In this issue of Blood, Baumrin and colleagues report on the primary qualitative development and initial validation process used for the newly proposed Lee Symptom Scale–Skin Sclerosis (LSS-Scl), a patient-reported outcome (PRO) instrument of 55 items specifically developed for adult patients with chronic graft-versus-host disease (cGVHD)-associated skin sclerosis.1
cGVHD is an immune-mediated, heterogenous, multiorgan complication affecting recipients of allogeneic hematopoietic cell transplantation (HCT). The proposed 3 biologic phases of cGVHD with sclerosis begin with early inflammation caused by tissue injury and progress to aberrant tissue repair and fibrosis driven by impaired tolerance and immune dysregulation, leading to sclerosis.2 The skin is the most commonly affected organ in cGVHD, and patients with longstanding or severe forms of the disease are the most likely to develop sclerosis.3 Sclerosis of the skin and fascia is associated with a particularly high symptom burden, impaired health-related quality of life, high morbidity, and disability. Improved treatment of this disorder remains an area of unmet need.4 The refinement of the 2014 clinician-reported organ-specific National Institutes of Health (NIH) skin score and clinical response criteria along with the development of novel tools to better measure and document changes in skin sclerosis for clinical trials were identified as top priorities and key elements of the roadmap for progress in skin cGVHD by the 2020 NIH consensus conference.4 Although efforts are underway to refine clinician-reported outcome measures for specific skin phenotypes (erythematous vs sclerotic) through the Cutaneous NIH cGVHD Response Criteria Taskforce, developing sclerosis-specific PRO measures would help in the assessment of any treatment advancement in this highly morbid disease. Such measures could capture disease burden and functional impairment while assessing treatment responses that may not be captured by clinicians, even when using previously refined and validated tools.
The Lee Symptom Scale (LSS) is a 2-minute PRO measure designed to assess the symptom burden of cGVHD. The 30-item scale content of the LSS was validated by cognitive interviews.5,6 The LSS is currently considered the gold standard PRO measure and has been incorporated as a secondary endpoint in clinical trials, as recommended by the NIH cGVHD consensus criteria. It includes a skin subscale (5 questions addressing skin symptom burden) and a muscle/joint subscale (4 questions addressing joint, muscle, and fascia symptom burden). Changes in LSS skin and muscle/joint subscales correlate with patient-reported changes in sclerotic disease burden7 as well as with the NIH skin score and organ response, making the scale useful for capturing changes in disease manifestations.8 However, previous work has also highlighted the need for refinement of the LSS skin subscale,6 particularly for sclerotic forms of skin disease, which necessitate additional components to capture symptom severity and functional implications. In addition, there is interest in refining the clinician-reported skin score, as substantial changes must occur to be considered a treatment response. This is especially pertinent in cGVHD-associated sclerosis, where treatment responses are slow and active sclerosis difficult to distinguish on clinical exam from fixed deficits.
Addressing this need, and in line with guidance from the US Food and Drug Administration (FDA), the LSS-Scl PRO was created by a team led by Stephanie Lee and including experts in qualitative methods and instrument development. The authors employed a 2-part qualitative approach to identify relevant PRO domains for cGVHD-associated sclerosis in adults and then evaluate the content validity of the candidate items. In the first phase, 36 adults with cGVHD-associated sclerosis of the skin or fascia per NIH diagnostic criteria9 were recruited from one academic medical center. Semistructured open-ended qualitative interviews were conducted to capture sclerosis-relevant symptoms and functional limitations. Following the coding of symptoms and functions, redundant terms or those with low relevance were omitted, and new symptoms and functions not previously included in existing sclerosis-specific PROs were added. This process resulted in 5 main domains of candidate items: 1) skin changes, 2) symptoms, 3) emotional and social functioning, 4) mobility restrictions, and 5) activity limitations. In the second phase of content validation, a pool of 54 items were tested and iteratively refined through cognitive debriefing interviews until a target of >80% comprehension was achieved in 25 participants. Using FDA guidance, phrasing changes were made to improve relevance and comprehension. One item was removed, and 2 items were added to address respondent feedback, resulting in 55 items, requiring a median time of 4 minutes for completion.
Prior experience and understanding of the similarities and differences in the pathophysiology and clinical course of cGVHD-associated sclerosis compared with other sclerotic skin conditions have highlighted the need to learn from, but not directly extrapolate other PRO measures to this unique patient population.10 Using this methodical approach and incorporating FDA guidance, Baumrin and colleagues present a promising tool that demonstrates preliminary construct validity through correlation with clinical assessments of disease severity using the modified Rodnan skin score and photographic range of motion. Although there was effort to ensure inclusion of diverse sclerotic disease manifestations, the study is limited by its lack of racial diversity and single-center recruitment. Future validation studies are needed and are currently underway. In addition, there remains a need to develop a similar tool for the pediatric population.
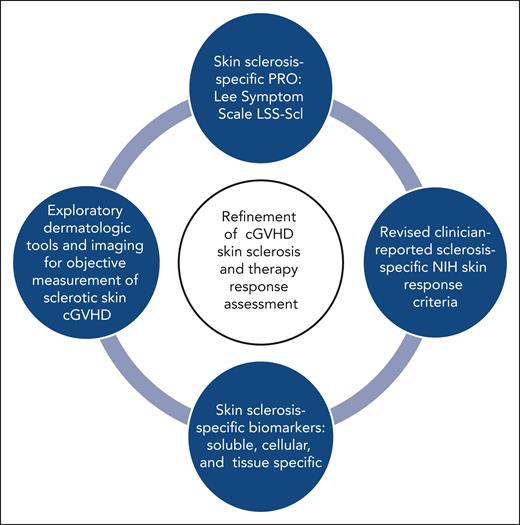
The newly proposed LSS-Scl PRO instrument is part of a long-awaited effort to accelerate progress in this highly morbid form of cGVHD (see figure). The ability to better assess skin sclerosis by incorporating these PRO endpoints should stimulate clinical trials targeting this form of cGVHD.
Key components for advancing the refinement of cGVHD skin sclerosis assessment and therapy response evaluation.
Key components for advancing the refinement of cGVHD skin sclerosis assessment and therapy response evaluation.
Conflict-of-interest statement: The authors declare no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal