Visual Abstract
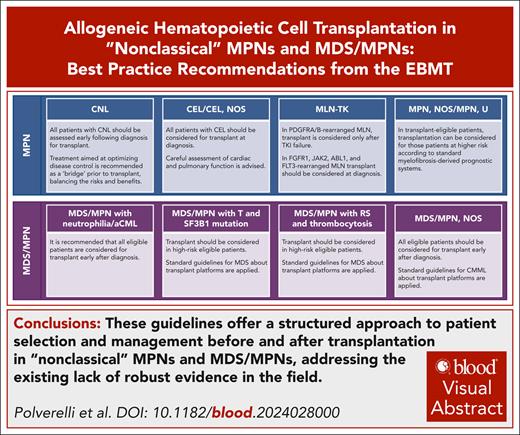
“Nonclassical” myeloproliferative neoplasms (MPNs) and myelodysplastic/myeloproliferative neoplasms (MDS/MPNs) represent a heterogeneous group of malignancies characterized by a wide range of clinical manifestations. Unlike classical MPNs, there is no standardized management approach for these conditions, particularly concerning the indications for and management of allogeneic hematopoietic cell transplantation. To address this gap, the European Society for Blood and Marrow Transplantation (EBMT) Practice Harmonization and Guidelines (PH&G) Committee and the Chronic Malignancies Working Party (CMWP) have collaborated to develop shared guidelines aimed at optimizing the selection and management of patients with these rare forms of neoplasms. A comprehensive review of the literature from the publication of the revised fourth edition of the (2016) World Health Organization classification onward was conducted. A multidisciplinary group of experts in the field convened to produce this document, which was developed through multiple rounds of draft circulation. Key recommendations include the early identification of potential transplant candidates, particularly in cases of chronic neutrophilic leukemia, chronic eosinophilic leukemia (CEL)/CEL, not otherwise specified (CEL-NOS), myeloid/lymphoid neoplasm with eosinophilia and tyrosine kinase gene fusions with FGFR1, JAK2, ABL1, and FLT3 rearrangements, MDS/MPN with neutrophilia/atypical chronic myeloid leukemia, and MDS/MPN, NOS. For patients with MPN, NOS/MPN unclassifiable, standard recommendations for myelofibrosis should be applied. Similarly, in MDS/MPN with thrombocytosis, transplantation is recommended on the basis of established MDS guidelines. Given the current lack of robust evidence, this document will serve as a valuable resource to guide future research activities, providing a framework for addressing critical unanswered questions and advancing the field.
Introduction
Myeloproliferative neoplasms (MPNs) and myelodysplastic/myeloproliferative neoplasms (MDS/MPNs) represent a heterogeneous and complex group of hematological malignancies. Recent refinements introduced by the World Health Organization (WHO) classification of tumors and International Consensus Classification (ICC) have enhanced our understanding and categorization of these conditions.1,2 These entities frequently display a broad spectrum of clinical manifestations and can present significant challenges to accurate diagnosis, prognostication, and treatment. Among “classical” MPNs, chronic myeloid leukemia (CML), essential thrombocythemia, polycythemia vera, and myelofibrosis (MF) are the most frequently recognized. Several recent publications have addressed the primary treatment goals and the role of transplant in these conditions.3-5 Similarly, chronic myelomonocytic leukemia (CMML) is the most common form of MDS/MPN, and contemporary management has been thoroughly discussed in the recent literature.6 By contrast, because of their relative rarity and hence limited cumulative evidence base, adult “nonclassical” forms of MPNs and MDS/MPNs remain an area with significant unmet need in terms of both diagnosis and clinical management. These uncommon disorders include chronic neutrophilic leukemia (CNL) (WHO/ICC), chronic eosinophilic leukemia (CEL) (WHO)/CEL, not otherwise specified (NOS) (ICC), myeloid/lymphoid neoplasms (MLNs) with eosinophilia and tyrosine kinase (TK) gene fusions (MLN-TK) (WHO/ICC), and MPN, NOS (WHO)/MPN-unclassifiable (U) (ICC) among the MPNs. In addition, MDS/MPN with neutrophilia (WHO)/atypical CML (aCML) (ICC), MDS/MPN with SF3B1 mutation and thrombocytosis (WHO)/MDS/MPN with thrombocytosis and SF3B1 mutation (ICC), MDS/MPN with ring sideroblasts and thrombocytosis, NOS (recognized only by ICC), and MDS/MPN, NOS (WHO/ICC) are included under the spectrum of MDS/MPN diseases.1,2
The prognosis for patients with such nonclassical MPNs and MDS/MPNs varies widely based on the specific subtype, molecular landscape, and individual patient factors. Although some patients experience a relatively indolent disease course, others may display an aggressive disease course with significant rates of morbidity and a markedly reduced life expectancy. Thus, allogeneic hematopoietic stem cell transplantation (HCT) remains a viable option for eligible patients, despite inherent risks in terms of both morbidities and nonrelapse mortality (NRM). The rarity, heterogeneity, and complexity characteristics to the management of these disorders underscore the need for standardized best practice recommendations, particularly in the context of HCT. These recommendations are key to address critical issues, such as ideal patient selection, pretransplant treatment strategies, optimal timing for HCT, and comprehensive transplant policies. Given these challenges, the European Society for Blood and Marrow Transplantation (EBMT) Practice Harmonization and Guidelines Committee has prioritized the development of best practice recommendations for the management of adult patients with nonclassical MPNs and MDS/MPNs undergoing HCT. These recommendations aim to provide a cohesive framework to improve patient outcomes and harmonize clinical practices across treatment centers internationally.
Methodology
This workshop was conducted according to the method published by the EBMT Practice Harmonization and Guidelines Committee.7 The Chronic Malignancies Working Party of the EBMT proposed the development of practice recommendations for nonclassical MPNs and MDS/MPNs. To comprehensively assess the scope of the issue, the EBMT registry was analyzed, collecting data on transplant procedures for each indication starting from 2016, following the release of the fourth edition of the WHO classification (Table 1). Despite the limited number of cases, transplant procedures have shown a consistent upward trend in recent years, suggesting a growing awareness of such diseases.
Number of transplant procedures for nonclassical MPNs and MDS/MPNs performed in Europe from 2016 to 2023
| Diagnosis . | Year of HCT . | 2016 Frequency . | 2017 Frequency . | 2018 Frequency . | 2019 Frequency . | 2020 Frequency . | 2021 Frequency . | 2022 Frequency . | 2023 Frequency . |
|---|---|---|---|---|---|---|---|---|---|
| MPN | CNL (WHO/ICC) | 4 | 7 | 11 | 9 | 13 | 8 | 10 | 10 |
| CEL (WHO)/CEL, NOS (ICC) | 1 | 1 | 4 | — | 2 | 1 | 3 | 4 | |
| MLN-TK with ABL1 rearrangement | — | — | — | — | — | — | — | — | |
| MLN-TK with FGFR1 rearrangement | 2 | 3 | 5 | 1 | 3 | 2 | — | 1 | |
| MLN-TK with FLT3 rearrangement | — | — | — | — | — | — | — | — | |
| MLN-TK with JAK2 rearrangements | — | — | — | — | — | 1 | 1 | 4 | |
| MLN-TK with PDGFRA/B rearrangement | — | — | — | — | — | — | — | 1 | |
| MPN, NOS (WHO)/ MPN-U (ICC) | 37 | 35 | 37 | 46 | 42 | 46 | 42 | 80 | |
| Total nonclassical MPN | 44 | 46 | 57 | 56 | 60 | 58 | 56 | 100 | |
| MDS/MPN | MDS/MPN with neutrophilia (WHO)/aCML (ICC) | 37 | 32 | 40 | 44 | 36 | 40 | 38 | 40 |
| MDS/MPN with ring sideroblasts and thrombocytosis, NOS (ICC only) | — | — | — | — | — | 1 | 2 | 7 | |
| MDS/MPN with SF3B1 mutation and thrombocytosis (WHO)/MDS/MPN with thrombocytosis and SF3B1 mutation (ICC) | — | — | — | — | — | — | — | — | |
| MDS/MPN, NOS (WHO/ICC) | 59 | 84 | 98 | 91 | 107 | 99 | 112 | 86 | |
| Total nonclassical MDS/MPN | 96 | 116 | 138 | 135 | 143 | 140 | 152 | 133 |
| Diagnosis . | Year of HCT . | 2016 Frequency . | 2017 Frequency . | 2018 Frequency . | 2019 Frequency . | 2020 Frequency . | 2021 Frequency . | 2022 Frequency . | 2023 Frequency . |
|---|---|---|---|---|---|---|---|---|---|
| MPN | CNL (WHO/ICC) | 4 | 7 | 11 | 9 | 13 | 8 | 10 | 10 |
| CEL (WHO)/CEL, NOS (ICC) | 1 | 1 | 4 | — | 2 | 1 | 3 | 4 | |
| MLN-TK with ABL1 rearrangement | — | — | — | — | — | — | — | — | |
| MLN-TK with FGFR1 rearrangement | 2 | 3 | 5 | 1 | 3 | 2 | — | 1 | |
| MLN-TK with FLT3 rearrangement | — | — | — | — | — | — | — | — | |
| MLN-TK with JAK2 rearrangements | — | — | — | — | — | 1 | 1 | 4 | |
| MLN-TK with PDGFRA/B rearrangement | — | — | — | — | — | — | — | 1 | |
| MPN, NOS (WHO)/ MPN-U (ICC) | 37 | 35 | 37 | 46 | 42 | 46 | 42 | 80 | |
| Total nonclassical MPN | 44 | 46 | 57 | 56 | 60 | 58 | 56 | 100 | |
| MDS/MPN | MDS/MPN with neutrophilia (WHO)/aCML (ICC) | 37 | 32 | 40 | 44 | 36 | 40 | 38 | 40 |
| MDS/MPN with ring sideroblasts and thrombocytosis, NOS (ICC only) | — | — | — | — | — | 1 | 2 | 7 | |
| MDS/MPN with SF3B1 mutation and thrombocytosis (WHO)/MDS/MPN with thrombocytosis and SF3B1 mutation (ICC) | — | — | — | — | — | — | — | — | |
| MDS/MPN, NOS (WHO/ICC) | 59 | 84 | 98 | 91 | 107 | 99 | 112 | 86 | |
| Total nonclassical MDS/MPN | 96 | 116 | 138 | 135 | 143 | 140 | 152 | 133 |
A list of global experts and key opinion leaders in the field, including hematologists, hematopathologists, molecular biology specialists, and transplant physicians, was compiled on the basis of their professional experience, prior research, and relevant scientific contributions. Key clinical questions and areas of unmet clinical needs were identified to guide consensus development, organized into 3 distinct sections (supplemental Material, available on the Blood website).
During the initial meeting in June 2024, experts formed specific subgroups to focus on individual topics. A comprehensive literature search of PubMed/MedLine until September 2024 was conducted for each key question, identifying indexed articles. In accordance with the EBMT practice recommendation method, and because of the lack of prospective studies, the evidence was derived from retrospective studies, reviews, and expert opinions, without formal evidence grading.
A task force was established to draft panel positions addressing the identified key questions. These drafts underwent multiple iterations within respective subgroups. A hybrid face-to-face and virtual meeting with EBMT members was held on 30 September 2024 and 1 October 2024, in Lille, France, to finalize the recommendations.
The primary goal of the meeting was to develop a comprehensive draft consensus manuscript, which was subsequently reviewed by all authors to finalize these agreed-upon best practice recommendations with a focus on the identification and pretransplant and posttransplant management of patients with nonclassical MPN and MDS/MPN, where relevant literature was available. All recommendations were considered valid if an agreement of >80% was reached. Table 2 presents a list of the key publications in the field of transplantation for these entities.
Main publications reporting on transplant cohorts of patients with nonclassical MPN and MDS/MPN
| Author (year) . | MDS/MPN type . | Patient No. . | Tranplant period . | Age, median (range), y . | Donor . | Conditioning . | Stem cell source . | NRM/relapse . | Survival outcome . |
|---|---|---|---|---|---|---|---|---|---|
| Dholaria (2022)8 | CNL | 29 | 2000-2018 | 58 (33-72) | MRD 41% UD 56% MMRD 3% | MAC 48% | PB 93% | NRM 13.8% at 4y CIR 34.5% at 4y | OS 55.2% at 1 y |
| McLornan (2022)9 | CEL/CEL, NOS | 30 | 2000-2018 | 46 (IQR, 40-55) | MRD 30% UD 67% MMRD 3% | MAC 61% | PB 67% | NRM 45% at 3y CIR 20% at 3y | OS 34% at 3 y |
| McLornan (2020)10 | MPN, NOS/MPN-U | 70 | 2000-2015 | NA (22-70) | MRD 39% UD 61% | MAC 44% | PB 91% | NRM 34% at 5y (MAC) CIR 27% at 5y (MAC) | OS 41% at 5 y (MAC) |
| Metzgeroth (2023)11 | MLN-TK | 25 | 2003-2022 | NA | NA | NA | NA | NR | 10/12 alive at 3 y (chronic phase) 7/13 alive at 4.7 y (blast phase) |
| Hernández-Boluda (2022)12 | MLN-TK with FGFR1 rearrangement | 22 | 1997-2018 | 51 (22-67) | MRD 23% UD 68% MMRD9% | MAC 55% | PB 86% | NRM 14% at 5y CIR 23% at 5y | OS 74% at 5 y |
| Tang (2021)13 | MLN-TK with FLT3 rearrangement | 6 | 2005-2020 | 34 (2-43) | NA | NA | NA | NA | 4/6 alive in CR at a median follow-up of 41 mo |
| Onida (2017)14 | MDS/MPN with neutrophilia/aCML | 42 | 1997-2006 | 46 (25-67) | MRD 64% UD 36% | MAC 76% | PB 67% | NRM 24% at 5y CIR 40% at 5y | OS 51% at 5 y |
| Itonaga (2018)15 | MDS/MPN with neutrophilia/aCML | 14 | 2003-2014 | 45 (10-66) | MRD 36% UD 64% | MAC 86% | PB 14% BM 72% CB 14% | NRM 2 relapse/progression 4 | 8/14 alive at last follow-up |
| Kurosawa (2020)16 | MDS/MPN, NOS | 86 | 2001-2017 | 57 (16-71) | MRD 28% UD 72% | MAC 62% | BM/PB 80% CB 20% | NRM 26% at 3y CIR 24% at 3y | OS 49% at 3 y |
| Author (year) . | MDS/MPN type . | Patient No. . | Tranplant period . | Age, median (range), y . | Donor . | Conditioning . | Stem cell source . | NRM/relapse . | Survival outcome . |
|---|---|---|---|---|---|---|---|---|---|
| Dholaria (2022)8 | CNL | 29 | 2000-2018 | 58 (33-72) | MRD 41% UD 56% MMRD 3% | MAC 48% | PB 93% | NRM 13.8% at 4y CIR 34.5% at 4y | OS 55.2% at 1 y |
| McLornan (2022)9 | CEL/CEL, NOS | 30 | 2000-2018 | 46 (IQR, 40-55) | MRD 30% UD 67% MMRD 3% | MAC 61% | PB 67% | NRM 45% at 3y CIR 20% at 3y | OS 34% at 3 y |
| McLornan (2020)10 | MPN, NOS/MPN-U | 70 | 2000-2015 | NA (22-70) | MRD 39% UD 61% | MAC 44% | PB 91% | NRM 34% at 5y (MAC) CIR 27% at 5y (MAC) | OS 41% at 5 y (MAC) |
| Metzgeroth (2023)11 | MLN-TK | 25 | 2003-2022 | NA | NA | NA | NA | NR | 10/12 alive at 3 y (chronic phase) 7/13 alive at 4.7 y (blast phase) |
| Hernández-Boluda (2022)12 | MLN-TK with FGFR1 rearrangement | 22 | 1997-2018 | 51 (22-67) | MRD 23% UD 68% MMRD9% | MAC 55% | PB 86% | NRM 14% at 5y CIR 23% at 5y | OS 74% at 5 y |
| Tang (2021)13 | MLN-TK with FLT3 rearrangement | 6 | 2005-2020 | 34 (2-43) | NA | NA | NA | NA | 4/6 alive in CR at a median follow-up of 41 mo |
| Onida (2017)14 | MDS/MPN with neutrophilia/aCML | 42 | 1997-2006 | 46 (25-67) | MRD 64% UD 36% | MAC 76% | PB 67% | NRM 24% at 5y CIR 40% at 5y | OS 51% at 5 y |
| Itonaga (2018)15 | MDS/MPN with neutrophilia/aCML | 14 | 2003-2014 | 45 (10-66) | MRD 36% UD 64% | MAC 86% | PB 14% BM 72% CB 14% | NRM 2 relapse/progression 4 | 8/14 alive at last follow-up |
| Kurosawa (2020)16 | MDS/MPN, NOS | 86 | 2001-2017 | 57 (16-71) | MRD 28% UD 72% | MAC 62% | BM/PB 80% CB 20% | NRM 26% at 3y CIR 24% at 3y | OS 49% at 3 y |
CB, cord blood; CIR, cumulative incidence of relapse; IQR, interquartile range; MAC, myeloablative conditioning; MMRD, mismatched related donor; MRD, measurable residual disease; NA, not available; PB, peripheral blood; UD, unrelated donor.
Current state-of-the-art approaches
Molecular landscape of nonclassical MPNs and MDS/MPNs
The application of next-generation sequencing (NGS) technology to large cohorts of patients with nonclassical MPNs and MDS/MPNs has unveiled molecular features characterizing, but not defining, the individual nosological disease types, now recognized in the most recent diagnostic classifications (see below Comparison of WHO/ICC classifications).1,2 Particularly, studies focusing on the molecular architecture of these disorders identified specific comutational patterns underpinning the multistep pathogenesis linked to the clinical heterogeneity of these nonclassical MPNs and MDS/MPNs.
Nonclassical MPNs are frequently diagnosed on the basis of prominent clinical features (eg, eosinophilia, splenomegaly, and leukocytosis), and absence of criteria fulfilling the diagnosis of classical MPNs. Some, but not all, are characterized by specific molecular patterns:
CNL is strongly, but not exclusively, associated with pathogenetic CSF3R mutations.
CEL is a diagnosis of exclusion with no indicative molecular features.
MLN-TK have disease-defining gene alterations: PDGFRA, PDGFRB, FGFR1, JAK2, FLT3, and ETV6::ABL1 and other tyrosine-kinase alterations.
Cases with MPN, NOS/U typically have JAK2, CALR, or MPL mutations but do not meet the hematological and histopathologic criteria for classical MPN.
Within the MDS/MPN entities, conventional cytogenetics can identify clonality/aberrations in 15% to 35% of cases, most typically in MDS/MPN with neutrophilia/aCML,17 whereas NGS panels show recurrent myeloid gene mutations in ≈90% of cases.18 Mutations in epigenetic regulators (ASXL1, TET2, and DNMT3A), splicing (SF3B1, SRSF2, and U2AF1), the JAK-STAT pathway (JAK2, CALR, and MPL), and the rat sarcoma virus (RAS) pathway (NRAS, KRAS, and CBL) genes are the most recurrent alterations.17 In general, the combination and order of acquisition of such lesions dictate the clinicopathologic presentation. The current classification is not strictly segregated according to molecular lesions, such that mutations may occur promiscuously across these entities. However, several studies have highlighted that patients with MDS/MPN could be broadly characterized by their genomic make-up:17,19,20
MDS/MPN with neutrophilia/aCML frequently carry SETBP1 and/or ASXL1 mutations.
“MDS/MPN with ring sideroblasts and thrombocytosis" cases are dominated by SF3B1 and often JAK2 mutations or, at a low frequency, CALR or MPL mutations.
Especially in MDS/MPN, NOS, molecular mutations can be useful for further disease stratification. Genotypically patients with “CMML-like” MDS/MPN, NOS show enrichment for TET2, as well as SRSF2, ASXL1, RUNX1, and RAS pathway alterations.
Phenotypically, patients with “MDS/MPN with neutrophilia-like” MDS/MPN, NOS show enrichment for ASXL1, SETBP1, ETNK1, RUNX1, TET2, and RAS pathway gene mutations.
The current WHO/ICC classifications incorporate only SF3B1 as a disease-defining lesion in the MDS/MPN and thrombocytosis category.
Apart from these recurrent genomic profiles, some less frequent mutations may identify cases with specific clinical trajectories and outcomes (eg, TP53, CBL).21 Genomic information may help to establish an accurate diagnosis, enhance prognostication, and even support reclassification of ambiguous cases into currently defined disease entities, supplementing pathomorphologic and clinical criteria.22
Comparison of WHO/ICC classifications
The fifth edition of the WHO classification2 and the ICC of myeloid and lymphoid neoplasms1 are built on the revised fourth edition of the (2016) WHO classification.23 For entities included in this article, the definitions and diagnostic criteria in the WHO fifth edition and ICC are similar, with some key differences as summarized in Table 3.
Differences and similarities among the WHO (fifth edition) and ICC classifications
| WHO revised fourth edition . | WHO fifth edition . | ICC . | Differences or similarities . |
|---|---|---|---|
| CNL | CNL Unchanged from 2016 | CNL Similar to WHO revised fourth edition except: Lowering of threshold PB WBC >13 × 109/L if accompanied by CSF3R mutation Defines Accelerated phase as circulating or BM blasts 10%-19% with progressive splenomegaly or worsening thrombocytopenia Blast phase as circulating or BM blasts ≥20% | In the presence of CSF3R mutation–lowering of the PB WBC threshold to >13 × 109/L for diagnosis in ICC Definition of accelerated and blast phase added in ICC |
| CEL, NOS | CEL | CEL, NOS | Both exclude the growing number of tyrosine kinase gene fusions now categorized separately. WHO fifth edition drops the not otherwise specified (NOS) descriptor |
| Myeloid/lymphoid neoplasms with eosinophilia and gene rearrangement | Myeloid/lymphoid neoplasms with eosinophilia and tyrosine kinase gene fusions | Myeloid/lymphoid neoplasms with eosinophilia and tyrosine kinase gene fusions | Both add expanded categories involving JAK2 and FLT3 rearrangements and add ETV6::ABL1 fusion |
| MPN, U | MPN, NOS | MPN-U | Remains unchanged, with only minor terminology adjustments in the WHO fifth edition |
| Atypical CML, BCR-ABL1 negative | MDS/MPN with neutrophilia Same as revised fourth edition but name changed | Atypical CML Essentially unchanged from revised fourth edition except to delete reference to the lack of BCR::ABL1 gene fusion in the name | Significant terminology changes in WHO fifth edition |
| MDS/MPN with ring sideroblasts and thrombocytosis | MDS/MPN with SF3B1 mutation and thrombocytosis | MDS/MPN with thrombocytosis and SF3B1 mutation MDS/MPN with ring sideroblasts and thrombocytosis, NOS | The ICC distinguishes forms carrying the SF3B1 mutation from those without |
| MDS/MPN, U | MDS/MPN, NOS | MDS/MPN, NOS | Remains unchanged, with only minor terminology adjustments in the WHO fifth edition |
| WHO revised fourth edition . | WHO fifth edition . | ICC . | Differences or similarities . |
|---|---|---|---|
| CNL | CNL Unchanged from 2016 | CNL Similar to WHO revised fourth edition except: Lowering of threshold PB WBC >13 × 109/L if accompanied by CSF3R mutation Defines Accelerated phase as circulating or BM blasts 10%-19% with progressive splenomegaly or worsening thrombocytopenia Blast phase as circulating or BM blasts ≥20% | In the presence of CSF3R mutation–lowering of the PB WBC threshold to >13 × 109/L for diagnosis in ICC Definition of accelerated and blast phase added in ICC |
| CEL, NOS | CEL | CEL, NOS | Both exclude the growing number of tyrosine kinase gene fusions now categorized separately. WHO fifth edition drops the not otherwise specified (NOS) descriptor |
| Myeloid/lymphoid neoplasms with eosinophilia and gene rearrangement | Myeloid/lymphoid neoplasms with eosinophilia and tyrosine kinase gene fusions | Myeloid/lymphoid neoplasms with eosinophilia and tyrosine kinase gene fusions | Both add expanded categories involving JAK2 and FLT3 rearrangements and add ETV6::ABL1 fusion |
| MPN, U | MPN, NOS | MPN-U | Remains unchanged, with only minor terminology adjustments in the WHO fifth edition |
| Atypical CML, BCR-ABL1 negative | MDS/MPN with neutrophilia Same as revised fourth edition but name changed | Atypical CML Essentially unchanged from revised fourth edition except to delete reference to the lack of BCR::ABL1 gene fusion in the name | Significant terminology changes in WHO fifth edition |
| MDS/MPN with ring sideroblasts and thrombocytosis | MDS/MPN with SF3B1 mutation and thrombocytosis | MDS/MPN with thrombocytosis and SF3B1 mutation MDS/MPN with ring sideroblasts and thrombocytosis, NOS | The ICC distinguishes forms carrying the SF3B1 mutation from those without |
| MDS/MPN, U | MDS/MPN, NOS | MDS/MPN, NOS | Remains unchanged, with only minor terminology adjustments in the WHO fifth edition |
BM, bone marrow; PB, peripheral blood; WBC, white blood cell.
Regarding MPN classification, the definition of CNL remained unchanged in the WHO fifth edition, whereas the ICC reduced the threshold of required neutrophilia (>13 × 109/L) in the presence of a CSF3R mutation. The ICC defines both accelerated and blast phases. These definitions may enable therapeutic interventions and interpretations of outcomes in future trials. CEL continues to be recognized in the WHO fifth edition and ICC as an MPN characterized by persistent eosinophilia, clonality, and abnormal/dysplastic bone marrow morphology that does not fulfil the diagnostic criteria of MLN with eosinophilia and TK fusions (MLN-TK) or other defined myeloid neoplasms that may present with eosinophilia. Although both classifications regard CEL as a diagnosis of exclusion in patients with sustained eosinophilia, they differ in minor aspects.
In the category of MDS/MPNs, the WHO fifth edition renamed aCML as MDS/MPN with neutrophilia but kept diagnostic parameters the same. The ICC maintained the name of aCML, adding mutational status (SETBP1 and/or ASXL1) as supportive of the diagnosis. Both classifications split MDS/MPN with ring sideroblasts and thrombocytosis into SF3B1 mutated and unmutated. The ICC explicitly defined MDS/MPN with SF3B1 and thrombocytosis to exclude therapy-related and other cytogenetic and genetic anomalies. The WHO fifth edition additionally recognizes that any MDS/MPN entity may arise after exposure to cytotoxic therapy. Both the WHO fifth edition and the ICC have renamed MDS/MPN, U, as MDS/MPN, NOS.
Disease-specific HCT indications
CNL (WHO/ICC)
CNL is a rare disorder presenting with leukocytosis and frequently splenomegaly. It has a variable clinical course but is ultimately associated with a poor prognosis, with a median survival of <2 years. Disease progression remains the primary cause of death.24,25 Conventional treatment strategies are highly variable, ranging from cytoreduction with hydroxycarbamide and interferon to use of targeted kinase inhibitors, such as ruxolitinib or dasatinib, albeit responses are commonly short lived.26 “Acute myeloid leukemia (AML)–style” induction approaches may be considered in accelerated/blast-phase disease as a potential bridge to HCT in eligible patients, but the regimen of choice remains undetermined.27
Features of progression include debilitating splenomegaly, treatment refractoriness and progressive neutrophilia, acquisition of transfusion dependency, and increasing genomic complexity.24,28 The presence/acquisition of pathogenetic mutations in ASXL1, CBL, CEBPA, EZH2, NRAS, TET2, and/or U2AF1 are associated with poor overall prognosis.24,28
Given the poor prognosis associated with conventional therapy, all patients with CNL should be assessed early after diagnosis for potential transplant eligibility. However, data addressing the HCT outcomes in this disease group are limited. The largest cohort published to date was a retrospective evaluation of 29 patients who underwent transplantation between 2000 and 2018 performed on behalf of the Center for International Blood and Marrow Transplant Research and the EBMT.8 Blast phase patients were excluded. Stem cell source was predominantly peripheral blood, with myeloablative conditioning (MAC) accounting for ≈50%, whereas nonmyeloablative/reduced intensity conditioning (RIC) was used in the other 50%. Overall survival after transplantation exceeded 50% at 4 years, with limited NRM but relapse rate of 35% at 4 years (Table 2), underscoring the importance of rigorous posttransplant monitoring to detect early signs of disease recurrence. No specific studies are available on the use of pretransplant treatments as a bridge to HCT. However, given the limited disease modulation, pretransplant cytoreductive or tyrosine kinase inhibitor (TKI) therapy should be considered to enhance disease control (reduce white blood cell count; improve splenomegaly) and optimize the patient's physical condition in preparation for HCT, balancing the risks and benefits while considering the potential use of such treatments (eg, infectious risk, disease progression).24 Development of dynamic posttransplant measurable residual disease (MRD) analyses when a molecular marker is detected (eg, CSF3R) needs to be further investigated in this setting but is encouraged by the panel to collate such data where possible.29 The use of maintenance therapy after transplant with agents such as ruxolitinib or dasatinib remains investigational. Panel recommendations for CNL are summarized in Table 4.
Panel recommendations for CNL
| Disease . | Panel recommendations . |
|---|---|
| CNL (WHO/ICC) | All patients with CNL should be assessed early following diagnosis for potential transplant eligibility and donor search Treatment aimed at optimizing disease control (control of leukocytosis, reduction in splenomegaly, where relevant) is recommended as a “bridge” before transplant, balancing the risks and benefits Given limited data, no recommendations can be made on optimal transplant conditioning regimens and posttransplant disease monitoring and maintenance. However, consideration needs to be given to considerable relapse rates and approaches tailored accordingly. |
| Disease . | Panel recommendations . |
|---|---|
| CNL (WHO/ICC) | All patients with CNL should be assessed early following diagnosis for potential transplant eligibility and donor search Treatment aimed at optimizing disease control (control of leukocytosis, reduction in splenomegaly, where relevant) is recommended as a “bridge” before transplant, balancing the risks and benefits Given limited data, no recommendations can be made on optimal transplant conditioning regimens and posttransplant disease monitoring and maintenance. However, consideration needs to be given to considerable relapse rates and approaches tailored accordingly. |
CEL (WHO)/CEL, NOS (ICC)
CEL (WHO)/CEL, NOS (ICC) is a rare, debilitating, and aggressive MPN with an augmented risk of organ failure (especially cardiac failure) because of eosinophilic infiltration and high rates of transformation to acute leukemia. Median survival is poor, often estimated at <2 years from time of diagnosis.30,31
Therapeutic options range from supportive care approaches, including corticosteroids or hydroxycarbamide/interferon, to “AML-like” induction therapy and HCT; most cases frequently display limited response to therapy.30,31
Data on the outcomes of HCT in CEL are limited to a single report by the EBMT on 30 patients who underwent transplant between 2000 and 2018.9 Median age was 46 years (interquartile range, 39-59 years), with a male predominance. Stem cell source was peripheral blood derived in 67%, MAC used in 61%, unrelated donor (URD) used in 67%, and in vivo T-cell depletion in 52% of cases. The 1- and 3-year overall survival (OS) estimates were 46% and 34%, respectively; however, for patients with matched sibling donor, OS was 65% at 3 years. Transplant failure was attributable to high rates of NRM (38% at 1 year), particularly following use of a URD. This analysis was conducted before the widespread use of posttransplant cyclophosphamide, which suggests that outcomes for unrelated donor transplants may have improved in recent years.
Panel recommendations for CEL (WHO)/CEL, NOS (ICC) are summarized in Table 5.
Panel recommendations for CEL (WHO)/CEL, NOS (ICC)
| Disease . | Panel recommendations . |
|---|---|
| CEL (WHO)/CEL, NOS (ICC) | Given the poor prognosis of CEL/CEL, NOS and the risk of organ dysfunction, all patients should be considered for HCT at diagnosis with a prompt donor search Careful assessment of cardiac and pulmonary function is advised for transplant eligibility and then for tailoring transplant platform Given the lack of disease-modifying agents, no recommendation can be made on pretreatment strategies Transplant should not be delayed once a suitable donor is found |
| Disease . | Panel recommendations . |
|---|---|
| CEL (WHO)/CEL, NOS (ICC) | Given the poor prognosis of CEL/CEL, NOS and the risk of organ dysfunction, all patients should be considered for HCT at diagnosis with a prompt donor search Careful assessment of cardiac and pulmonary function is advised for transplant eligibility and then for tailoring transplant platform Given the lack of disease-modifying agents, no recommendation can be made on pretreatment strategies Transplant should not be delayed once a suitable donor is found |
Myeloid/lymphoid neoplasm with eosinophilia and tyrosine kinase gene fusions (WHO/ICC)
According to both the ICC and WHO 2022 classifications, several MLNs associated with rearrangements of PDGFRA, PDGFRB, FGFR1, JAK2, ABL1, or FLT3 tyrosine kinase genes (MLN-TK) fall within this categorization. These are rare malignancies with a frequently aggressive clinical course that can present as an MPN with a high tendency to blast phase transformation, or directly as AML, T or B lymphoblastic leukemia/lymphoma or mixed phenotype acute leukemia, with or without a concomitant MPN component. Cardiac eosinophilic infiltration is particularly prominent in patients with MLN-TK-PDGFRA.32,33 Recently, comprehensive response criteria have been proposed to address the heterogeneous clinical presentation of MLN-TK.34
Treatment with TKI, primarily imatinib, is effective in most patients with MLN harboring PDGFRA35 or PDGFRB36 fusion genes, even in the blast phase.37 This treatment can induce durable complete molecular remissions akin to those achieved in CML.38 In the German registry, only 16 of 104 (15%) patients with PDGFRA/B fusion genes had died after a median follow-up of 9.2 years.11 Acquired resistance to imatinib due to mutations has been reported in a few patients with primarily blast phase disease,39,40 although some of them may respond to alternative TKI (eg, ponatinib for T674I mutations or avapritinib for D842V mutations).41,42
In contrast, patients with FGFR1, JAK2, ABL1, or FLT3 fusion genes have less favorable responses to TKIs, often ultimately progressing to blast phase, with a median survival of ≈5 years in the German registry.11,43 However, exceptions may include patients with chronic phase MLN-FGFR1 or MLN-ETV6::ABL1, who can achieve molecular responses to pemigatinib44 or nilotinib/dasatinib,43 respectively.
Nevertheless, the durability of these responses remains uncertain, and HCT constitutes the only treatment with demonstrated long-term disease control in these conditions. A recent retrospective study by the EBMT, including 22 patients with MLN-FGFR1 undergoing HCT, reported rates of 5-year OS, progression-free survival, NRM, and relapse incidence of 74%, 63%, 14%, and 23%, respectively, underscoring the curative potential of HCT in this aggressive disease.12 Among 12 patients with MLN-FLT3 from several US institutions, 6 underwent HCT, with 4 still alive at the last follow-up.13
On the basis of these data, early referral to HCT is recommended for most eligible patients with FGFR1, JAK2, ABL1, or FLT3 fusion genes in chronic phase, because TKI treatment typically does not yield durable remissions, and the disease can rapidly progress to blast phase.33,44 Patients with MLN-FGFR1 or MLN-ETV6::ABL1 who achieve deep responses to TKIs (pemigatinib for FGFR1 or nilotinib/dasatinib for ABL1) might delay transplant if predicted to be at high risk for NRM, with close monitoring of their TKI response and reconsideration if warning signals arise. In general, bridging therapy with a specific TKI with or without chemotherapy should be considered. Patients ineligible for HCT should be considered for clinical trials. Finally, the role of TKI maintenance after HCT deserves investigation in a standardized manner. Table 6 summarizes the panel recommendations for MLN-TK.
Panel recommendations for MLN-TK (WHO/ICC)
| Disease . | Panel recommendations . |
|---|---|
| MLN-TK (WHO/ICC) | In patients with PDGFRA/B-rearranged MLN, both in chronic and blast phases, HCT is only considered after failure of TKI treatment. However, in young patients (<60 y) presenting with blast-phase disease, HCT could be considered on achieving a response. Careful assessment of cardiac and pulmonary function is advised for transplant eligibility and then for tailoring transplant platform HCT, after bridging with an alternative TKI with or without chemotherapy, seems to be the preferred option for the rare cases of MLN-PDGFRA/B with secondary resistance to imatinib HCT with donor search should be considered early after diagnosis for most eligible patients with FGFR1-, JAK2-, ABL1-, and FLT3-rearranged MLN, given the low predictability and uncertain durability of responses to TKIs TKI treatment directed to the specific molecular abnormality is recommended to decrease disease burden pre-HCT A thorough evaluation of cardiac and pulmonary function is essential, given the possible organ impairment associated with prior/ongoing eosinophilic infiltration The HCT strategy should be tailored to the predominant clinical features of the disease (ie, AML, ALL, or MPN) Monitoring of the underlying molecular abnormality using sensitive techniques is advised to inform treatment strategies to prevent overt disease relapse The role of TKI maintenance after HCT warrants investigation |
| Disease . | Panel recommendations . |
|---|---|
| MLN-TK (WHO/ICC) | In patients with PDGFRA/B-rearranged MLN, both in chronic and blast phases, HCT is only considered after failure of TKI treatment. However, in young patients (<60 y) presenting with blast-phase disease, HCT could be considered on achieving a response. Careful assessment of cardiac and pulmonary function is advised for transplant eligibility and then for tailoring transplant platform HCT, after bridging with an alternative TKI with or without chemotherapy, seems to be the preferred option for the rare cases of MLN-PDGFRA/B with secondary resistance to imatinib HCT with donor search should be considered early after diagnosis for most eligible patients with FGFR1-, JAK2-, ABL1-, and FLT3-rearranged MLN, given the low predictability and uncertain durability of responses to TKIs TKI treatment directed to the specific molecular abnormality is recommended to decrease disease burden pre-HCT A thorough evaluation of cardiac and pulmonary function is essential, given the possible organ impairment associated with prior/ongoing eosinophilic infiltration The HCT strategy should be tailored to the predominant clinical features of the disease (ie, AML, ALL, or MPN) Monitoring of the underlying molecular abnormality using sensitive techniques is advised to inform treatment strategies to prevent overt disease relapse The role of TKI maintenance after HCT warrants investigation |
MPN, NOS (WHO)/MPN-U (ICC)
MPN, NOS/MPN-U encompasses a heterogeneous group of MPNs that fail to meet stringent diagnostic criteria of other MPN entities within the WHO or ICC classification systems.1,2 True incidence remains unknown, but it is estimated to represent 5% of all MPNs if strict diagnostic criteria are applied.45 Dynamic reassessment is warranted, as over time the characteristics may meet the diagnostic criteria of other MPN entities. Clinical phenotype is markedly heterogeneous—ranging from those with an indolent disease course to those with aggressive disease associated with significant splenomegaly and symptom burden and inherent risk of leukemic transformation.46,47 A large series from a United Kingdom tertiary center, with median follow-up of >7 years, suggested thrombotic complications in ≈20% of patients and transformation rates of ≈9%, highlighting the need for close vigilance.46 Median event-free survival was 11 years. Recently, a retrospective study by Crane et al, comprising 94 patients, reported a median OS of 54 months.48 Interestingly, the Dynamic International Prognostic Scoring System-plus model and high-risk molecular profile retained prognostic relevance, suggesting that MF-derived prognostic scores may be used to inform prognosis also in this context.
McLornan et al reported an EBMT registry-based evaluation of outcomes following HCT in 70 patients with a verified diagnosis of MPN, NOS/MPN-U, representing the largest transplant cohort reported to date.10 Regarding conditioning intensity, 31 patients underwent MAC and 39 patients underwent RIC. There was a nonsignificant trend toward delayed engraftment with RIC protocols. The 1- and 5-year OS estimates were 77% and 42% (MAC) and 59% and 41% (RIC), respectively. NRM rates at 1 and 3 years were considerable at 19% and 29% for MAC and 28% and 28% for RIC, respectively. Cumulative incidences of relapse at 1 and 3 years were 10% and 23% (MAC) and 28% and 36% (RIC), respectively. Risk of relapse tended to be higher in those patients with MPN-NOS who had an abnormal karyotype at time of HCT. Regarding donor type, univariate analysis suggested worse OS and NRM rates with use of a URD compared with matched sibling donor.
Given the rarity of the disease group, any recommendations for HCT are solely translated from experience with other MPNs, predominantly MF. Pragmatically, as it has been previously suggested, consideration to HCT in transplant-eligible individuals with MPN, NOS/MPN-U who have a suitable donor may include those ascertained as having higher risk disease (ie, those with increasing peripheral blood/marrow blasts), acquisition of cytogenetic or mutational profiles predicted to be associated with a worse prognosis (transcribed from MF data as no sufficient evidence in MPN, NOS/MPN-U), progressive debilitating splenomegaly despite optimized medical therapy, or those who become transfusion dependent.3,4,46,47,49,50 From a practical stance, in our opinion, approaches taken to optimize outcomes in HCT for MF could be applied to those with MPN, NOS/MPN-U given a lack of contemporary data to guide best practice.3 The recommendations for MPN, NOS/MPN-U are included in Table 7.
Panel recommendations for MPN, NOS (WHO)/MPN, U (ICC)
| Disease . | Panel recommendations . |
|---|---|
| MPN, NOS (WHO)/MPN-U (ICC) | Given disease heterogeneity, therapeutic approaches to MPN, NOS should be discussed in centers with expertise in MPN management In patients with transplant-eligible MPN, NOS, HCT can be considered for those patients at higher risk according to standard MF-derived prognostic systems It is recommended that standard guidelines for MF pertaining to transplant are applied |
| Disease . | Panel recommendations . |
|---|---|
| MPN, NOS (WHO)/MPN-U (ICC) | Given disease heterogeneity, therapeutic approaches to MPN, NOS should be discussed in centers with expertise in MPN management In patients with transplant-eligible MPN, NOS, HCT can be considered for those patients at higher risk according to standard MF-derived prognostic systems It is recommended that standard guidelines for MF pertaining to transplant are applied |
MDS/MPN with neutrophilia (WHO)/atypical CML (ICC)
Life expectancy of patients with MDS/MPN with neutrophilia/aCML is, in general, short, with a sizable proportion (up to 40%) transforming into AML within 12 to 18 months from diagnosis and a median OS reported in the 12- to 24-month range.51,52 Despite the advent of novel targeted therapies and drug combinations currently under active investigation, HCT remains the only curative option. Factors reported as associated with inferior survival by retrospective analyses of a limited-size patient series include age >65 years, presence of cytopenias (anemia and thrombocytopenia), leukocytosis, elevated lactate dehydrogenase level, higher marrow blast percentage, and/or presence of pathogenetic TET2 mutations, with several models proposed to stratify patients at diagnosis according to the risk of disease-associated death.52-55 However, median survival remained extremely poor, even in the lower-risk groups (<2 years’ median OS).
An EBMT registry-based retrospective study of 42 patients reported that half of patients were alive after 6 years after transplant.14 A smaller Japanese experience with shorter follow-up demonstrated comparable results.15 The MD Anderson group reported on 65 patients, 7 of whom underwent transplant. Median survival for the nontransplant cohort was 24.6 months and not reached in the transplant cohort.52 There are no robust data on whether pretransplant treatment influences outcomes after transplantation. Leukocytosis is typically managed with cytoreductive agents, like hydroxyurea or immunomodulation with interferon. Hypomethylating agents (HMAs) and/or chemotherapy-based induction regimens are usually favored when there is a high blast count in advanced stages of the disease, particularly in the context of AML transformation. Table 8 lists the panel's recommendations for this entity.
Panel recommendations for MDS/MPN with neutrophilia (WHO)/atypical CML (ICC)
| Disease . | Panel recommendations . |
|---|---|
| MDS/MPN with neutrophilia (WHO)/aCML (ICC) | It is recommended that eligible patients are considered for transplant early after diagnosis with a prompt donor search No recommendations can be made on optimal transplant conditioning and posttransplant disease monitoring and maintenance |
| Disease . | Panel recommendations . |
|---|---|
| MDS/MPN with neutrophilia (WHO)/aCML (ICC) | It is recommended that eligible patients are considered for transplant early after diagnosis with a prompt donor search No recommendations can be made on optimal transplant conditioning and posttransplant disease monitoring and maintenance |
MDS/MPN with SF3B1 mutation and thrombocytosis (WHO)/MDS/MPN with thrombocytosis and SF3B1 mutation (ICC)
This entity, affecting often elderly individuals, generally presents a good prognosis, with a low risk of leukemic transformation and a median survival exceeding 5 years.56 The presence of abnormal karyotype, ASXL1/SETBP1 mutations, and/or moderate to severe anemia (hemoglobin <10 g/dL) at diagnosis or at follow-up were reported to be associated with worse prognosis, with expected median OS shorter than 1 year.57 No well molecularly annotated cohorts of transplanted MDS/MPN with SF3B1 mutation have been reported to date, with only a few case series or reports available.58-61
MDS/MPN with ring sideroblasts and thrombocytosis, NOS (ICC only)
The absence of the canonical SF3B1 mutation characterizes 10% to 30% of MDS/MPN with ring sideroblasts and thrombocytosis cases.62 However, discordant prognostic significance has been documented according to SF3B1-mutational status, with some recent reports showing no impact on OS and progression-free survival.57 In analogy to patients with SF3B1 mutation, no specific data are available in the literature regarding the role of transplantation. As shown in Table 1, only 10 patients with MDS/MPN with thrombocytosis with or without SF3B1 mutation have been reported in the EBMT registry as having undergone a transplant for this indication. Standard recommendations for HCT in MDS should hence be applied.63
Table 9 summarizes the recommendations for both MDS/MPN with SF3B1 mutation and thrombocytosis (WHO)/MDS/MPN with thrombocytosis and SF3B1 mutation (ICC) and MDS/MPN with ring sideroblasts and thrombocytosis, NOS (ICC only).
Panel recommendations for MDS/MPN with SF3B1 mutation and thrombocytosis (WHO)/MDS/MPN with thrombocytosis and SF3B1 mutation (ICC) and MDS/MPN with ring sideroblasts and thrombocytosis, NOS (ICC only)
| Disease . | Panel recommendations . |
|---|---|
| MDS/MPN with SF3B1 mutation and thrombocytosis (WHO)/MDS/MPN with thrombocytosis and SF3B1 mutation (ICC) and MDS/MPN with ring sideroblasts and thrombocytosis, NOS (ICC only) | Transplant should be considered in high-risk eligible patients (eg, refractory anemia, adverse cytogenetics, and/or presence of ASXL1 or SETBP1 mutations) in both MDS/MPN with thrombocytosis with or without SF3B1 mutation, with a prompt donor search It is recommended that standard guidelines for MDS pertaining to transplant platform are applied |
| Disease . | Panel recommendations . |
|---|---|
| MDS/MPN with SF3B1 mutation and thrombocytosis (WHO)/MDS/MPN with thrombocytosis and SF3B1 mutation (ICC) and MDS/MPN with ring sideroblasts and thrombocytosis, NOS (ICC only) | Transplant should be considered in high-risk eligible patients (eg, refractory anemia, adverse cytogenetics, and/or presence of ASXL1 or SETBP1 mutations) in both MDS/MPN with thrombocytosis with or without SF3B1 mutation, with a prompt donor search It is recommended that standard guidelines for MDS pertaining to transplant platform are applied |
MDS/MPN, NOS (WHO/ICC)
MDS/MPN, NOS remains an exceedingly rare disease entity with no established consensus on optimal therapy and a dismal prognosis. A 2-center report on 135 patients highlighted a median leukemia-free survival of 24 months.21 Evaluation of a cohort of 85 patients from the MD Anderson center, followed up from 1987 to 2013, reported a worse life expectancy, approaching 1 year.64 Additionally, the presence of TP53 mutations confers higher risk of progression.65 Regarding treatment approaches, in the above-mentioned experience, 59 of 135 received HMAs but overall had poor responses (only 1 patient achieving a complete remission [CR]). Eight (6%) patients underwent HCT, of whom 5 (63%) were alive and disease free at the last follow-up.21 The largest transplant series to date comes from the Japanese Society for Hematopoietic Cell Transplantation,16 which included a cohort of 86 MDS/MPN, NOS patients who underwent transplant between 2001 and 2017 using a heterogeneous range of transplant platforms. Disease status (stable/responsive vs progressive) and advanced age were significant prognostic factors for transplant outcomes, with overall long-term survival approaching 50%. Recently, the North American cooperative group reported on a cohort of 120 patients with MDS/MPN, including 48 NOS/U cases, who underwent haploidentical transplantation, primarily with RIC and nonmyeloablative conditioning regimens. Interestingly, transplant outcomes were comparable to those observed in CMML and other MDS/MPN overlap syndromes, with younger age (<65 years) and absence of splenomegaly identified as independent favorable factors for survival after transplant.66 All these data support the potential application of CMML-like transplant strategies even in the context of MDS/MPN, NOS.6 Cytoreductive agents, like hydroxyurea or immunomodulation with interferon, are typically used to manage increased leukocyte proliferation, whereas HMAs may be considered for patients with predominant cytopenias and/or increased blast count. JAK inhibitors, alone or combined with HMAs, have also been investigated.67 For younger patients progressing to AML, induction treatment is used as a bridge to HCT. Table 10 provides the panel’s recommendations for this entity.
Panel recommendations for MDS/MPN, NOS
| Disease . | Panel recommendations . |
|---|---|
| MDS/MPN, NOS | It is recommended that eligible patients are considered for transplant early after diagnosis, with a prompt donor search It is recommended that standard guidelines for CMML pertaining to transplant platform are applied |
| Disease . | Panel recommendations . |
|---|---|
| MDS/MPN, NOS | It is recommended that eligible patients are considered for transplant early after diagnosis, with a prompt donor search It is recommended that standard guidelines for CMML pertaining to transplant platform are applied |
Chimerism and MRD assessment
The panel agreed that chimerism and MRD monitoring should be performed in the post-HCT period, where relevant. This will facilitate data collection in an area where there is a major lack of robust evidence. A range of techniques to assess lineage-specific chimerism are available, most commonly assessed via the polymerase chain reaction (PCR) analysis of short tandem repeats to define host and donor populations.68 The role of CD34+ specific chimerism requires evaluation. MRD assessment for these disease entities remains experimental, but if assessed, sensitive laboratory techniques are preferred, ideally with a sensitivity of 0.01% to 1%, and consideration to use of digital PCR or quantitative PCR. These recommendations are as per recently suggested by the EBMT group for MRD assessment in MF as no specific guidelines exist for the specific diseases covered in these guidelines.69 The panel agreed that use of extended NGS panels for MRD assessment remains a research tool at present. Timing of assessment is as per individual institutional policies.
Unanswered questions and future research areas
Several critical questions remain unanswered in the field of nonclassical MPN and MDS/MPN. First, a better understanding of disease prognostication is essential, and ongoing efforts, such as the International Working Group registry, are expected to provide valuable insights. Additionally, pretransplant treatment strategies across the range of disorders need to be optimized to improve outcomes, as current protocols vary significantly between institutions. A relevant issue will be the determination of transplant eligibility, which remains poorly defined. Given the older age of many patients, frailty screening to assess physical function and capacity is an area of paramount importance. This screening could also incorporate tools to more specifically evaluate cognitive function, comorbidities, social status, anxiety, and nutrition, ensuring a thorough assessment of the patient’s overall health and eligibility for transplantation.70 In this regard, a strict age limit should not be imposed. Instead, it seems reasonable to extend transplant evaluation up to 70 years and, in selected fit patients, even up to 75 years.
Furthermore, donor matching is a crucial factor in weighing the risks and benefits of transplantation, although this aspect has not been extensively addressed in this particular setting. All these considerations are fundamental when discussing transplant indications and must be carefully balanced against the intrinsic risk of the disease, which remains largely undefined in many scenarios. Given the available evidence, it is not possible to recommend a one-size-fits-all timing for every case and transplant center. However, it seems reasonable to initiate the search for a donor (preferably a related donor, or an unrelated/alternative donor when necessary) early in all patients affected by diseases with an expected survival of <5 years, taking into account comorbidities, transplant risks, and patient preferences.
Another important aspect is identifying the optimal transplantation platform, including the choice of donor, the intensity of the conditioning regimen, and the approach to graft-versus-host disease prophylaxis, to achieve superior long-term outcomes across various patient populations. Disease monitoring, especially in cases where molecular markers are available, requires standardization to ensure consistent and reliable assessments across different centers. Furthermore, the role of donor lymphocyte infusion and maintenance therapy, particularly when TKIs are available, remains an area of active investigation. Finally, there is an urgent need for international prospective trials with harmonized protocols to establish universally accepted treatment guidelines and improve patient outcomes across diverse health care settings. In this context, this document will be useful in guiding future research activities, providing a framework for addressing these critical unanswered questions, and driving advancements in the field.
Acknowledgment
The authors sincerely thank Linda Koster, study coordinator of the European Society for Blood and Marrow Transplantation (EBMT), for her contribution in providing transplant procedure data from the EBMT registry.
Authorship
Contribution: N. Polverelli and D.P.M. proposed the topic for practice recommendations and led the literature review; C.G., K.R., J.C.H.-B., F.O., N. Polverelli, and D.P.M. identified key clinical questions and areas of unmet clinical needs to guide consensus development; C.G. and K.R. organized the task force for the “Current State of the Art” section; J.C.H.-B. and D.P.M. focused on nonclassical MPNs; N. Polverelli and F.O. addressed nonclassical MDS/MPNs; D.A.A., N.C.P.C., P.G., C.H., J.D.K., J.J.K., L.M., R.M., E.P., F. Palandri, M.M.P., A.O., D.H.R., A.R., and D.H.W. drafted “Current State of the Art”; G.B., F.C., T.C., V.F., N. Gagelmann, N. Gangat, J.G., T.J., F. Passamonti, N. Pemmaraju, and I.Y.-A. contributed to “Nonclassical MPN”; L.A., F.B.D., Y.C., J.D.-S., G.H., N.K., M.M., M.R., D.R., C.S., K.S., A.T., and A.M.V. worked on “Nonclassical MDS/MPN”; the preliminary draft was thoroughly reviewed by N. Polverelli, K.R., M.K., M.R., J.D.-S., T.C., J.C.H.-B., F.O., I.S.-O., I.Y.-A., and D.P.M., who prepared the final draft; and all authors reviewed the manuscript and approved its final version.
Conflict-of-interest disclosure: J.G. was included in the response adjudication committee for FIGHT-203 trial (Pemigatinib in FGFR1-Rearranged MLN). N. Gangat received fees for advisory board for DISC Medicine and Agios. Y.C. has received institutional consulting fees for advisory board from Merck Sharp & Dohme (MSD), Novartis, Incyte, Bristol Myers Squibb (BMS), Pfizer, AbbVie, Roche, Jazz, Gilead, Amgen, AstraZeneca, Servier, Takeda, Pierre Fabre, and Medac and has received travel support from MSD, Roche, Novartis, Pfizer, BMS, Gilead, Amgen, Incyte, AbbVie, Janssen, AstraZeneca, Jazz, Pierre Fabre, and Sanofi, all via the institution. T.J. received institutional research support from CTI Biopharma, Kartos Therapeutics, Incyte, BMS, Tscan, Karyopharm Therapeutics; serves on the advisory board of BMS, Incyte, AbbVie, CTI, Kite, Cogent Biosciences, Blueprint Medicine, Telios Pharma, Protagonist Therapeutics, Galapagos, Tscan Therapeutics, Karyopharm, Morphosys, and In8Bio. The remaining authors declare no competing financial interests.
Correspondence: Nicola Polverelli, Unit of Bone Marrow Transplantation and Cellular Therapies, Division of Hematology, Fondazione IRCCS Policlinico San Matteo, Viale Camillo Golgi 19, 27100 Pavia, Italy; email: n.polverelli@smatteo.pv.it.
References
Author notes
The online version of this article contains a data supplement.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal