initially identify and quantify mtDAMPs in MM, we used cell-free mtDNA as a surrogate marker. BM and PB samples were collected from newly diagnosed patients with MM (Table 1). PB samples were also collected from healthy controls. Cell-free serum was obtained as described in Figure 1A, and qPCR was used to detect and quantify the presence of mtDNA. Figure 1B shows mtDNA to be elevated in the PB serum of patients with MM compared with that of controls (Figure 1B), with no significant change in genomic DNA levels between MM and healthy controls (Figure 1C). Furthermore, comparing mtDNA levels in BM serum to matched PB serum from patients with MM showed a significant increase in cell-free mtDNA in the BM (Figure 1D), suggesting that the majority of cell-free mtDNA associated with MM is maintained within the BM microenvironment. To further determine if MM was associated with increased cell-free mtDNA, we analyzed culture media from 3 control cell types (human CD34+ cells, B cells, and monocytes), primary CD138+ plasma cells, and immortalized MM cell lines (Figure 1E). CD34+ cells, B cells (CD19+), and monocytes (CD14+) were used as controls, as the frequency of plasma cells in healthy individuals is extremely low, and it is therefore difficult to isolate sufficient plasma cells for a direct comparison in these experiments. Results confirm that cell-free mtDNA is associated with myeloma (Figure 1F; supplemental Figure 1A-B, available on the Blood website). These data show that cell-free mtDNA is elevated in MM.
Data on patients with myeloma
| Patient no. . | Age, y . | Sex . | Diagnosis . |
|---|---|---|---|
| MM1 | 59 | F | Myeloma (s) |
| MM2 | 74 | F | Myeloma (s) |
| MM3 | 72 | F | Myeloma (s) |
| MM4 | 80 | M | Myeloma (a) |
| MM5 | 37 | M | Myeloma (s) |
| MM6 | 79 | F | Myeloma (s) |
| MM7 | 69 | M | Myeloma (a) |
| MM8 | 57 | M | Myeloma (s) |
| MM9 | 66 | F | Myeloma (s) |
| MM10 | 82 | F | Myeloma (a) |
| MM11 | 74 | M | Myeloma (a) |
| MM12 | 53 | F | Myeloma (s) |
| MM13 | 64 | M | Myeloma (s) |
| MM14 | 73 | M | Myeloma (s) |
| MM15 | 75 | F | Myeloma (s) |
| MM16 | 55 | M | Myeloma (s) |
| MM17 | 75 | F | Myeloma (s) |
| MM18 | 86 | M | Myeloma (a) |
| MM19 | 83 | F | Myeloma (a) |
| MM20 | 72 | F | Myeloma (s) |
| MM21 | 62 | M | Myeloma (a) |
| MM22 | 49 | F | Myeloma (a) |
| MM23 | 80 | F | Myeloma (s) |
| MM24 | 63 | F | Myeloma (s) |
| MM25 | 66 | F | Myeloma (a) |
| MM26 | 60 | F | Myeloma (a) |
| Patient no. . | Age, y . | Sex . | Diagnosis . |
|---|---|---|---|
| MM1 | 59 | F | Myeloma (s) |
| MM2 | 74 | F | Myeloma (s) |
| MM3 | 72 | F | Myeloma (s) |
| MM4 | 80 | M | Myeloma (a) |
| MM5 | 37 | M | Myeloma (s) |
| MM6 | 79 | F | Myeloma (s) |
| MM7 | 69 | M | Myeloma (a) |
| MM8 | 57 | M | Myeloma (s) |
| MM9 | 66 | F | Myeloma (s) |
| MM10 | 82 | F | Myeloma (a) |
| MM11 | 74 | M | Myeloma (a) |
| MM12 | 53 | F | Myeloma (s) |
| MM13 | 64 | M | Myeloma (s) |
| MM14 | 73 | M | Myeloma (s) |
| MM15 | 75 | F | Myeloma (s) |
| MM16 | 55 | M | Myeloma (s) |
| MM17 | 75 | F | Myeloma (s) |
| MM18 | 86 | M | Myeloma (a) |
| MM19 | 83 | F | Myeloma (a) |
| MM20 | 72 | F | Myeloma (s) |
| MM21 | 62 | M | Myeloma (a) |
| MM22 | 49 | F | Myeloma (a) |
| MM23 | 80 | F | Myeloma (s) |
| MM24 | 63 | F | Myeloma (s) |
| MM25 | 66 | F | Myeloma (a) |
| MM26 | 60 | F | Myeloma (a) |
Cell-free mtDNA is elevated in myeloma. (A) Schematic of the serum extraction process. DNA was extracted from patient PB serum and analyzed via TaqMan qPCR to assess mtDNA and genomic DNA content. (B) Fold change in serum mtDNA in healthy controls (n = 9) vs patients with myeloma (n = 21). (C) Fold change in serum genomic DNA. (D) mtDNA changes from matched PB and BM serum of patients with MM (n = 11). Data indicate mean ± standard deviation (SD). Statistics are presented as Mann-Whitney U test. (E) Schematic of the cell-free media extraction process. DNA was extracted from cell-free media extracted from cells in culture and analyzed via TaqMan qPCR. (F) Fold change in mtDNA in the media of control CD34+ cells (n = 6), MM patient-derived cells (n = 6), and immortalized MM cell lines (n = 4). Data indicate mean ± SD. Statistics are presented as Wilcoxon test. ∗∗P < .01; ∗∗∗P < .001.
Cell-free mtDNA is elevated in myeloma. (A) Schematic of the serum extraction process. DNA was extracted from patient PB serum and analyzed via TaqMan qPCR to assess mtDNA and genomic DNA content. (B) Fold change in serum mtDNA in healthy controls (n = 9) vs patients with myeloma (n = 21). (C) Fold change in serum genomic DNA. (D) mtDNA changes from matched PB and BM serum of patients with MM (n = 11). Data indicate mean ± standard deviation (SD). Statistics are presented as Mann-Whitney U test. (E) Schematic of the cell-free media extraction process. DNA was extracted from cell-free media extracted from cells in culture and analyzed via TaqMan qPCR. (F) Fold change in mtDNA in the media of control CD34+ cells (n = 6), MM patient-derived cells (n = 6), and immortalized MM cell lines (n = 4). Data indicate mean ± SD. Statistics are presented as Wilcoxon test. ∗∗P < .01; ∗∗∗P < .001.
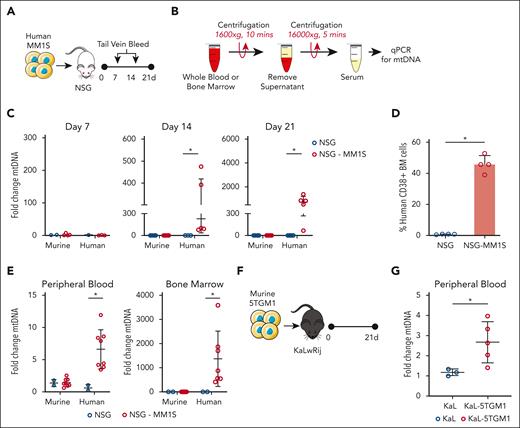
Increased mtDNA in MM originates from the malignant plasma cells
To ascertain the origin of cell-free mtDNA detected at increased levels in the serum and BM of patients with MM, we next studied the blood of immunocompromised NSG mice engrafted with the immortalized human MM cell line MM1S. PB samples were taken once a week over the course of 3 weeks, and serum was extracted for mtDNA analysis (Figure 2A-B). The serum was analyzed by qPCR for human and murine mtDNA. The fold change in mtDNA at day 7 was used as a baseline to assess mtDNA change over the next 21 days. We observe no change in the levels of murine mtDNA in both control and engrafted mice over time (Figure 2C). However, human mtDNA levels first became detectable on day 14 and increased further by day 21 in MM1S-engrafted mice. The human origin of the mtDNA was confirmed further with a second human mitochondrial target (supplemental Figure 2A). We detected no human mtDNA in control mice at the same time points. Engraftment of the MM1S cells in mice was confirmed by measuring the percentage of human CD38+ cells in the BM by flow cytometry (Figure 2D). To confirm the MM1S-NSG model results, we repeated the experiment described and engrafted NSG mice with MM1S cells. For this experiment, we analyzed the levels of mtDNA in both the PB and BM serum 21 days after the injection of MM1s cells. We observed an elevated level of human mtDNA in the PB serum, which was significantly enhanced in the BM serum (Figure 2E). Together with the data from Figure 1D, this shows that BM serum in patients with myeloma and MM mouse models has increased levels of myeloma-derived mtDNA compared with PB serum.
mtDNA is released by MM cells. (A-B) Schematic of experimental design. Human MM1s (2 × 106) were injected IV into busulfan (25 mg/kg)–pretreated NSG mice. PB samples were taken via IV tail vein bleed at 7 and 14 days after engraftment. (C) Cell-free serum was extracted from PB via centrifugation, and DNA was extracted and analyzed via qPCR for the presence of murine and human mtDNA, using human and mouse ND1 primers. (D) Percentage of human CD38+ cells in the BM of control NSG mice (n = 4) and NSG-MM1s mice (n = 4). (E) In a separate experiment, human MM1s (2 × 106) were injected IV into busulfan (25 mg/kg)–pretreated NSG mice. At 21 days, PB and BM samples were taken, cell-free serum was taken, and DNA was extracted and analyzed via qPCR for mtDNA. (F-G) A total of 1 × 106 murine 5TGM1(GFP+ LUCI+) cells were injected into C57BL/KaLwRij mice. Mice were euthanized at 21 days, and PB serum samples were extracted and analyzed via qPCR for mtDNA. Data indicate mean ± SD. Statistics are presented as Mann-Whitney U test. ∗P < .05.
mtDNA is released by MM cells. (A-B) Schematic of experimental design. Human MM1s (2 × 106) were injected IV into busulfan (25 mg/kg)–pretreated NSG mice. PB samples were taken via IV tail vein bleed at 7 and 14 days after engraftment. (C) Cell-free serum was extracted from PB via centrifugation, and DNA was extracted and analyzed via qPCR for the presence of murine and human mtDNA, using human and mouse ND1 primers. (D) Percentage of human CD38+ cells in the BM of control NSG mice (n = 4) and NSG-MM1s mice (n = 4). (E) In a separate experiment, human MM1s (2 × 106) were injected IV into busulfan (25 mg/kg)–pretreated NSG mice. At 21 days, PB and BM samples were taken, cell-free serum was taken, and DNA was extracted and analyzed via qPCR for mtDNA. (F-G) A total of 1 × 106 murine 5TGM1(GFP+ LUCI+) cells were injected into C57BL/KaLwRij mice. Mice were euthanized at 21 days, and PB serum samples were extracted and analyzed via qPCR for mtDNA. Data indicate mean ± SD. Statistics are presented as Mann-Whitney U test. ∗P < .05.
Finally, to exclude the possibility that these data represented a cross-species or an unexpected NSG model phenomenon, we used an isogeneic murine model of MM. In similar experiments using the KaLwRij-5TGM1 isogenic mouse model of myeloma, we confirmed the presence of elevated levels of mtDNA in the PB of animals with MM (Figure 2F-G). To determine if the increase in mtDNA is specific to myeloma or also occurs in other hematological malignancies, we used our established mouse model of acute myeloid leukemia (AML).10 The BM serum of mice engrafted with MN1 cells did not show an increase in mtDNA (supplemental Figure 2B-C). Together, these data suggest that malignant plasma cells are the source of increased levels of mtDNA in MM, which originate in the tumor microenvironment and egress into the circulation.
MM induces STING-mediated activation of macrophages via mtDAMPs
To address the functional consequence of myeloma-derived mtDNA on the BM microenvironment, we performed studies on macrophages from the tumor microenvironment. We and others have recently shown that macrophages and effector cells react to mtDAMPs via the STING pathway in the contexts of inflammation,22 ischemia, and AML.10 Accordingly, we analyzed a panel of genes associated with STING pathway activation in macrophages isolated from 5TGM1(GFP+ LUCI+)-engrafted KaLwRij mice (Figure 3A). Engraftment of 5TGM1 in the KaLwRij mice was determined by GFP-expressing cells in the BM (Figure 3B). The sorting strategy for the BM macrophages is shown in Figure 3C and as previously described.10 Real-time qPCR showed increased expression of GBP2, IFIT3, and IRF7 in BM macrophages fluorescence-activated cell sorted (FACS) purified from 5TGM1-engrafted mice (Figure 3D). To determine if STING pathway activation in macrophages was directly related to secreted components from MM, we cultured BM-derived macrophages (BMDMs) from KaLwRij mice with 5TGM1-conditioned media (CM) that had undergone centrifugation to remove cells and large extracellular vesicles (EVs) and further filtered through a 100 kDa ultracentrifugal filter to remove small EVs and any other remaining large proteins (Figure 3E). These centrifugation steps to remove large and small EVs were included as others have shown that whole functional mitochondria can be packaged in EVs and transferred between cells.24,25 Removal of the EVs therefore allowed us to purely focus on the effect of cell-free mtDNA. Results show that STING pathway genes were upregulated in BMDM treated with CM from 5TGM1 (Figure 3F). This suggests that MM cells release small cell-free molecules that trigger STING activation in macrophages.
MM induces STING-mediated activation of macrophages via mtDAMPs. (A) Schematic of experimental design. Murine 5TGM1 cells (1 × 106) were injected into KaLwRij mice. (B) At 28 days, BM samples were taken and analyzed for 5TGM1 engraftment by GFP+ cells. (C) BM macrophages were FACS-purified (GR1−, F4/80+, CD115int), and RNA was extracted for analysis by quantitative real-time PCR (qRT-PCR). (D) Relative gene expression of GBP2, IFIT3, and IRF7 in FACS-purified macrophages. (E) Large and small EV were removed from 5TGM1-CM by centrifugation and filtering through a 100 kDa Amicon Ultra-15 Centrifugal Filter. (F) BMDM were then treated with filtered CM for 6 hours followed by RNA extraction for analysis using qRT-PCR of GBP2, IFIT3, and IRF7. Relative gene expression of GBP2, IFIT3, and IRF7 in BMDMs treated with mtDAMPs (10 μg) (G) or CpG ODN 1826 (n = 4) (H). Data indicate mean ± SD. Statistics are presented as Mann-Whitney U test. (I) BMDM were pretreated with STING inhibitor H-151 (10 μM) for 2 hours before treatment with either CpG ODN 1826 or mtDAMPs (10 μg) for 6 hours. RNA was extracted and gene expression was analyzed via qRT-PCR. Relative gene expression of GBP2, IFIT3, and IRF7 in control untreated BMDMs, CpG (n = 4). Statistics are presented as 2-way analysis of variance with Šidák post hoc multiple comparisons test. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. FITC, fluorescein isothiocyanate; FSC, forward scatter; SSC, side scatter.
MM induces STING-mediated activation of macrophages via mtDAMPs. (A) Schematic of experimental design. Murine 5TGM1 cells (1 × 106) were injected into KaLwRij mice. (B) At 28 days, BM samples were taken and analyzed for 5TGM1 engraftment by GFP+ cells. (C) BM macrophages were FACS-purified (GR1−, F4/80+, CD115int), and RNA was extracted for analysis by quantitative real-time PCR (qRT-PCR). (D) Relative gene expression of GBP2, IFIT3, and IRF7 in FACS-purified macrophages. (E) Large and small EV were removed from 5TGM1-CM by centrifugation and filtering through a 100 kDa Amicon Ultra-15 Centrifugal Filter. (F) BMDM were then treated with filtered CM for 6 hours followed by RNA extraction for analysis using qRT-PCR of GBP2, IFIT3, and IRF7. Relative gene expression of GBP2, IFIT3, and IRF7 in BMDMs treated with mtDAMPs (10 μg) (G) or CpG ODN 1826 (n = 4) (H). Data indicate mean ± SD. Statistics are presented as Mann-Whitney U test. (I) BMDM were pretreated with STING inhibitor H-151 (10 μM) for 2 hours before treatment with either CpG ODN 1826 or mtDAMPs (10 μg) for 6 hours. RNA was extracted and gene expression was analyzed via qRT-PCR. Relative gene expression of GBP2, IFIT3, and IRF7 in control untreated BMDMs, CpG (n = 4). Statistics are presented as 2-way analysis of variance with Šidák post hoc multiple comparisons test. ∗P < .05; ∗∗P < .01; ∗∗∗P < .001. FITC, fluorescein isothiocyanate; FSC, forward scatter; SSC, side scatter.
To determine whether this was a specific mtDNA or a broader mtDAMP response, we treated BMDMs with mtDAMPs obtained from mouse liver or CpG oligodeoxynucleotide (ODN) 1826 (a molecular mimic of mtDNA) and looked at gene expression of STING activation genes. The purity of the mtDAMPs used was confirmed using PCR for mtDNA and genomic DNA, which showed that only mtDNA could be detected in the mtDAMPs used (supplemental Figure 3A). Although mtDAMP treatment resulted in the upregulation of all STING genes (Figure 3G), CpG treatment failed to fully activate the STING-related genes, with only Irf7 being significantly upregulated (Figure 3H). To determine if raised levels of mtDNA in patients with myeloma also correlate with changes in STING genes, monocytes were isolated from the PB of patients newly diagnosed with myeloma and healthy controls. The results show that STING genes were upregulated in monocytes collected from the PB of patients with myeloma compared with those of controls (supplemental Figure 3B). Finally, to confirm that this response was mediated through STING, we used the STING inhibitor H-151 to block the mtDAMP-induced STING activation pathway. Figure 3I shows that treatment with H-151 inhibits mtDAMP-induced STING activation genes in BMDM. The data suggest that mtDAMPs released from myeloma cells induce a STING response in BM macrophages.
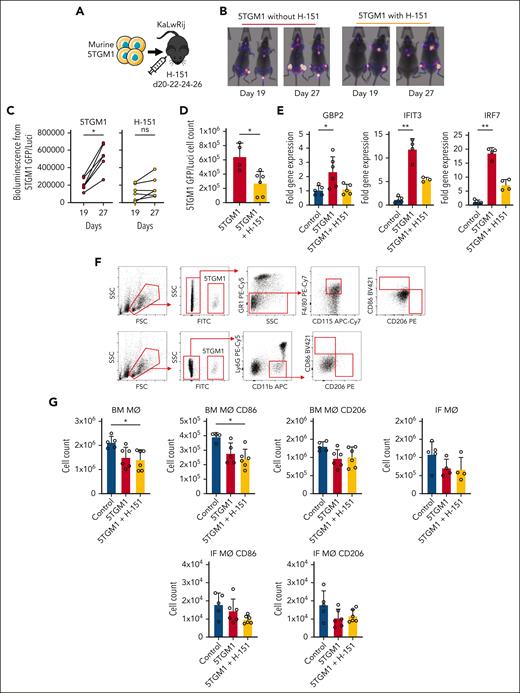
MM progression is attenuated by STING inhibition
To understand the tumor-specific functional consequences of STING activation by MM-derived mtDAMPs in the microenvironment, KaLwRij mice were engrafted with 5TGM1(GFP+LUCI+) cells, and the tumor was allowed to establish for 19 days, before 1 week of treatment with STING inhibitor H-151 (Figure 4A). The animals were imaged before and after treatment, and bioluminescent images show reduced tumor progression in the H-151–treated group from days 19 to 27, despite similar engraftment in the 2 treatment groups on day 19 (Figure 4B-C; supplemental Figure 4A-B). The animals were then euthanized, and tumor volume was measured by flow cytometry for GFP+ cells. When compared with control 5TGM1-engrafted animals, H-151-treated animals had reduced tumor volume (Figure 4D). BM was isolated from euthanized animals, and BM macrophages were FACS-purified and analyzed for GBP2, IFIT3, and IRF7 gene expression. When compared with control animals, BM macrophages from H-151–treated animals had a trend toward decreased expression of STING markers, GBP2, IRF7, and IFIT3 (Figure 4E). Flow cytometry was also used to analyze the BM-resident and infiltrating macrophage cell populations in the tumor microenvironment. We found that there were no significant differences in the size of these populations or the polarization of M1 (CD86+) or M2 (CD206+) macrophages with STING inhibition (Figure 4F-G). Finally, 5TGM1 cells were treated with 10 μM of H-151 for 24 hours, and cell survival was then measured using a CellTiter Glo Assay (supplemental Figure 4C). The results show that H-151 has no direct effect on 5TGM1 survival.
MM progression is attenuated by STING inhibition. (A) 5TGM1 cells (1 × 106) transduced with rLV.EF1.mCherry-Mito9 lentivirus (5TGM1LUCI+) were injected into KaLwRij mice. (B) In vivo imaging of mice engrafted with 5TGM1(GFP+ LUCI+) on days 19 and 27, representing before and after H-151 (750 nM) treatment, respectively. (C) Bioluminescence, before and after treatment, was quantified using ImageJ (n = 6 in each group). Data indicate mean ± SD. Statistics presented as Wilcoxon test. (D) Mice were euthanized at 27 days. (E) BM was harvested for flow cytometry 5TGM1 engraftment and FACS-purified for BM macrophages. RNA was extracted for analysis by qRT-PCR of GBP2, IFIT3, and IRF7. (F) BM cells were analyzed for GR1, F4/80, CD115, LY6G, CD11b, CD86, and CD206 expression and used to identify resident BM macrophages (BM MΦ) (GR1−, CD115lo/int, and F4/80+) and MM-infiltrating macrophages (IF MΦ) (Ly6G− and CD11b+). The gating strategy is shown. (G) Cell counts of BM MΦ and IF MΦ from treated mice. Data indicate mean ± SD. Statistics presented as Kruskal-Wallis test with Dunn post hoc multiple comparisons test. ∗P < .05; ∗∗P < .01.
MM progression is attenuated by STING inhibition. (A) 5TGM1 cells (1 × 106) transduced with rLV.EF1.mCherry-Mito9 lentivirus (5TGM1LUCI+) were injected into KaLwRij mice. (B) In vivo imaging of mice engrafted with 5TGM1(GFP+ LUCI+) on days 19 and 27, representing before and after H-151 (750 nM) treatment, respectively. (C) Bioluminescence, before and after treatment, was quantified using ImageJ (n = 6 in each group). Data indicate mean ± SD. Statistics presented as Wilcoxon test. (D) Mice were euthanized at 27 days. (E) BM was harvested for flow cytometry 5TGM1 engraftment and FACS-purified for BM macrophages. RNA was extracted for analysis by qRT-PCR of GBP2, IFIT3, and IRF7. (F) BM cells were analyzed for GR1, F4/80, CD115, LY6G, CD11b, CD86, and CD206 expression and used to identify resident BM macrophages (BM MΦ) (GR1−, CD115lo/int, and F4/80+) and MM-infiltrating macrophages (IF MΦ) (Ly6G− and CD11b+). The gating strategy is shown. (G) Cell counts of BM MΦ and IF MΦ from treated mice. Data indicate mean ± SD. Statistics presented as Kruskal-Wallis test with Dunn post hoc multiple comparisons test. ∗P < .05; ∗∗P < .01.
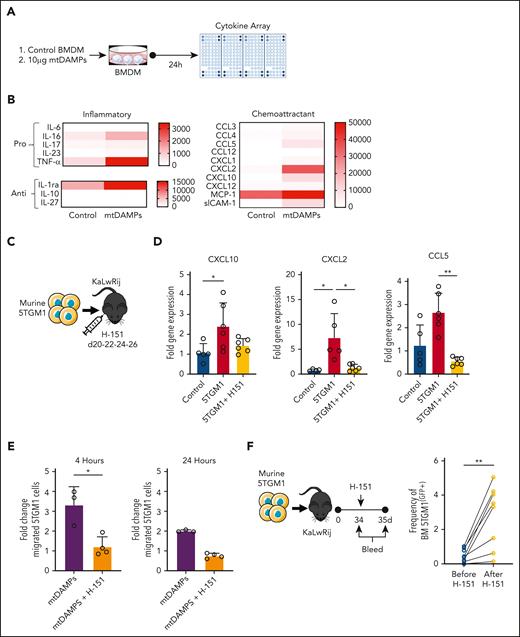
MM-derived mtDAMPs induce a migratory signature in BM macrophages
To investigate the secretome changes in macrophages exposed to MM-derived mtDAMPs, we treated BMDMs with myeloma-derived mtDAMPs and assayed the cell supernatant using a Proteome Profiler Mouse Cytokine Array (Figure 5A). As predicted, we detected an upregulation in several cytokines, including those associated with inflammation and STING pathway activation. However, in addition, we observed a cluster of chemoattractant cytokines (CCL5, CXCL2, and CXCL10) that were also upregulated by mtDAMP-treated macrophages (Figure 5B). MM is primarily a BM disease, with clonal plasma cells rarely detected in the PB at leukemic levels, as reflected by the clinical observation that plasma cell leukemia represents <1% of all cases of MM.26 Therefore, we hypothesized a role for MM-derived mtDAMPs in promoting the retention of malignant plasma cells in the BM via activation of the STING pathway in macrophages. To address this, we first determined in vivo whether these chemokines were upregulated in FACS-purified BM macrophages from 5TGM1-engrafted KaLwRij mice and whether this upregulation could be inhibited by H-151 (Figure 5C). When compared with control BM macrophages from KaLwRij animals, macrophages from 5TGM1-engrafted animals had increased CCL5, CXCL2, and CXCL10 messenger RNA expression. Moreover, STING inhibition significantly reduced the expression of CXCL2 and CCL5 (Figure 5D). Next, we used an in vitro migration assay in which CM from BMDM were treated with mtDAMPs with and without STING inhibition with H-151. Results show that CM from mtDAMP-treated macrophages increased the migration of 5TGM1 cells, whereas when STING signaling was inhibited, cell migration was reduced (Figure 5E). Inhibitors for CCL5 (anti-CCL5 antibody), CXCL10-CXCR3 (AMG487), and CXCL2-CXCR2 (SB225002) were used to determine the role of each pathway in the retention of MM. Inhibition of CCL5 significantly reduced mtDAMP-induced migration (supplemental Figure 5A). Moreover, STING inhibition in 5TGM1-engrafted KaLwRij mice resulted in an increased frequency of 5TGM1 cells in the BM (Figure 5F). Finally, to establish the role of macrophages in the retention of myeloma in the BM marrow, we used clodronate liposomes to deplete macrophages in the 5TGM1-KaLwRij–engrafted model and then assessed myeloma egress from the BM (supplemental Figure 5B). The frequency of macrophages in the BM was reduced in clodronate-treated animals (supplemental Figure 5C). When compared with control liposome-treated KaLwRij animals from 5TGM1-engrafted animals, clodronate liposome treatment showed increased levels of 5TGM1 cells in the PB and reduced tumor volume in the BM (supplemental Figure 5D). Together, these data show that myeloma cells release mtDAMPs into the BM, which activate resident macrophages to produce a chemotaxis signature that results in myeloma BM retention.
Myeloma-derived mtDAMPs induce a migratory signature in BM macrophages. (A) Schematic of experimental design. BMDMs were cultured with mtDAMPs (10 μg) for 24 hours. BMDM cell supernatant was cleared of cellular debris by centrifugation before cytokine array analysis (n = 3). (B) Quantification of cytokine array results segmented into inflammatory and chemoattractant-related factors. (C) Schematic of experimental design. Murine 5TGM1(GFP+ LUCI+) cells (1 × 106) were injected into C57BL/KaLwRij mice. On days 20, 22, 24, and 26 after engraftment, mice were injected intraperitoneally with either 200 μL H-151 (750 nM) or vehicle. Mice were euthanized at 27 days; BM was harvested, and myeloma-associated macrophages were isolated via FACS purification. (D) Relative gene expression of CXCL10, CXCL2, and CCL5 (n = 6 in each treatment group). Data indicate mean ± SD. Statistics presented as Kruskal-Wallis test with Dunn post hoc multiple comparisons test. (E) BMDMs were cultured with either mtDAMPs (10 μg) alone or mtDAMPs and H-151 (10 μM) for 24 hours. BMDM-CM was cleared of cellular debris by centrifugation and placed into the bottom chamber of the transwell. 5TGM1(GFP+) cells were placed in the upper chamber and migrated 5TGM1(GFP+) cells were counted at 4 and 24 hours. Data indicate mean ± SD. Statistics are presented as Mann-Whitney U test. (F) Murine 5TGM1(GFP+ LUCI+) cells (1 × 106) were injected into C57BL/KaLwRij mice. At 34 days after engraftment, PB samples were taken by tail vein bleed, then the mice were injected IP with H-151 (750 nM). On day 35, posttreatment blood samples were taken and mice were euthanized. The PB samples were analyzed for 5TGM1(GFP+) cell presence via flow cytometry (n = 8 mice). Data indicate mean ± SD. Statistics are presented as Wilcoxon test. ∗∗P < .01; ∗P < .05.
Myeloma-derived mtDAMPs induce a migratory signature in BM macrophages. (A) Schematic of experimental design. BMDMs were cultured with mtDAMPs (10 μg) for 24 hours. BMDM cell supernatant was cleared of cellular debris by centrifugation before cytokine array analysis (n = 3). (B) Quantification of cytokine array results segmented into inflammatory and chemoattractant-related factors. (C) Schematic of experimental design. Murine 5TGM1(GFP+ LUCI+) cells (1 × 106) were injected into C57BL/KaLwRij mice. On days 20, 22, 24, and 26 after engraftment, mice were injected intraperitoneally with either 200 μL H-151 (750 nM) or vehicle. Mice were euthanized at 27 days; BM was harvested, and myeloma-associated macrophages were isolated via FACS purification. (D) Relative gene expression of CXCL10, CXCL2, and CCL5 (n = 6 in each treatment group). Data indicate mean ± SD. Statistics presented as Kruskal-Wallis test with Dunn post hoc multiple comparisons test. (E) BMDMs were cultured with either mtDAMPs (10 μg) alone or mtDAMPs and H-151 (10 μM) for 24 hours. BMDM-CM was cleared of cellular debris by centrifugation and placed into the bottom chamber of the transwell. 5TGM1(GFP+) cells were placed in the upper chamber and migrated 5TGM1(GFP+) cells were counted at 4 and 24 hours. Data indicate mean ± SD. Statistics are presented as Mann-Whitney U test. (F) Murine 5TGM1(GFP+ LUCI+) cells (1 × 106) were injected into C57BL/KaLwRij mice. At 34 days after engraftment, PB samples were taken by tail vein bleed, then the mice were injected IP with H-151 (750 nM). On day 35, posttreatment blood samples were taken and mice were euthanized. The PB samples were analyzed for 5TGM1(GFP+) cell presence via flow cytometry (n = 8 mice). Data indicate mean ± SD. Statistics are presented as Wilcoxon test. ∗∗P < .01; ∗P < .05.
Discussion
MM represents a spectrum of genetically, molecularly, and phenotypically incurable tumors that evolve and progress over time.27 Even at early and asymptomatic stages of the disease, genetic and molecular diversity28 and a compromised immune microenvironment29 can be identified. Furthermore, in relapse, there is an accumulation of additional genetic mutations, which activate oncogenic pathways and affect drug sensitivity.30 Despite these observations demonstrating MM to be a set of highly genetically diverse,31 molecularly distinct,32 clinically varied,33 and clonally unstable34 disease entities, almost without exception, all MM tumor subtypes originate, proliferate, and relapse within the BM microenvironment. This observation of a shared microenvironmental dependency for such a heterogenous spectrum of disease implies a fundamental role for the nonmalignant cells of the BM niche in MM pathophysiology and evolution. The commonality of this observation also leads to speculation that novel therapeutic strategies targeting the tumor microenvironment interactions may have broad clinical efficacy despite such broad molecular and cellular diversity in these cancer subtypes.
Macrophages play a fundamental role in normal BM homeostasis. Moreover, in the tumor microenvironment, the interaction of the macrophages, tumor cells, and stromal cells enables and sustains most of the hallmarks of cancer.35 In MM, macrophages are abundant and have been shown to affect the initiation and progression of the disease,36 via a number of mechanisms of action, including homing of malignant cells to BM, plasma cell proliferation, drug resistance, neovascularization, and immunosuppression.37 Specifically, invasion of tumor-supporting macrophages has been shown to correlate with low survival in patients with MM.38 Here, we identified that STING-mediated activation of BM macrophages enhances MM progression by secreting migratory chemokines that retain MM in the protective BM. Other studies have shown that in the 5TGM1-KaLwRij model, depletion of macrophages, using clodronate liposomes, before injection of 5TGM1 slows MM engraftment.38 Moreover, they show that clodronate treatment decreases CXCL12 expression in BM cells, suggesting that this treatment is inhibiting the homing of MM to the BM.38 Another study by the same group shows that the inhibition of CCL3/CCR1 interactions between MM and BM stromal cells causes the egress of MM from the BM.39 Collectively, these studies describe the importance of macrophages in the retention of MM in the BM, which supports survival, proliferation, and chemotherapy resistance, and highlight the potential clinical value of drugs that interfere with these processes.
The presence of cell-free mtDNA has been found in the serum of patients with various cancer types.40 Several groups have reported the diagnostic value of mtDNA in plasma, serum, or whole blood as a biomarker of solid malignancies, including lung, breast, and testicular cancer.19,41-43 However, the understanding of the source of this mtDNA and its pathophysiological impact on cancer progression is less well established. Here, we observed that mtDNA is elevated in cell-free serum samples from patients with MM. Moreover, through animal modeling, we showed that the mtDNA detected in the serum originates from the tumor cell. We also observe increased cell-free mtDNA in the PB serum of patients with myeloma compared with that of healthy controls, which is further elevated in the BM. Furthermore, we showed that the increased levels of cell-free mtDNA correlated with an upregulation of the STING-related genes in macrophages both in vivo and in vitro, as well as in PB monocytes from patients with MM. As we could not exclude that the isolated mtDNA contained trace amounts of mtDAMPs, we used the mtDNA mimic, CpG ODN 1826, to determine if the response was specific to mtDNA or a broader mtDAMP response. Although CpG ODN mimics cell-free mtDNA, the concentration of CpG repeats is much higher than that contained in the mtDNA and therefore may have increased the functional response observed. Moreover, the use of CpG ODN 1826 at the concentrations used may not represent the physiological response observed in vivo. However, using mtDMAPs also has its limitations, as it is unclear which components of mtDAMPs include proteins, lipids, metabolites, and DNA and have various context-specific immunoregulatory functions. Cell-free mtDNA is recognized via pattern recognition receptors and is a potent activator of the innate immune system. Cell-free mtDNA is elevated in the circulation of trauma patients and patients with cancer; however, the functional consequences of elevated mtDNA are largely undefined. MM relies upon cellular interactions within the BM microenvironment for survival and progression. Here, using in vivo models, we describe the role of MM cell–derived mtDAMPs in the protumoral BM microenvironment and the mechanism and functional consequence of mtDAMPs in myeloma disease progression. Initially, we identified elevated levels of mtDNA in the PB serum of patients with MM compared with that of healthy controls. Using the MM1S cells engrafted into NSG mice, we established that elevated mtDNA was derived from MM cells. We further show that BM macrophages sense and respond to mtDAMPs through the STING pathway, and inhibition of this pathway reduces MM tumor burden in the KaLwRij-5TGM1 mouse model. Moreover, we found that MM-derived mtDAMPs induced the upregulation of chemokine signatures in BM macrophages, and inhibition of this signature resulted in the egress of MM cells from the BM. Here, we demonstrate that malignant plasma cells release mtDNA, a form of mtDAMPs, into the myeloma BM microenvironment, which in turn activates macrophages via STING signaling. We establish the functional role of these mtDAMP-activated macrophages in promoting disease progression and retaining MM cells in the protumoral BM microenvironment of the DAMP is responsible for the response observed, and this would be particularly important to allow targeting of the mtDAMP response as a therapeutic intervention. Mechanistically, we show that myeloma-derived mtDAMPs rather than CpG ODN promoted protumoral microenvironment remodeling by activating BM macrophage chemotaxis signatures through the activation of the STING pathway. Specifically, inhibition of mtDAMP-induced STING activation promotes the egress of myeloma from the supporting BM microenvironment.
Targeting the cGAS-STING pathway has been shown to play an important role in many preclinical models of inflammation, chronic diseases, and cancer. In cancer, we and others have shown that STING activation can significantly extend survival in in vivo models of AML.10,44 In this manuscript, describing the role of macrophages in the progression of MM, STING inhibition extends the survival of MM, which on the face of it appears contradictory to the results obtained in AML and other cancer models.45 In some contexts, macrophages in the tumor microenvironment have been found to promote AML progression. Specifically, displacement of resident macrophages or invasion of tumor-supporting macrophages has been shown to correlate with low survival in patients with AML. In our previously published data on AML, LAP-dependent activation of STING increased the phagocytosis of AML cells.10 In mouse melanoma cells and several other cell lines, the anthracycline drug doxorubicin induced the activation of STING. Accordingly, the consequences of STING activation/inhibition are not only tissue- and cell-specific but will also likely have different disease-specific outcomes within the spectrum of BM disorders.
Macrophages play a number of important and often disease-specific roles in the tumor microenvironment, and given the association between high macrophage infiltration and poor survival in most cancers, identifying intratumoral macrophage-specific therapeutic targets remains an important goal.46 Here, we identify a functional role for mtDNA in the myeloma BM microenvironment through its effect on STING activation in myeloma-associated macrophages.
Acknowledgments
The authors thank the Norwich Research Park, the Rosetrees Trust, the Big C, and the National Health Service. The authors also thank Allyson Tyler and Karen Ashurst from the Laboratory Medicine Department at the Norfolk and Norwich University Hospital for technical assistance, Rachel Stanley at the Norwich Research Park Biorepository (United Kingdom) for supporting primary tissue collection, and the team at the Disease Modelling Unit of the University of East Anglia for assistance with the in vivo studies.
This work was supported by a Sir Henry Welcome Postdoctoral Fellowship (213731/Z/18/Z) (E.E.W.), Rosetrees Trust (J.A.M.), a Wellcome Trust Clinical Research Fellowship (220534/Z/20/Z) (C.H.), the Medical Research Council project (MR/T02934X/1) (S.A.R.). The authors acknowledge support by a grant from the Biotechnology and Biological Sciences Research Council, part of UK Research and Innovation’s Core Capability (grant BB/CCG1720/1); the National Capability (BBS/E/T/000PR9816); and the Norfolk and Norwich University Hospital Charitable Fund.
Authorship
Contribution: A.J., C.H., K.M.B., and S.A.R. designed the research; J.A.M., K.H., D.J.F.-S., J.J.M., C.H., R.M., E.E.W., and A.J. performed the research; A.J., S.A.R., and C.H. carried out in vivo work; K.M.B., C.H., and R.D.S. provided essential reagents and knowledge; and A.J., C.H., K.M.B., and S.A.R. wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Stuart A. Rushworth, Department of Molecular Haematology, Norwich Medical School, University of East Anglia, Norwich Research Park, Norwich NR4 7UQ, United Kingdom; e-mail: s.rushworth@uea.ac.uk; and Kristian M. Bowles, Department of Molecular Haematology, Norwich Medical School, University of East Anglia, Norwich Research Park, Norwich NR4 7UQ, United Kingdom; e-mail: k.bowles@uea.ac.uk.
References
Author notes
∗A.J. and C.H. are joint first authors.
†K.M.B. and S.A.R. are joint corresponding authors.
All relevant data are included in the article and the data supplement. Data are available on request from the corresponding authors, Stuart A. Rushworth (s.rushworth@uea.ac.uk) and Kristian M. Bowles (k.bowles@uea.ac.uk).
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal