Key Points
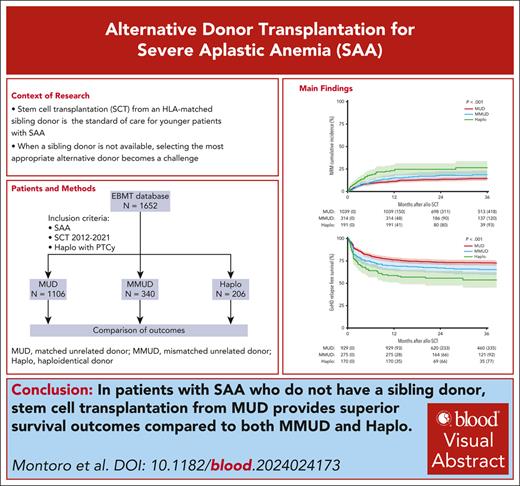
SCT from MUD offers superior survival outcomes for severe aplastic anemia compared with both MMUD and Haplo SCT.
The decision between an MMUD and Haplo donor in the absence of an available MUD remains uncertain.
Visual Abstract
Selecting the most suitable alternative donor becomes challenging in severe aplastic anemia (SAA) when a matched sibling donor (MSD) is unavailable. We compared outcomes in patients with SAA undergoing stem cell transplantation (SCT) from matched unrelated donors (MUD) (n = 1106), mismatched unrelated donors (MMUD) (n = 340), and haploidentical donors (Haplo) (n = 206) registered in the European Society for Blood and Marrow Transplantation database (2012-2021). For Haplo SCT, only those receiving posttransplant cyclophosphamide for graft-versus-host disease (GVHD) prophylaxis were included. Median age was 20 years, and the median time from diagnosis to transplantation 8.7 months. Compared with MUD, MMUD (hazard ratio [HR], 2.93; 95% confidence interval [CI], 1.52-5.6) and Haplo (HR, 5.15; 95% CI, 2.5-10.58) showed significantly higher risks of primary graft failure. MUD had lower rates of acute GVHD compared with MMUD and Haplo (grade 2-4: 13%, 22%, and 19%, respectively; P < .001; grade 3-4: 5%, 9%, and 7%, respectively; P = .028). The 3-year nonrelapse mortality rate was 14% for MUD, 19% for MMUD, and 27% for Haplo (P < .001), whereas overall survival and GVHD and relapse-free survival (GRFS) rates were 81% and 73% for MUD, 74% and 65% for MMUD, and 63% and 54% for Haplo, respectively (P < .001). In addition to donor type, multivariable analysis identified other factors associated with GRFS such as patient age, performance status, and interval between diagnosis and transplantation. For patients with SAA lacking an MSD, our findings support MUDs as the preferable alternative donor option. However, selecting between an MMUD and Haplo donor remains uncertain and requires further exploration.
Medscape Continuing Medical Education online

In support of improving patient care, this activity has been planned and implemented by Medscape, LLC and the American Society of Hematology. Medscape, LLC is jointly accredited with commendation by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Medscape, LLC designates this Journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to 1.0 MOC points in the American Board of Internal Medicine's (ABIM) Maintenance of Certification (MOC) program. Participants will earn MOC points equivalent to the amount of CME credits claimed for the activity. It is the CME activity provider's responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.
All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives; (2) study the education content; (3) take the post-test with a 75% minimum passing score and complete the evaluation at https://www.medscape.org/journal/blood; and (4) view/print certificate. For CME questions, see page 343.
Disclosures
CME questions author Laurie Barclay, freelance writer and reviewer, Medscape, LLC, declares no competing financial interests.
Learning Objectives
Upon completion of this activity, participants will:
Compare engraftment, graft failure, second transplant, and graft-versus-host disease from different donor sources for patients with severe aplastic anemia (SAA) who lack a sibling donor, based on a study of patients with SAA included in the SAAWP-EBMT registry (2012-2021)
Compare nonrelapse mortality, cause of death, and survival from different donor sources for patients with SAA who lack a sibling donor, based on a study of patients with SAA included in the SAAWP-EBMT registry (2012-2021)
Identify clinical implications of comparative outcomes from different donor sources for patients with SAA who lack a sibling donor, based on a study of patients with SAA included in the SAAWP-EBMT registry (2012-2021)
Release date: July 18, 2024; Expiration date: July 18, 2025
Introduction
Stem cell transplantation (SCT) from an HLA–matched sibling donor (MSD) is considered the standard of care for younger patients with severe aplastic anemia (SAA).1,2 For patients lacking a suitable MSD, matched unrelated donors (MUDs) have increasingly been used for patients with SAA who do not respond to immunosuppressive therapy (IST).3-6 However, a significant number of patients with SAA who require SCT are unable to access a fully HLA-MUD or experience delays in finding one. In such cases, apart from unrelated cord blood, which has primarily been used in pediatric and young adults, alternative options, such as mismatched unrelated donors (MMUDs)3,7-10 and haploidentical family donors (Haplo),11-22 have been explored.
The current body of research on the efficacy and safety of SCT for SAA, comparing MUDs, MMUDs, and Haplo in the context of SAA is sparse and involves a limited number of patients.23-27 Consequently, reaching solid conclusions regarding the optimal alternative donor transplant choice for patients with SAA remains a challenging task. To address this knowledge gap, we have conducted an extensive study using the Severe Aplastic Anemia Working Party (SAAWP) of the European Society for Blood and Marrow Transplantation (EBMT) registry.
This study aims to compare transplant outcomes across the 3 donor types, MUDs, MMUDs, and Haplo donors, for patients with SAA. Although MUD and MMUD transplants primarily use in vivo T-cell depletion (TCD) with antithymocyte globulin (ATG) or alemtuzumab, for the haploidentical cohort, we restricted the analysis to those who received posttransplant cyclophosphamide (PT-Cy), reflecting its prevailing usage in contemporary practice. With a substantial patient population and access to comprehensive registry data, our study endeavors to provide valuable evidence to assist the optimal transplant approach for patients with SAA.
Patients and methods
Study design and data source
Data were collected from the SAAWP database of the EBMT, a collaborative effort comprising over 600 transplantation centers that are required to report all consecutive SCTs and follow-up once a year. Patients prospectively provided signed informed consent for both data collection through the ProMISe system and any subsequent a posteriori analysis. The study was conducted in accordance with the Declaration of Helsinki and was approved by the scientific committee of the SAAWP of the EBMT.
Inclusion criteria
The study included all consecutive patients reported to the EBMT with a diagnosis of SAA who underwent their first SCT from either a MUD, MMUD, or Haplo donor between January 2012 and December 2021. For the purposes of the study, we focused on transplants from Haplo donors who received PT-Cy as prophylaxis for graft-versus-host disease (GVHD). The patients’ HLA typing was performed at high-level resolution for 10 loci, including HLA-A, -B, -C, -DRB1, and -DQB1. A full MUD was defined as a 10/10 allele match, whereas haploidentical donors had at least 2 HLA mismatches, and MMUDs had at least 1 HLA mismatch. Patients who had undergone cord blood transplantation or ex vivo TCD were excluded from the study.
End points and definitions
All outcomes in the study are defined from the time of first SCT. The primary end point of this study was GVHD and relapse-free survival (GRFS). Secondary end points included engraftment, graft failure, acute and chronic GVHD (cGVHD), nonrelapse mortality (NRM), event-free survival (EFS), and overall survival (OS). GRFS was defined as survival without disease relapse (including primary and secondary graft failure [SGF]) and grade 3 to 4 or chronic extensive GVHD. OS was defined as the time between the date of transplantation and death. Events considered in EFS were primary and SGF, second transplantation, relapse, and death, whichever occurred first. NRM was defined as death from any cause, without a preceding return of marrow to its status before transplantation or graft failure.
Myeloid engraftment was defined as the first day of an absolute neutrophil count of 0.5 × 109/L lasting for at least 3 consecutive days. Platelet engraftment was defined as the first day of a platelet count of 20 × 109/L or higher, without transfusion support for 7 consecutive days. Primary graft failure (PGF) was defined as failure to achieve myeloid engraftment by day +42, and SGF was defined as a decrease of absolute neutrophil count to less than 0.5 × 109/L after initial myeloid engraftment, but not related to infection or drug toxicity. Acute GVHD (aGVHD) and cGVHD were defined and graded according to standard criteria.28-30
Statistical analysis
OS, EFS, and GRFS were estimated using the Kaplan–Meier product limit estimation method, and differences in subgroups were assessed by the log-rank tests. Median follow-up was determined using the reverse Kaplan–Meier method. Competing risks methods were used to analyze the cumulative incidences of NRM, aGVHD grades 2 to 4 and grades 3 to 4, cGVHD, and primary and SGF. NRM and graft failure were considered together with second transplantation and death as competing events. For aGVHD and cGVHD, as well as platelet and neutrophil recovery, competing events included relapse/graft failure, second transplantation, and death, whichever occurred first. Subgroup differences in competing risks analyses were assessed by Gray’s test.
Multivariable Cox proportional hazards regression was applied to investigate the simultaneous impact of multiple covariates on the OS and GRFS. Cox cause–specific hazards models were used for the outcomes aGVHD grade 2 to 4 and cGVHD, and a logistic regression model was applied to investigate PGF before day +42. All models include an identical predefined covariate constellation: donor type (MMUD, Haplo, or MUD), donor age at transplantation (in decades), patient age at transplantation (in decades), Karnofsky score (<90 vs 90-100), donor–recipient sex match (female donor to male patient vs other combinations), patient cytomegalovirus serostatus (positive vs negative), total body irradiation (TBI) (yes vs no), stem cell source (peripheral blood vs bone marrow), and interval from diagnosis to transplantation (years). A potential center effect was accommodated for by the inclusion of a random effect for center, a gamma frailty for center in the Cox regression models, and a random intercept for center in the logistic model of PGF. Only center effects with nonzero variance are retained.
Continuous variables are presented as median and interquartile range (IQR), and subgroup differences were tested using Kruskal–Wallis tests. Categorical variables are presented as percentages within the group of patients with available data, with subgroup differences tested using the χ2 test.
In all analyses, complete-case analysis was applied. All univariable estimates of survival and cumulative incidences and multivariable hazard ratios (HRs) are reported with corresponding 95% confidence intervals (CIs) in parentheses. All P values were 2-sided, and P < .05 was considered significant. Statistical analyses were performed in R, version 3.6.0 (R Core Team, Vienna, Austria), using the packages “survival,” “prodlim,” and “cmprsk.”
Results
Patient and transplantation characteristics
Patient and transplantation characteristics of the overall population and according to donor type are summarized in Table 1. Briefly, a total of 1652 patients were included in the study, of which 1106 (67%) underwent transplantation from MUD, 340 (21%) from MMUD, and 206 (12%) from Haplo. Median age of patients was 20 years (IQR, 11.2-40.1), and 953 (58%) were male. The median time from diagnosis to transplantation was 8.7 months (IQR, 4.8-16.6).
Patient and transplant characteristics in the whole cohort and stratified by donor type
| Characteristic . | Total N = 1652 . | MUD N = 1106 . | MMUD N = 340 . | Haplo N = 206 . | P value . |
|---|---|---|---|---|---|
| Median age at transplant, y (IQR) | 20.4 (11.2-40.1) | 21 (11.7-42.3) | 17.8 (10.4-34.8) | 20.9 (10.7-37.5) | .016 |
| Sex, n (%) | .756 | ||||
| Male | 953 (58) | 631 (57) | 201 (59) | 121 (59) | |
| Female | 699 (42) | 475 (43) | 139 (41) | 85 (41) | |
| KPS, n (%) | .319 | ||||
| ≥90 | 1116 (73) | 753 (74) | 232 (74) | 131 (67) | |
| <90 | 412 (27) | 267 (26) | 80 (26) | 65 (33) | |
| Missing | 124 | 86 | 28 | 10 | |
| Year of transplant, median (IQR) | 2017 (2014-2019) | 2017 (2014-2019) | 2016 (2014-2019) | 2018 (2017-2020) | <.001 |
| Interval diagnosis to transplant in months, median (IQR) | 8.7 (4.8-16.6) | 8.1 (4.3-14.3) | 10.4 (6.2-19.6) | 9.2 (4.8-18.5) | <.001 |
| Donor–recipient CMV serostatus, n (%) | <.001 | ||||
| Positive/positive | 740 (46) | 436 (40) | 164 (50) | 140 (72) | |
| Positive/negative | 97 (6) | 66 (6) | 20 (6) | 11 (6) | |
| Negative/positive | 397 (25) | 277 (26) | 96 (30) | 24 (12) | |
| Negative/negative | 370 (23) | 304 (28) | 46 (14) | 20 (10) | |
| Missing | 48 | 23 | 14 | 11 | |
| HCT-CI, n (%) | .522 | ||||
| Low | 894 (69) | 597 (69) | 178 (69) | 119 (70) | |
| Intermediate | 201 (16) | 126 (15) | 48 (18) | 27 (16) | |
| High | 194 (15) | 136 (16) | 33 (13) | 25 (14) | |
| Missing | 363 | 247 | 81 | 35 | |
| Median age of donor, y (range) | 29.4 (23.6-36.8) | 28.2 (23.4-34.4) | 29.5 (23.6-37.5) | 36.3 (27.2-45.9) | <.001 |
| Female donor to male recipient, n (%) | 254 (16) | 129 (12) | 71 (21) | 54 (26) | <.001 |
| TBI in conditioning, n (%) | <.001 | ||||
| Yes | 495 (31) | 253 (23) | 103 (31) | 139 (69) | |
| No | 1122 (69) | 834 (77) | 224 (69) | 64 (31) | |
| Missing | 35 | 19 | 13 | 3 | |
| TBI dose, n (%) | <.001 | ||||
| 2 Gy | 430 (87) | 239 (94) | 87 (84) | 104 (75) | |
| >2 Gy | 65 (13) | 14 (6) | 16 (16) | 35 (25) | |
| Conditioning regime,∗n (%) | <.001 | ||||
| Flu + Cy + ATG + TBI | 287 (18) | 156 (14) | 56 (17) | 75 (36.5) | |
| Flu + Cy + ATG | 402 (24) | 291 (26) | 84 (25) | 27 (13) | |
| Flu + Cy + TBI | 131 (8) | 56 (5) | 22 (6) | 53 (26) | |
| Flu + Cy + alemtuzumab | 416 (25) | 334 (30) | 82 (24) | 0 (0) | |
| Cy + ATG | 117 (7) | 95 (9) | 21 (6) | 1 (0.5) | |
| Other | 299 (18) | 174 (16) | 75 (22) | 50 (24) | |
| Stem cell source, n (%) | <.001 | ||||
| Bone marrow | 979 (59) | 666 (60) | 202 (59) | 111 (54) | |
| Peripheral blood | 663 (40) | 439 (40) | 136 (40) | 88 (43) | |
| BM + PB | 10 (1) | 1 (0) | 2 (1) | 7 (3) | |
| Serotherapy for in vivo TCD, n (%) | <.001 | ||||
| ATG | 1017 (63) | 685 (63) | 208 (64) | 124 (61) | |
| Alemtuzumab | 470 (29) | 372 (34) | 95 (29) | 3 (1) | |
| No serotherapy | 136 (8) | 35 (3) | 23 (7) | 78 (38) | |
| Missing | 29 | 14 | 14 | 1 | |
| GVHD prophylaxis, n (%) | <.001 | ||||
| CNI + MTX | 708 (43) | 540 (49) | 168 (49) | 0 (0) | |
| PT-Cy based | 274 (17) | 36 (3) | 32 (9) | 206 (100) | |
| Others | 670 (40) | 530 (48) | 140 (42) | 0 (0) |
| Characteristic . | Total N = 1652 . | MUD N = 1106 . | MMUD N = 340 . | Haplo N = 206 . | P value . |
|---|---|---|---|---|---|
| Median age at transplant, y (IQR) | 20.4 (11.2-40.1) | 21 (11.7-42.3) | 17.8 (10.4-34.8) | 20.9 (10.7-37.5) | .016 |
| Sex, n (%) | .756 | ||||
| Male | 953 (58) | 631 (57) | 201 (59) | 121 (59) | |
| Female | 699 (42) | 475 (43) | 139 (41) | 85 (41) | |
| KPS, n (%) | .319 | ||||
| ≥90 | 1116 (73) | 753 (74) | 232 (74) | 131 (67) | |
| <90 | 412 (27) | 267 (26) | 80 (26) | 65 (33) | |
| Missing | 124 | 86 | 28 | 10 | |
| Year of transplant, median (IQR) | 2017 (2014-2019) | 2017 (2014-2019) | 2016 (2014-2019) | 2018 (2017-2020) | <.001 |
| Interval diagnosis to transplant in months, median (IQR) | 8.7 (4.8-16.6) | 8.1 (4.3-14.3) | 10.4 (6.2-19.6) | 9.2 (4.8-18.5) | <.001 |
| Donor–recipient CMV serostatus, n (%) | <.001 | ||||
| Positive/positive | 740 (46) | 436 (40) | 164 (50) | 140 (72) | |
| Positive/negative | 97 (6) | 66 (6) | 20 (6) | 11 (6) | |
| Negative/positive | 397 (25) | 277 (26) | 96 (30) | 24 (12) | |
| Negative/negative | 370 (23) | 304 (28) | 46 (14) | 20 (10) | |
| Missing | 48 | 23 | 14 | 11 | |
| HCT-CI, n (%) | .522 | ||||
| Low | 894 (69) | 597 (69) | 178 (69) | 119 (70) | |
| Intermediate | 201 (16) | 126 (15) | 48 (18) | 27 (16) | |
| High | 194 (15) | 136 (16) | 33 (13) | 25 (14) | |
| Missing | 363 | 247 | 81 | 35 | |
| Median age of donor, y (range) | 29.4 (23.6-36.8) | 28.2 (23.4-34.4) | 29.5 (23.6-37.5) | 36.3 (27.2-45.9) | <.001 |
| Female donor to male recipient, n (%) | 254 (16) | 129 (12) | 71 (21) | 54 (26) | <.001 |
| TBI in conditioning, n (%) | <.001 | ||||
| Yes | 495 (31) | 253 (23) | 103 (31) | 139 (69) | |
| No | 1122 (69) | 834 (77) | 224 (69) | 64 (31) | |
| Missing | 35 | 19 | 13 | 3 | |
| TBI dose, n (%) | <.001 | ||||
| 2 Gy | 430 (87) | 239 (94) | 87 (84) | 104 (75) | |
| >2 Gy | 65 (13) | 14 (6) | 16 (16) | 35 (25) | |
| Conditioning regime,∗n (%) | <.001 | ||||
| Flu + Cy + ATG + TBI | 287 (18) | 156 (14) | 56 (17) | 75 (36.5) | |
| Flu + Cy + ATG | 402 (24) | 291 (26) | 84 (25) | 27 (13) | |
| Flu + Cy + TBI | 131 (8) | 56 (5) | 22 (6) | 53 (26) | |
| Flu + Cy + alemtuzumab | 416 (25) | 334 (30) | 82 (24) | 0 (0) | |
| Cy + ATG | 117 (7) | 95 (9) | 21 (6) | 1 (0.5) | |
| Other | 299 (18) | 174 (16) | 75 (22) | 50 (24) | |
| Stem cell source, n (%) | <.001 | ||||
| Bone marrow | 979 (59) | 666 (60) | 202 (59) | 111 (54) | |
| Peripheral blood | 663 (40) | 439 (40) | 136 (40) | 88 (43) | |
| BM + PB | 10 (1) | 1 (0) | 2 (1) | 7 (3) | |
| Serotherapy for in vivo TCD, n (%) | <.001 | ||||
| ATG | 1017 (63) | 685 (63) | 208 (64) | 124 (61) | |
| Alemtuzumab | 470 (29) | 372 (34) | 95 (29) | 3 (1) | |
| No serotherapy | 136 (8) | 35 (3) | 23 (7) | 78 (38) | |
| Missing | 29 | 14 | 14 | 1 | |
| GVHD prophylaxis, n (%) | <.001 | ||||
| CNI + MTX | 708 (43) | 540 (49) | 168 (49) | 0 (0) | |
| PT-Cy based | 274 (17) | 36 (3) | 32 (9) | 206 (100) | |
| Others | 670 (40) | 530 (48) | 140 (42) | 0 (0) |
P values were obtained using the χ2 test for categorical variables and the Kruskal–Wallis test for continuous data.
BM, bone marrow; CMV, cytomegalovirus; CNI, calcineurin inhibitors; Cy, cyclophosphamide; FCA, fludarabine, cyclophosphamide, ATG; Flu, fludarabine; HCT-CI, hematopoietic cell transplantation-comorbidity index; MTX, methotrexate; PB, peripheral blood.
The most frequently used doses were: Flu 30 mg/m2 × 4 (days −6 to −3), Cy 300 mg/m2 or 30 mg/kg × 4 (days −6 to −3), ATG 3.75 mg/kg × 2 (days −4 to −3), and TBI 2 Gy (day −1) (FCA TBI regimen); Flu 30 mg/m2 × 4 (days −6 to −3), Cy 300 mg/m2 × 4 (days −6 to −3), and ATG (5-10 mg/kg) (FCA regimen); Flu 30 mg/m2 × 4 (days −6 to −2), Cy 14.5 mg/kg × 2 (days −7 to −6), and TBI 2 Gy (day −1) (Baltimore protocol); Flu 30 mg/m2 (days −6 to −3), Cy 300 mg/m2 × 4 (days −6 to −3), and alemtuzumab 0.2 mg/kg × 5 (days −7 to −3) (FCC regimen), and Cy 50 mg/kg × 4 (days −5 to −2) and ATG (5-10 mg/kg). ATG schedule and dosage are presented with thymoglobulin (Genzyme, a Sanofi company).
Patients in the MMUD cohort were significantly younger than those in the MUD and Haplo cohorts (P = .016), and the time from diagnosis to transplantation was longer than in those in the MUD and Haplo cohorts (10.4 months vs 8.1 months in MUD and 9.2 months in Haplo; P < .001). Differences in sex, Karnofsky performance status (KPS), and hematopoietic cell transplantation-comorbidity index risk were not statistically significant. Regarding transplantation characteristics, Haplo-SCT recipients received more frequently peripheral blood grafts (43% vs 40% each in MUD and MMUD; P < .001) and TBI-based conditioning regimens (68% vs 31% in MMUD and 23% in MUD; P < .001). Furthermore, Haplo-SCT donors were significantly older (median, 36 vs 29 years in MMUD and 28 years in MUD; P < .001), more often cytomegalovirus seropositive (77% vs 56% in MMUD and 46% in MUD; P < .001), and a higher proportion of female donors were used for male recipients (26% vs 21% in MMUD and 12% in MUD; P < .001). Most patients in the MMUD group had only 1 antigen mismatch (85.9%). The use of ATG serotherapy for in vivo TCD was similar among the 3 cohorts (range, 61-64). In contrast, the use of alemtuzumab was virtually limited to the MUD and MMUD groups, whereas PT-Cy was exclusively used in the Haplo cohort. Unfortunately, information regarding patients who underwent IST before transplantation was available in only a quarter of patients (428; 26%). Among these, 202 (66%), 54 (76%), and 41 (82%) had received previous IST in the MUD, MMUD, and Haplo cohorts, respectively.
Engraftment
The median time to neutrophil engraftment was 19 days (95% CI, 19-20), 20 days (95% CI, 19-21), and 18 days (95% CI, 18-20) for MUD, MMUD, and Haplo, respectively. The cumulative incidence of neutrophil recovery at 28 days was 85% (95% CI, 83-87) for MUD, 84% (95% CI, 80-88) for MMUD, and 75% (95% CI, 69-81) for Haplo (P = .03) (Table 2).
Univariable analysis of transplant outcomes according to donor type
| Outcome . | MUD . | MMUD . | Haploidentical . | P value . |
|---|---|---|---|---|
| Myeloid engraftment, CI at 28 d (%) | 85 (83-87) | 84 (80-88) | 75 (69-81) | .033 |
| Platelet engraftment, CI at 100 d (%) | 88 (86-91) | 82 (78-87) | 72 (65-78) | <.001 |
| PGF, CI at 42 d (%) | 3 (2-4) | 7 (4-10) | 13 (8-17) | <.001 |
| SGF, 3-y CI (%) | 4 (3-5) | 4 (2-7) | 2 (0-4) | .4 |
| aGVHD grades 2-4, CI at 100 d (%) | 13 (11-15) | 22 (17-27) | 19 (13-24) | <.001 |
| aGVHD grades 3-4, CI at 100 d (%) | 5 (3-6) | 9 (5-12) | 7 (3-10) | .028 |
| Overall cGVHD, 3-y CI (%) | 18 (16-21) | 20 (15-25) | 18 (11-25) | .79 |
| Extensive cGVHD, 3-y CI (%) | 7 (6-9) | 7 (4-10) | 6 (1-10) | .6 |
| NRM, 3-y CI (%) | 14 (12-17) | 19 (14-23) | 27 (19-34) | <.001 |
| EFS, 3-y CI (%) | 73 (71-76) | 63 (58-69) | 55 (47-63) | <.001 |
| OS, 3-y CI (%) | 81 (79-84) | 74 (69-79) | 63 (54-71) | <.001 |
| GRFS, 3-y CI (%) | 73 (70-76) | 65 (60-71) | 54 (45-62) | <.001 |
| Outcome . | MUD . | MMUD . | Haploidentical . | P value . |
|---|---|---|---|---|
| Myeloid engraftment, CI at 28 d (%) | 85 (83-87) | 84 (80-88) | 75 (69-81) | .033 |
| Platelet engraftment, CI at 100 d (%) | 88 (86-91) | 82 (78-87) | 72 (65-78) | <.001 |
| PGF, CI at 42 d (%) | 3 (2-4) | 7 (4-10) | 13 (8-17) | <.001 |
| SGF, 3-y CI (%) | 4 (3-5) | 4 (2-7) | 2 (0-4) | .4 |
| aGVHD grades 2-4, CI at 100 d (%) | 13 (11-15) | 22 (17-27) | 19 (13-24) | <.001 |
| aGVHD grades 3-4, CI at 100 d (%) | 5 (3-6) | 9 (5-12) | 7 (3-10) | .028 |
| Overall cGVHD, 3-y CI (%) | 18 (16-21) | 20 (15-25) | 18 (11-25) | .79 |
| Extensive cGVHD, 3-y CI (%) | 7 (6-9) | 7 (4-10) | 6 (1-10) | .6 |
| NRM, 3-y CI (%) | 14 (12-17) | 19 (14-23) | 27 (19-34) | <.001 |
| EFS, 3-y CI (%) | 73 (71-76) | 63 (58-69) | 55 (47-63) | <.001 |
| OS, 3-y CI (%) | 81 (79-84) | 74 (69-79) | 63 (54-71) | <.001 |
| GRFS, 3-y CI (%) | 73 (70-76) | 65 (60-71) | 54 (45-62) | <.001 |
Univariable outcomes of engraftment, graft failure, acute and cGVHD, NRM, OS, EFS, GVHD, and GRFS, stratified by donor type. Kaplan–Meier estimates of OS, EFS, and GRFS are given, with group differences tested by log-rank tests, and cumulative incidences are given for all other outcomes, with group differences tested by the Gray test. All estimates are reported with 95% CIs in parentheses.
The median time to platelet engraftment was 21 days (20-21), 23 days (21-26), and 29 days (26-32) for MUD, MMUD, and Haplo cohorts, respectively. Platelet engraftment at 60 and 100 days was 86% (95% CI, 84-89) and 88% (95% CI, 86-91) for MUD, 81% (95% CI, 76-86) and 82% (95% CI, 78-87) for MMUD, and 69% (95% CI, 62-76) and 72% (95% CI, 65-78) for Haplo (P < .001), respectively (Table 2).
Graft failure and second transplantation
PGF occurred in 29 patients in the MUD group, 22 patients in the MMUD group, and 24 patients in the Haplo group, whereas SGF was observed in 39, 11, and 3 patients, respectively. The cumulative incidence of PGF for the MUD, MMUD, and Haplo cohorts was 3% (95% CI, 2-4), 7% (95% CI, 4-10), and 13% (95% CI, 8-17), respectively (P < .001) (Table 2). No significant differences were observed according to stem cell source. In multivariable analysis (Table 3), compared with MUD, MMUD (odds ratio [OR], 2.93; 95% CI, 1.52-5.6; P = .001) and Haplo (OR, 5.15; 95% CI, 2.5-10.58; P < .001) were associated with a higher rate of PGF. Another factor associated with a higher rate of PGF was KPS <90% (OR, 2.41; 95% CI, 1.38-4.15; P = .002).
Multivariable analysis of transplant outcomes
| Covariate . | Group . | PGF . | aGVHD 2-4 . | cGVHD . | OS . | GRFS . | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) . | P value . | HR (95% CI) . | P value . | HR (95% CI) . | P value . | HR (95% CI) . | P value . | HR (95% CI) . | P value . | ||
| Donor type | MUD | ||||||||||
| MMUD | 2.93 (1.52-5.6) | .001 | 1.96 (1.39-2.76) | <.001 | 1.3 (0.9-1.87) | .17 | 1.53 (1.12-2.09) | .007 | 1.41 (1.07-1.86) | .01 | |
| Haplo | 5.15 (2.5-10.58) | <.001 | 1.14 (0.72-1.8) | .6 | 0.96 (0.56-1.62) | .9 | 1.94 (1.34-2.8) | <.001 | 1.78 (1.29-2.46) | <.001 | |
| Donor age (decades) | 0.94 (0.72-1.22) | .5 | 1.1 (0.94-1.29) | .2 | 1.18 (1.01-1.38) | .03 | 1.12 (0.99-1.27) | .08 | 1.1 (0.99-1.23) | .08 | |
| Patient age (decades) | 0.92 (0.77-1.07) | .3 | 0.89 (0.81-0.97) | .01 | 1.18 (1.09-1.27) | <.001 | 1.26 (1.18-1.34) | <.001 | 1.15 (1.08-1.22) | <.001 | |
| Karnofsky score | 90-100 | ||||||||||
| <90 | 2.41 (1.38-4.15) | .002 | 0.84 (0.58-1.2) | .3 | 1.22 (0.88-1.69) | .2 | 1.47 (1.13-1.9) | .004 | 1.31 (1.04-1.66) | .02 | |
| TBI given | No | ||||||||||
| Yes | 0.78 (0.42-1.43) | .4 | 1.52 (1.1-2.12) | .01 | 1.07 (0.76-1.5) | .7 | 0.92 (0.69-1.22) | .19 | 0.98 (0.77-1.26) | .9 | |
| Stem cell source | Bone marrow | ||||||||||
| Peripheral blood | 0.79 (0.44-1.39) | .4 | 1.08 (0.78-1.49) | .6 | 1.07 (0.78-1.47) | .7 | 0.93 (0.71-1.04) | .6 | 0.93 (0.74-1.17) | .5 | |
| Interval from diagnosis to HCT (y) | 1.04 (0.96-1.11) | .3 | 1.01 (0.96-1.06) | .7 | 1.02 (0.99-1.06) | .2 | 1.01 (0.97-1.04) | .8 | 1.04 (1.01-1.07) | .006 | |
| Center effect | Variance | 0.4 | .03 | 0.35 | .08 | 0.39 | .003 | 0.16 | .06 | ||
| Covariate . | Group . | PGF . | aGVHD 2-4 . | cGVHD . | OS . | GRFS . | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) . | P value . | HR (95% CI) . | P value . | HR (95% CI) . | P value . | HR (95% CI) . | P value . | HR (95% CI) . | P value . | ||
| Donor type | MUD | ||||||||||
| MMUD | 2.93 (1.52-5.6) | .001 | 1.96 (1.39-2.76) | <.001 | 1.3 (0.9-1.87) | .17 | 1.53 (1.12-2.09) | .007 | 1.41 (1.07-1.86) | .01 | |
| Haplo | 5.15 (2.5-10.58) | <.001 | 1.14 (0.72-1.8) | .6 | 0.96 (0.56-1.62) | .9 | 1.94 (1.34-2.8) | <.001 | 1.78 (1.29-2.46) | <.001 | |
| Donor age (decades) | 0.94 (0.72-1.22) | .5 | 1.1 (0.94-1.29) | .2 | 1.18 (1.01-1.38) | .03 | 1.12 (0.99-1.27) | .08 | 1.1 (0.99-1.23) | .08 | |
| Patient age (decades) | 0.92 (0.77-1.07) | .3 | 0.89 (0.81-0.97) | .01 | 1.18 (1.09-1.27) | <.001 | 1.26 (1.18-1.34) | <.001 | 1.15 (1.08-1.22) | <.001 | |
| Karnofsky score | 90-100 | ||||||||||
| <90 | 2.41 (1.38-4.15) | .002 | 0.84 (0.58-1.2) | .3 | 1.22 (0.88-1.69) | .2 | 1.47 (1.13-1.9) | .004 | 1.31 (1.04-1.66) | .02 | |
| TBI given | No | ||||||||||
| Yes | 0.78 (0.42-1.43) | .4 | 1.52 (1.1-2.12) | .01 | 1.07 (0.76-1.5) | .7 | 0.92 (0.69-1.22) | .19 | 0.98 (0.77-1.26) | .9 | |
| Stem cell source | Bone marrow | ||||||||||
| Peripheral blood | 0.79 (0.44-1.39) | .4 | 1.08 (0.78-1.49) | .6 | 1.07 (0.78-1.47) | .7 | 0.93 (0.71-1.04) | .6 | 0.93 (0.74-1.17) | .5 | |
| Interval from diagnosis to HCT (y) | 1.04 (0.96-1.11) | .3 | 1.01 (0.96-1.06) | .7 | 1.02 (0.99-1.06) | .2 | 1.01 (0.97-1.04) | .8 | 1.04 (1.01-1.07) | .006 | |
| Center effect | Variance | 0.4 | .03 | 0.35 | .08 | 0.39 | .003 | 0.16 | .06 | ||
Multivariable logistic regression model of PGF before day 42 and Cox cause–specific hazards models of aGVHD grade 2 to 4, cGVHD, OS, GVHD, and GRFS. Donor and patient age at transplant are in decades. Effect estimates are given with 95% CIs. Corresponding P values are calculated using the Wald test. No center effect was identified for PGF. Center variance was 0 and is thus, not reported here. P values considered statistically significant are shown in bold.
No statistically significant difference was found in SGF, which was 4% (95% CI, 3-5), 4% (95% CI, 2-7), and 2% (95% CI, 0-4) in MUD, MMUD, and Haplo, respectively (P = .4) (Table 2). A second transplantation after graft failure was performed in 90 patients in the MUD group, 36 patients in the MMUD group, and 29 patients in the Haplo group.
GVHD
The cumulative incidence of aGVHD grades 2 to 4 and 3 to 4 at 100 days was 13% (95% CI, 11-15) and 5% (95% CI, 3-6) for the MUD cohort, 22% (95% CI, 17-27) and 9% (95% CI, 5-12) for the MMUD cohort, and 19% (95% CI, 13-24) and 7% (95% CI, 3-10) for the Haplo cohort, respectively (P < .001 and P = .028) (Table 2). In multivariable analysis (Table 3), MMUD was found to be associated with increased risk of aGVHD grades II to IV compared with MUD (HR, 1.96; 95% CI, 1.39-2.76; P < .001). Additionally, the use of TBI in the conditioning regimen (HR, 1.52; 95% CI, 1.1-2.12; P = .01) was also associated with a higher risk of aGVHD grades 2 to 4. There was no correlation between the use of TBI and the choice of stem cell source in any donor cohort. Patient age was associated with the risk of aGVHD grades 2 to 4 per decade increase (HR, 0.89; 95% CI, 0.81-0.97; P = .01).
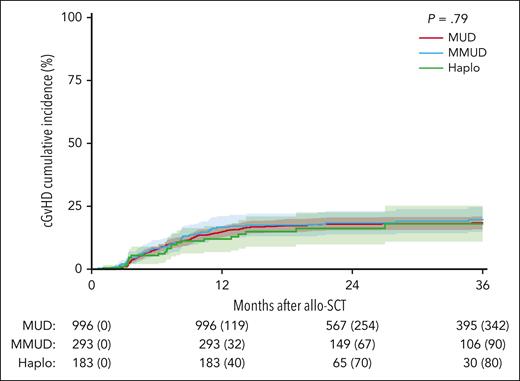
The 3-year cumulative incidence of cGVHD for the MUD, MMUD, and Haplo cohorts was 18% (95% CI, 16-21), 20% (95% CI, 15-25), and 18% (95% CI, 11-25), respectively (P = .79) (Figure 1; Table 2). The cumulative incidence of extensive cGVHD was 7% (95% CI, 6-9) for MUD, 7% (95% CI, 4-10) for MMUD, and 6% (95% CI, 1-10) for Haplo (P = .6), respectively (Table 2). In multivariable analysis (Table 3), increasing donor and patient age per decade (HR, 1.18; 95% CI, 1.01-1.38; P = .03; and HR, 1.18; 95% CI, 1.09-1.27; P < .001; respectively) were independently associated with higher risk of cGVHD.
Cumulative incidence curves of cGVHD stratified by donor type. The numbers of patients censored at indicated time points are provided within parentheses.
Cumulative incidence curves of cGVHD stratified by donor type. The numbers of patients censored at indicated time points are provided within parentheses.
Because ATG and alemtuzumab were options that were mutually exclusive for in vivo TCD in the MUD and MMUD cohorts, multivariable analyses confined to these groups revealed that alemtuzumab exhibited a lower risk of aGVHD grades 2 to 4 (HR, 0.23; 95% CI, 0.14-0.38; P < .001) and cGVHD (HR, 0.57; 95% CI, 0.39-0.83; P = .004) compared with ATG.
NRM and causes of death
The 3-year cumulative incidence of NRM was 14% (95% CI, 12-17) for MUD, 19% (95% CI, 14-23) for MMUD, and 27% (95% CI, 19-34) for Haplo (P < .001) (Figure 2; Table 2). Among the 330 patients who died, the main cause of death was infection (172; 53%), which accounted for 90 (49%) in the MUD cohort, 49 (61%) in the MMUD cohort, and 33 (55%) in the Haplo cohort. The remaining causes of death accounted for <10% of total deaths, except for GVHD (38; 11.5%). Differences among the 3 cohorts were not statistically significant.
Cumulative incidence curves of NRM stratified by donor type. The numbers of patients censored at indicated time points are provided within parentheses.
Cumulative incidence curves of NRM stratified by donor type. The numbers of patients censored at indicated time points are provided within parentheses.
Survival
The 3-year EFS for the MUD, MMUD, and Haplo cohorts was 73% (95% CI, 71-76), 63% (95% CI, 58-69), and 55% (95% CI, 47-63), respectively (P < .001) (Table 2), whereas OS was 81% (95% CI, 79-84), 74% (95% CI, 69-79), and 63% (95% CI, 54-71), respectively (P < .001) (Table 2). In multivariable analysis (Table 3), compared with MUD, MMUD (HR, 1.53; 95% CI, 1.12-2.09; P = .007) and Haplo (HR, 1.94; 95% CI, 1.34-2.8; P < .001) were associated with worse survival. Other predictors for worse OS were increasing patient age per decade (HR, 1.26; 95% CI, 1.18-1.34; P < .001) and KPS <90% (HR, 1.47; 95% CI, 1.13-1.9; P = .004).
The 3-year GRFS for the MUD, MMUD, and Haplo cohorts was 73% (95% CI, 70-76), 65% (95% CI, 60-71), and 54% (95% CI, 45-62), respectively (P < .001) (Figure 3; Table 2). These differences persisted even when analyzing patients aged <18 and ≥18 years separately. Among patients aged <18 years, the GRFS for the MUD, MMUD, and Haplo cohorts was 84% (95% CI, 80-88), 70% (95% CI, 62-78), and 58% (95% CI, 44-71), respectively (P < .001). Similarly, among patients aged ≥18 years, it was 65% (95% CI, 60-69), 62% (95% CI, 53-70), and 52% (95% CI, 41-63), respectively (P = .03), in the same order. In multivariable analysis (Table 3), compared with MUD, MMUD (HR, 1.41; 95% CI, 1.07-1.86; P = .01) and Haplo (HR, 1.78; 95% CI, 1.29-2.46; P < .001) were associated with worse GRFS. Other factors associated with worse GRFS were increasing patient age per decade (HR, 1.15; 95% CI, 1.08-1.22; P < .001), KPS <90% (HR, 1.31; 95% CI, 1.04-1.66; P = .02), and a longer interval between diagnosis and transplantation (HR, 1.04; 95% CI, 1.01-1.07; P = .006).
Kaplan–Meier curves of GRFS stratified by donor type. The numbers of patients censored at indicated time points are provided within parentheses.
Kaplan–Meier curves of GRFS stratified by donor type. The numbers of patients censored at indicated time points are provided within parentheses.
Multivariable analyses confined to the MUD and MMUD cohorts, similar to those conducted for acute and cGVHD, also revealed that alemtuzumab was associated with improved OS (HR, 0.49; 95% CI, 0.34-0.7; P < .001) and GRFS (HR, 0.58; 95% CI, 0.43-0.78; P < .001) compared with ATG.
Discussion
In a scenario where the vast majority of MUD and MMUD transplants received standard GVHD prophylaxis and all haploidentical transplants used PT-Cy, this study shows that SCT from MUD yields better survival outcomes for patients with SAA compared with both MMUD and Haplo. In addition, in multivariable analysis, MUD SCT was found to be associated with lower rates of grade 2 to 4 aGVHD compared with MMUD SCT, despite using similar GVHD prophylaxis. However, this association did not significantly differ when compared with Haplo SCT. Conversely, MMUD and Haplo SCT exhibited significantly higher rates of PGF compared with MUD.
Although our study represents, to our knowledge, the largest study comparing outcomes among transplants from alternative donors in patients with acquired SAA, it is important to acknowledge certain limitations inherent to registry-based analyses. However, registry-based studies represent real-world practices, providing insightful perspectives, especially for rare diseases such as SAA. The most apparent limitation in our study is the uneven distribution of certain clinical and transplant-related characteristics across the donor groups. The observed center effect, as seen in other registry studies,31 may be attributed to the low numbers of patients per center in certain subgroups. Notably, some variables that could potentially influence survival outcomes, such as patient age, interval from diagnosis to transplantation, and the stem cell source,6,32,33 were found to be unevenly distributed among the 3 cohorts. Specifically, the MMUD cohort consisted of younger patients, the MUD cohort had a shorter interval from diagnosis to transplantation, and the Haplo group, aside from a shorter learning curve, had a higher proportion of patients receiving peripheral blood as the source of stem cells. However, these differences did not seem clinically relevant and did not accumulate within a single cohort.
In several recent studies, including ours, a notable incidence of PGF has been observed in patients with SAA who underwent Haplo SCT22,34-37 but also in those who received MMUD SCT.8,10 This finding has been attributed to various factors, with the presence of donor-specific HLA antibodies,38 the absence of prior IST, and type of conditioning being the most prominent.22,37 The impact of donor-specific HLA antibodies may be particularly relevant in Haplo and MMUDs. Unfortunately, because of data unavailability, their potential impact on graft failure was not explicitly addressed in our study, highlighting the need for future research. Although data on pretransplantation IST were available for only a quarter of the series, the analyses of this subgroup show no significant differences in the incidence of PGF or any other transplant outcomes. Regarding the utilization of TBI, emerging evidence suggests that intensifying conditioning by increasing TBI doses may potentially mitigate the risk of graft failure, particularly in highly sensitized and treatment-naïve patients with SAA undergoing Haplo SCT, without inducing severe organ toxicity.22 Concerns about the use of TBI persist and the optimum dose may yet have to be determined. This approach has also shown promise in other IST-naïve nonmalignant diseases, such as severe hemoglobinopathies.39 Although our study did not uncover any evidence suggesting an influence of conditioning on PGF, we did observe a higher incidence of this event in the Haplo and MMUD cohorts, as previously mentioned. Additionally, our analysis revealed that poor performance status was associated with an increased risk of PGF. These findings underscore the importance of considering alternative factors to be incorporated into clinical decision-making in the context of graft failure prevention.
Considering that the incidence of GVHD is particularly relevant in patients with nonmalignant diseases such as SAA, who lack the benefit of the graft-versus-tumor effect, we should underscore the higher risk of aGVHD grade 2 to 4 observed in the MMUD cohort compared with both the MUD and the Haplo cohorts. These findings align with previous reports where HLA disparity showed an impact on the incidence of aGVHD grade 2 to 4.26,40,41 Therefore, exploring innovative strategies to reduce GVHD in nonmalignant diseases becomes imperative. Approaches such as the use of PT-Cy have demonstrated efficacy in hematological malignancies, not only in haploidentical but also in MUD and MMUD SCT.42-46 Additionally, partial ex vivo TCD47 in the context of SAA has emerged as a compelling option deserving consideration. In the absence of other established efficacy and safety measures, it is crucial to consider additional factors beyond the type of donor in decision-making. For instance, our study identified a higher risk of aGVHD grades 2 to 4 associated with the use of TBI in conditioning and patient age, whereas for cGVHD, risk factors were donor and patient age. In contrast, in vivo TCD with alemtuzumab was found to decrease the risk of both aGVHD grades 2 to 4 and cGVHD when compared with ATG, indicating a potentially stronger lymphodepletive effect, as previously reported.48 However, it is important to note that alemtuzumab was exclusively used in Great Britain, raising the possibility of a center effect, which cannot be entirely ruled out. These findings suggest that attention should be given to factors such as conditioning regimen, TCD, and donor age to optimize outcomes in SCT.
The observation of more favorable outcomes in the MUD cohort than in the MMUD and Haplo cohorts in our study, which is consistent with findings in diseases other than SAA,45,46 raises the question of whether MMUD and Haplo SCT should still be considered experimental approaches and thus reserved only for patients without a suitable MUD. However, these registry data should be interpreted with caution, since results from other series involving patients with refractory SAA who underwent Haplo transplantation14-20,49 or MMUD transplantation50 showed significantly more favorable outcomes than those reported in our study. Considering the young age of most of the patients in this study, it is reasonable to question the applicability of the results to older patients. Recognizing the significant contributions from Chinese studies, it is crucial to acknowledge potential genetic differences between Chinese and White cohorts that may impact outcomes. Furthermore, economic considerations may be influential in regions where the choice between IST and SCT must be made.51 Future research should encompass diverse populations for a comprehensive understanding of differences in transplantation outcomes in SAA.
In conclusion, our study findings support MUD transplantation as the preferable choice over MMUD or Haplo transplantation for patients with SAA lacking an MSD. However, in the absence of a matched donor, choosing between an MMUD and Haplo donor remains uncertain. These findings provide valuable insights for clinicians when making decisions regarding transplantation strategies based on donor availability. However, it is crucial to conduct prospective controlled studies to thoroughly investigate the relative efficacy and safety of SCT from alternative donors, and to optimize conditioning regimens and strategies for GVHD and graft failure prevention. Additionally, the development of effective strategies for preventing GVHD in nonmalignant diseases, such as SAA, remains an unmet need that warrants further investigation.
Acknowledgments
The authors thank all centers from the Severe Aplastic Anemia Working Party of the European Society for Blood and Marrow Transplantation that kindly agreed to participate in this study.
Authorship
Contribution: J.M., A.R., R.P.d.L. conceptualized and designed the study; J.M., D.-J.E., A.R., R.P.d.L. performed data analysis and interpretation; and all authors were involved in manuscript writing and gave final approval for the manuscript before submission.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Juan Montoro, Department of Hematology, Hospital Universitario y Politécnico La Fe, Avenida Fernando Abril Martorell 106, 46026 Valencia, Spain; email: juanmontorogomez@gmail.com.
References
Author notes
All relevant data are available in the article. The corresponding author can be contacted for additional information.
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal