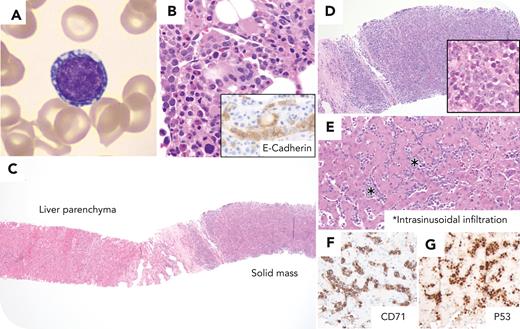
A 52-year-old woman with a history of sickle cell disease (SCD) and myelodysplastic neoplasm with biallelic TP53 inactivation (MDS-biTP53) presented with worsening cytopenias, disseminated intravascular coagulation, and concern about disease progression. Peripheral blood smear review demonstrated rare immature-appearing cells with stippled chromatin and cytoplasmic vacuoles (panel A; 100× objective, Wright-Giemsa stain). Bone marrow biopsy showed persistent myelodysplastic syndrome with erythroid predominance (20% pronormoblasts), multilineage dysplasia, and no increase in myeloblasts (panel B, 50× objective, and E-cadherin immunohistochemical stain [inset], 100× objective). Magnetic resonance imaging demonstrated 2 liver lesions in the left hepatic lobe, measuring 2.4 and 1.7 cm in greatest dimension. Liver core biopsy showed intrasinusoidal and nodular aggregates of neoplastic cells with vesicular chromatin, distinct nucleoli, and small amounts of cytoplasm (panel C, 4× objective; panel D, 10× objective; panel D inset, 50× objective; and panel E, 20× objective, hematoxylin and eosin stain). The neoplastic infiltrate expressed CD71, P53 (panels F-G; 20× objective), E-cadherin, CD33 (subset), CD45 (large-subset), and CD117 (subset); neoplastic cells were negative for CD3, CD20, CD30, CD34, myeloperoxidase, lysozyme, pan cytokeratin, and S-100. A diagnosis of erythroblastic sarcoma (EBS) was established.
EBS is an extremely rare tumor composed of erythroid precursors. The suggested etiology of the current case includes blast transformation from extramedullary hematopoiesis in a patient with concomitant SCD not receiving hydroxyurea and myeloid neoplasm with TP53 abnormalities.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal