Abstract
We previously used peripheral newborn blood (NBB) as a possible in vivo experimental model for cord blood (CB) transplantation and showed that B10.D2 NBB cells successfully reconstituted adult (DBA/2 × B10.D2)F1 mice without causing graft-versus-host disease (GVHD), probably because of their phenotypic and functional immaturity. Here we investigated the influence of T-cell maturation occurring in NBB cells during the early postbirth period on the degree of engraftment, the incidence of GVHD, and the graft-versus-leukemia (GVL) potential. These parameters were compared in recipients grafted with bone marrow (BM) cells. We observed an increased percentage of CD4+ mature T cells accompanied by the acquisition of proliferative responses to phytohemagglutinin (PHA) and to allogeneic cells of day-5 NBB cells. The capacity of day-2 NBB to engraft was moderately reduced and recipients developing GVHD were occasionally observed after the graft of day-5 NBB cells. No GVL effect was evidenced regardless of the time of postbirth blood collection. However, the GVL effect can be obtained by the delayed infusion of donor mature T cells to recipients grafted with day-0 NBB, without causing GVHD. In contrast, the same protocol applied to mice grafted with BM cells induced GVHD mortality of all recipients. Interleukin (IL)-10 but not IL-2 messenger RNA was expressed in NBB cells as opposed to BM cells. These findings suggest that, in terms of GVHD incidence, delayed infusion of mature T cells as post-transplant tumor immunotherapy would be more effective when applied after CB than after BM transplantation.
IN RECENT YEARS, THE number of transplantations using human umbilical cord blood (CB) instead of bone marrow (BM) has increased regularly, yielding promising results.1,2 Indeed, CB may represent a particularly desirable source of transplantable cells because previous studies indicate that it contains a large number of hematopoietic progenitors.3 In addition, it has been reported that these cells possess a naive phenotype,4 a reduced alloreactivity,5-8 and a limited capacity to cause graft-versus-host disease (GVHD).1,2,9 Because many CB transplantations concern children with malignant diseases,1,2,9 it is important to preserve an intact antileukemic effect. Yet the low potential of CB cells to induce a GVHD might be associated with a lack of graft-versus-leukemia (GVL) effect because effector T cells responsible for GVHD contribute, at least partially, to the GVL effect.10 On the other hand, natural killer (NK) and lymphokine-activated killer (LAK) cells were shown to mediate this effect.5,11,12 If NK lytic cell activity is minimal in CB, increased LAK activity can be enhanced in vitro by incubation with interleukin-2 (IL-2).5,11 12 All these data are encouraging but are not conclusively indicative of the real in vivo capacity of CB cells to mediate a GVL effect in the absence of GVHD.
In a previous study, we explored an experimental murine model for CB transplantation and showed the powerful capacity of peripheral blood (PB) cells from B10.D2 newborn mice (NBB cells) to engraft fully in adult (DBA/2 × B10.D2)F1 mice without inducing a GVHD across the minor histocompatibility antigens (mHAgs) barrier.13
The purpose of this report was to examine whether, in our experimental murine model, we could show that a GVL effect exists in the absence of a GVHD across the mHAgs barrier. Yet our previous data clearly showed that murine NBB cells displayed more immature phenotypic and functional characteristics than human CB cells.13 Therefore in attempts to mimic the human situation, we investigated the immunological reactivity and the GVHD and GVL capacity of NBB cells collected from B10.D2 mice either on the day of birth or 2 and 5 days later. It is known that phenotypic maturation and acquisition of immunocompetence progressively develop during the early postbirth period at rates that depend on the cell compartment and the function studied.14-17 However, most of the studies were done in thymus or peripheral lymphoid organs and no data are available for PB.
Here we report a significant increase in the percentage of CD4+ mature T cells in day-5 NBB accompanied by the acquisition of proliferative responses to phytohemagglutinin (PHA) and to allogeneic cells. Yet the capacity of NBB cells to engraft irradiated F1 recipients was significantly reduced when NBB was collected 2 days after birth and mice developing GVHD were only occasionally observed after the graft of day-5 NBB cells. However, no GVL effect was observed regardless of the time of postbirth blood collection. Additional experiments indicated that a GVL effect can be obtained, without causing GVHD, by the delayed infusion of donor mature T cells to recipients grafted with NBB collected on the day of birth. In contrast, the same protocol applied to mice grafted with BM cells induced GVHD mortality of all recipients. We hypothesize that the protection against GVHD by NBB cells involves the intervention of regulatory mechanisms.
MATERIALS AND METHODS
Mice.
B10.D2 (H-2d, Mls-1b2b), DBA/2 (H-2d, Mls-1a2a), (DBA/2 × B10.D2)F1 (H-2d/d, Mls-1a/b2a/b), C57BL/6 (H-2b, Mls-1b2b) mice were bred in our own animal facility.
PB collection.
The PB from individual adult or newborn B10.D2 mice was collected on Calciparin.13 The volume of blood obtained from one newborn mouse ranged from 40 to 50 μL. For in vitro experiments, PB from six to eight individual newborn mice from the same litter was pooled and mononuclear cells were prepared using Ficoll/Hypaque gradients (1090; Pharmacia, Uppsala, Sweden). PB from one adult B10.D2 mouse (500 to 800 μL) was similarly separated on Ficoll/Hypaque gradient (1077; Pharmacia). For in vivo experiments, the blood of two newborn mice was pooled before injection into recipients.
Graft procedure.
(DBA/2 × B10.D2)F1 mice were exposed to a 137Cs radiation source (RX 30/55 irradiator; Gravatom Industries Ltd, Gosport, UK) at a dose rate of 0.75 Gy/minute. Lethally irradiated (9.5 Gy) recipients were infused intravenously with 107 BM cells and 8 × 106 lymph node B10.D2 cells, or with 6 × 105 adult PB B10.D2 cells, or with 106 PB cells (two B10.D2 newborn mice) collected on the day of birth or 2 and 5 days later.
Phenotype characterization.
Mononuclear cells from B10.D2 adult or newborn PB and from adult BM were directly labeled with fluorescein isothiocyanate (FITC)- or phycoerythrin (PE)-conjugated anti-CD4, anti-CD8, anti-TCR α/β monoclonal antibodies (MoAb) (Pharmingen Clinisciences, Montrouge, France) and anti–Thy-1 MoAb (Coulter, Margency, France). Unconjugated rat MoAb against stem-cell antigen (SCA-1, clone Fall-3; Pharmingen) and mouse MoAb against Lyt-1.1 allele (Coulter) were shown by FITC-conjugated goat antirat immunoglobulin (Ig) (GAR, Coulter) or by FITC-conjugated goat antimouse Ig (GAM, Coulter), respectively.13 Briefly, 5 × 105 cells were incubated for 30 minutes at 4°C with the corresponding MoAb. After washing, the cells were stained with the specific second reagent. PE-conjugated anti-CD4 and FITC-conjugated anti-CD8 MoAbs were mixed before incubation. Samples of 10,000 cells were analyzed in a flow cytometer (Profile II, Coulter) and the percentage of single- or double-positive cells was calculated.
Mixed lymphocyte reaction (MLR) and mitogen stimulation.
Cells (2 × 105 per well) from B10.D2 adult or newborn PB and from B10.D2 adult BM and spleen were cultured with PHA or concanavalin A (Con A) mitogens and with irradiated splenocytes (4 × 105 per well) from C57BL/6 mice. Proliferation was evaluated 2 days (cultures with mitogens) or 3 days (cultures with irradiated spleen cells) later by 3H-thymidine incorporation, added during the last 18 hours of culture.
Evaluation of GVL effect.
To assess the GVL effect, two protocols were used (1) F1 recipients were injected intravenously with 105 P815 tumor cells (mastocytoma from DBA/2 mice) 1 day before lethal irradiation and grafting with B10.D2 BM cells or NBB cells collected on different days after birth and (2) 103 P815 cells were injected intravenously into F1 mice 2 to 3 months after the graft of BM or NBB cells collected on different days after birth.
RNA extraction and cDNA synthesis.
2 × 106 Cells from adult spleen, BM, and NBB were stimulated by Con A and pelleted after 24 hours of culture. Total RNA was extracted with RNABle (Eurobio, les Ulis, France) and ethanol precipitated with the addition of 5 μg of glycogen before resuspension in 20 μL of water. Single-strand complementary DNA (cDNA) was synthesized using the First-Strand synthesis kit (Pharmacia Biotech, Orsay, France) and then diluted in 30 μL of water.
Oligonucleotides.
Cα, IL-2, interferon-γ (IFNγ), IL-4, and IL-10 primers were obtained from Life Technologies (GIBCO BRL, France).
Reverse Transcriptase Polymerase Chain Reaction (RT-PCR).
One μL of cDNA was added to 50 μL of amplification mixture (2.5 mmol/L MgCl2, 10 mmol/L dNTPs, 12.5 pmol/L of IL 3′ and 5′ primers with 1.5 u/reaction Taq polymerase) and overlaid with mineral oil (Sigma Chemical Co, St Louis, MO). The mixtures were submitted to 45 cycles, each consisting of 45 seconds at 94°C, 1 minute at 60°C, and 1 minute at 72°C. Ten μL aliquots of the reaction mixture were withdrawn through oil at 35, 40, and 45 cycles and analyzed by ethidium bromide staining of 2% agarose gel. For quantitative PCR, 5 μL of the reaction mixture was sampled through oil at different cycle numbers and transferred into avidin-coated wells containing 95 μL of TRIS-EDTA buffer for quantitation of the amplified products in a liquid-hybridization–enzyme-linked immunosorbent assay (ELISA) with luminometry readings.18
Statistical Analysis.
Statistical analysis for in vitro experiments was performed using Student’s t test. Survival data were analyzed using the χ2 test that compared the percentage of surviving mice presented in Figs 1, 3, and 4. The Mann-Whitney nonparametric test was used to compare the rate of mortality (Fig 2).
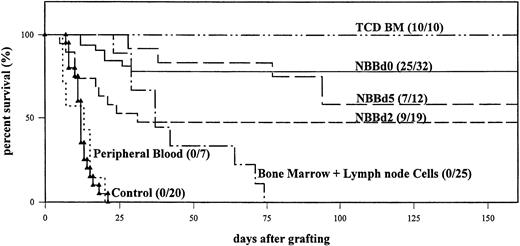
In vivo survival of lethally irradiated (DBA/2 × B10.D2)F1 mice either receiving no cells (control, ▴) or grafted with B10.D2 cells from adult PB (···), TCD BM (–··–), BM, and lymph nodes (–·–) or NBB collected on days 0 (––), 2 (– –), and 5 (— —) after birth. Mortality was recorded daily and mice were examined for the presence of clinical GVHD (number of live mice/total number of mice).
In vivo survival of lethally irradiated (DBA/2 × B10.D2)F1 mice either receiving no cells (control, ▴) or grafted with B10.D2 cells from adult PB (···), TCD BM (–··–), BM, and lymph nodes (–·–) or NBB collected on days 0 (––), 2 (– –), and 5 (— —) after birth. Mortality was recorded daily and mice were examined for the presence of clinical GVHD (number of live mice/total number of mice).
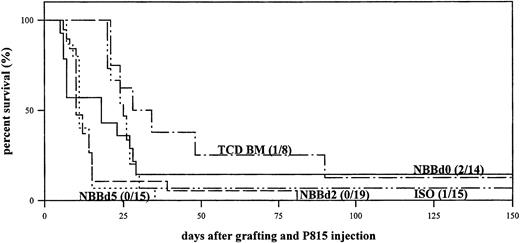
In vivo survival of lethally irradiated (DBA/2 × B10.D2) F1 mice grafted with B10.D2 cells from adult TCD BM (–·–) or from NBB collected on days 0 (––), 2(– –), and 5 (···) after birth. F1 mice grafted with BM and spleen cells from F1 mice (ISO, –··–) served as controls. All recipient mice received 105 P815 cells one day before irradiation and grafting. Mortality was recorded daily and mice were examined for the presence of tumor metastasis (number of live mice/total number of mice).
In vivo survival of lethally irradiated (DBA/2 × B10.D2) F1 mice grafted with B10.D2 cells from adult TCD BM (–·–) or from NBB collected on days 0 (––), 2(– –), and 5 (···) after birth. F1 mice grafted with BM and spleen cells from F1 mice (ISO, –··–) served as controls. All recipient mice received 105 P815 cells one day before irradiation and grafting. Mortality was recorded daily and mice were examined for the presence of tumor metastasis (number of live mice/total number of mice).
RESULTS
Phenotypic maturation of NBB cells after birth.
PB was collected from B10.D2 mice either on the day of birth, 2 or 5 days later, or from adult (2- to 3-month-old) mice. After purification on a Ficoll/Hypaque gradient, mononuclear cells were stained with various labeled MoAbs. The changes in composition of NBB during the early postnatal period are illustrated in Table 1 and compared with that of adult PB and BM. As already reported in our preceding paper,13 the majority of T cells of newborn mice expressed a CD4+CD8+ Thy-1+ immature phenotype with few CD4+ or CD8+ cells with a high level of TCR α/β. The cell composition of NBB collected on the day of birth did not differ significantly from that of adult BM except for the presence of CD4+CD8+ cells. Between day 0 and day 5, the percentage of CD4+CD8+ and of Thy-1+T cells decreased significantly (P = .05 andP = .01, respectively) and that of CD4+ but not of CD8+ T cells gradually rose above that of adult BM cells (P = .003). The percentage of T cells expressing TCR αβhigh increased in parallel (P = .01). Surprisingly, the mean percentage of SCA-1+ progenitor cells did not decrease significantly after birth until day 5, although it varied greatly between different blood samples.
Phenotypic Cell Composition of Adult BM and of Adult and NBB
| Cells From . | Age . | Mean Percentage of Positive Cells ± SE . | |||||
|---|---|---|---|---|---|---|---|
| CD4+CD8− . | CD4−CD8+ . | CD4+CD8+ . | TCRα/βhigh . | Thy-1+ . | SCA-1+ . | ||
| Adult blood | 2-3 months | 16.2 ± 1.1 | 7.1 ± 1.0 | ND | 20.4 ± 1.8 | 17.7 ± 2.7 | 0.4 ± 0.1 |
| Newborn blood | Day 0 | 3.3 ± 0.7 | 2.3 ± 0.4 | 40.8 ± 8.4 | 3.0 ± 0.4 | 46.3 ± 8.3 | 17.0 ± 5.2 |
| Day 2 | 9.9 ± 2.3* | 5.0 ± 2.2 | 36.2 ± 6.9 | 6.9 ± 0.9* | 54.3 ± 6.0 | 9.0 ± 6.0 | |
| Day 5 | 13.2 ± 1.9* | 5.8 ± 1.7 | 20.1 ± 5.6* | 12.8 ± 2.7* | 36.0 ± 8.2† | 16.3 ± 3.9 | |
| Adult bone marrow | 2-3 months | 3.1 ± 0.3 | 2.0 ± 0.2 | 0.2 ± 0.1 | 7.8 ± 1.0 | 2.2 ± 0.1 | 12.5 ± 1.0 |
| Cells From . | Age . | Mean Percentage of Positive Cells ± SE . | |||||
|---|---|---|---|---|---|---|---|
| CD4+CD8− . | CD4−CD8+ . | CD4+CD8+ . | TCRα/βhigh . | Thy-1+ . | SCA-1+ . | ||
| Adult blood | 2-3 months | 16.2 ± 1.1 | 7.1 ± 1.0 | ND | 20.4 ± 1.8 | 17.7 ± 2.7 | 0.4 ± 0.1 |
| Newborn blood | Day 0 | 3.3 ± 0.7 | 2.3 ± 0.4 | 40.8 ± 8.4 | 3.0 ± 0.4 | 46.3 ± 8.3 | 17.0 ± 5.2 |
| Day 2 | 9.9 ± 2.3* | 5.0 ± 2.2 | 36.2 ± 6.9 | 6.9 ± 0.9* | 54.3 ± 6.0 | 9.0 ± 6.0 | |
| Day 5 | 13.2 ± 1.9* | 5.8 ± 1.7 | 20.1 ± 5.6* | 12.8 ± 2.7* | 36.0 ± 8.2† | 16.3 ± 3.9 | |
| Adult bone marrow | 2-3 months | 3.1 ± 0.3 | 2.0 ± 0.2 | 0.2 ± 0.1 | 7.8 ± 1.0 | 2.2 ± 0.1 | 12.5 ± 1.0 |
Adult bone marrow cells and peripheral blood cells from adult or newborn B10.D2 mice were stained with anti-CD4 and anti-CD8, anti-TCRα/β, anti–SCA-1 or anti–Thy-1 MoAb. Fluorescence of 10,000 cells was measured. Five individual mice were analyzed and mean percentage of positive cells ± SE was calculated.
Abbreviation: ND, not detected.
Significantly different when compared to newborn blood day 0 (Student’s t test P < .05).
Acquisition of immunological competence.
Previous data showed that exposure to T-cell mitogens or allogeneic cells induces only a minor proliferative response of NBB cells collected on the day of birth.13 The results presented in Table 2 show a significant increase in the response to PHA (P = .027) but not to Con A (P = .08) of NBB cells collected on day 5 in comparison with cells collected from NBB on day 0. The low reactivity to allogeneic cells observed in day-0 NBB cells increased (P = .04) in day-5 NBB cells. The proliferative responses of peripheral blood cells remain significantly weaker in newborn mice than in adult mice. These data clearly show that NBB T cells progressively acquire immunological reactivity but that they are not yet fully competent by day 5 after birth.
Proliferative Response of Cells From Newborn Blood or Adult Spleen, Peripheral Blood and BM to T-cell Mitogens and Allogeneic Cells
| Stimulation with . | Thymidine Incorporation Into Cells From Mean cpm ± SD (Stimulation Index) . | |||||
|---|---|---|---|---|---|---|
| Adult Spleen . | Adult Peripheral Blood . | Adult Bone Marrow . | Newborn Blood* . | |||
| Day 0 . | Day 2 . | Day 5 . | ||||
| — | 3355 ± 1318 | 1698 ± 846 | 5075 ± 3615 | 1494 ± 1154 | 5011 ± 1833 | 1622 ± 609 |
| PHA | 53973 ± 33611 (16.0) | 33233 ± 14898 (19.5) | 8423 ± 1412 (1.6) | 5984 ± 2036 (4.0) | 15879 ± 10363 (3.7) | 16609 ± 6893† (9.9) |
| Con A | 35663 ± 19945 (10.6) | 37873 ± 28716 (22.3) | 10730 ± 2831 (2.1) | 2533 ± 1466 (1.7) | 10227 ± 5636 (2.0) | 9352 ± 4806 (5.6) |
| Irradiated B10.D2 cells | 5887 ± 1882 | 4042 ± 2002 | 3911 ± 3103 | 2055 ± 1208 | 4483 ± 1214 | 2655 ± 569 |
| Irradiated C57Bl/6 cells | 25431 ± 5362 (4.3) | 14619 ± 17272 (3.6) | 8659 ± 2537 (2.2) | 4687 ± 2789 (1.6) | 9225 ± 3250 (2.0) | 10646 ± 2446† (4.0) |
| Stimulation with . | Thymidine Incorporation Into Cells From Mean cpm ± SD (Stimulation Index) . | |||||
|---|---|---|---|---|---|---|
| Adult Spleen . | Adult Peripheral Blood . | Adult Bone Marrow . | Newborn Blood* . | |||
| Day 0 . | Day 2 . | Day 5 . | ||||
| — | 3355 ± 1318 | 1698 ± 846 | 5075 ± 3615 | 1494 ± 1154 | 5011 ± 1833 | 1622 ± 609 |
| PHA | 53973 ± 33611 (16.0) | 33233 ± 14898 (19.5) | 8423 ± 1412 (1.6) | 5984 ± 2036 (4.0) | 15879 ± 10363 (3.7) | 16609 ± 6893† (9.9) |
| Con A | 35663 ± 19945 (10.6) | 37873 ± 28716 (22.3) | 10730 ± 2831 (2.1) | 2533 ± 1466 (1.7) | 10227 ± 5636 (2.0) | 9352 ± 4806 (5.6) |
| Irradiated B10.D2 cells | 5887 ± 1882 | 4042 ± 2002 | 3911 ± 3103 | 2055 ± 1208 | 4483 ± 1214 | 2655 ± 569 |
| Irradiated C57Bl/6 cells | 25431 ± 5362 (4.3) | 14619 ± 17272 (3.6) | 8659 ± 2537 (2.2) | 4687 ± 2789 (1.6) | 9225 ± 3250 (2.0) | 10646 ± 2446† (4.0) |
Values represent the mean ± SD of two to four tests for each experimental group. In each of the six individual experiments performed, the proliferative response of adult peripheral blood and/or adult BM and/or NBB were compared with the response of adult spleen.
Newborn blood was collected either on the day of birth (day 0) or 2 or 5 days later.
Significantly increased compared with newborn blood collected at day 0 (Student’s t test P < .05).
Engraftment GVHD incidence in F1 mice receiving NBB cells collected on different days after birth.
In our transplantation model, all F1 recipients grafted with BM mixed with lymph node cells died because of acute GVHD against incompatible host DBA/2 mHAgs (Fig 1). Conversely, F1 mice receiving only BM cells depleted of mature Thy-1+ T cells (TCD BM) survived and became fully chimeric. F1 recipients grafted with adult PB died, because of the absence of engraftment due to the lack of SCA-1+ progenitor cells (Table 1), with a rate of mortality similar to that of irradiated F1 mice receiving no cells (control). PB was collected from newborn mice either on the day of birth or 2 and 5 days later. The blood of two newborn mice, containing around 106 mononuclear cells, was pooled before injection into lethally irradiated (DBA/2 × B10.D2)F1 mice. The percentage survival was significantly reduced (χ2 test; P = .052) when recipients were grafted with day-2 NBB cells (47%) compared with day-0 NBB cells (78%). In these two groups, early mortalities (before day 10) were due to a lack of engraftment attested by the microscopic size of the spleen. Mice grafted with day-5 NBB cells reacted differently; 5 of the 12 mice (42%) died after day 30 with signs of GVHD. None of the mice surviving over 100 days developed signs of GVHD.
Immunohematopoietic reconstitution of NBB-engrafted F1 recipients.
We evaluated the degree of chimerism of recipients grafted 2- to 3-months earlier by measuring the residual percentage of lymph node T cells expressing the Lyt-1.1 marker specific to recipient DBA/2 haplotype. The content of T cells of donor origin was high (82.3% to 88.9%) in all groups of mice regardless of the source of cells used for transplantation (Table 3). The percentages of CD4+ T cells as well as of Ig+ B cells were not significantly different from those found in normal B10.D2 mice and in BM-engrafted F1 mice, showing that the recovery was complete for these subpopulations 2 to 3 months after the graft. However, the percentages of CD8+ T cells remained significantly reduced (P< .05) in all grafted groups.
Reconstitution in the Lymph Nodes of F1 Recipient Mice Engrafted With Adult BM or NBB Cells
| LN Cells from . | Percentage of Positive Cells ± SD . | |||
|---|---|---|---|---|
| Donor Origin3-150 . | CD4+ . | CD8+ . | Ig+ . | |
| Normal B10.D2 mice | 98.3 ± 2.5 | 35.2 ± 5.1 | 22.8 ± 2.9 | 37.4 ± 2.0 |
| Adult BM-engrafted F1 recipients | 88.9 ± 0.6 | 34.1 ± 7.9 | 17.5 ± 4.83-151 | 41.0 ± 2.8 |
| NBB-engrafted F1 recipients | ||||
| Day 0 | 82.8 ± 4.9 | 38.6 ± 10.2 | 17.8 ± 2.03-151 | 35.2 ± 9.6 |
| Day 2 | 87.9 ± 1.7 | 31.9 ± 2.7 | 17.0 ± 1.53-151 | 45.8 ± 3.3 |
| Day 5 | 83.4 ± 2.4 | 35.4 ± 4.9 | 15.8 ± 2.03-151 | 43.1 ± 3.4 |
| LN Cells from . | Percentage of Positive Cells ± SD . | |||
|---|---|---|---|---|
| Donor Origin3-150 . | CD4+ . | CD8+ . | Ig+ . | |
| Normal B10.D2 mice | 98.3 ± 2.5 | 35.2 ± 5.1 | 22.8 ± 2.9 | 37.4 ± 2.0 |
| Adult BM-engrafted F1 recipients | 88.9 ± 0.6 | 34.1 ± 7.9 | 17.5 ± 4.83-151 | 41.0 ± 2.8 |
| NBB-engrafted F1 recipients | ||||
| Day 0 | 82.8 ± 4.9 | 38.6 ± 10.2 | 17.8 ± 2.03-151 | 35.2 ± 9.6 |
| Day 2 | 87.9 ± 1.7 | 31.9 ± 2.7 | 17.0 ± 1.53-151 | 45.8 ± 3.3 |
| Day 5 | 83.4 ± 2.4 | 35.4 ± 4.9 | 15.8 ± 2.03-151 | 43.1 ± 3.4 |
LN cells from normal B10.D2 mice or from F1 recipients collected 2 to 3 months after grafting with B10.D2 adult BM cells or B10.D2 NBB cells taken on days 0, 2, and 5 after birth. Cells were labeled with PE-conjugated anti-CD4, FITC-conjugated anti-CD8 and FITC-conjugated GAM MoAbs. Values are means ± SD for 3 to 8 mice.
For chimerism evaluation, the percentage of cells of B10.D2 origin was estimated by the following calculation: 100-percentage of cells stained with anti–Lyt-1.1 MoAb specific of DBA/2 recipient origin. Anti–Lyt-1.1 MoAb was shown by FITC-conjugated GAM MoAb.
Significantly reduced compared with normal B10.D2 mice (Student’st test P < .05).
Absence of a GVL effect in NBB-engrafted F1 recipients.
To investigate whether a GVL effect exists or not in F1 mice grafted with newborn blood, 105 P815 tumor cells were injected intravenously into recipients 1 day before irradiation and reconstitution with NBB collected on days 0, 2, and 5 after birth. The incidence of tumor relapse was compared with that of F1 recipients grafted with TCD BM cells of B10.D2 origin that did not develop lethal GVHD (Fig 1) and with that of F1 recipients grafted with F1 BM plus spleen cells (ISO). Previous data19 and Fig 2 showed that seven of eight TCD BM-grafted mice receiving 105 P815 cells died of leukemia with a median survival time (MST) of 30 days. This mortality rate is not significantly different (P = .13) from that of ISO-grafted mice (MST = 25 days; Fig 2). All mice grafted with day-2 and day-5 NBB cells died quickly (MST = 12 and 11 days, respectively) and only 2 of 14 mice grafted with day-0 NBB cells survived (MST = 18 days). The survival of day-2 and day-5 NBB-grafted mice but not of day-0 NBB-grafted mice was significantly shorter than that of TCD BM-grafted mice (P < .001). All recipients dying before day 12 had a highly atrophic spleen, indicating the absence of engraftment. From 2 weeks after P815 injection, irradiation, and grafting, most recipients, regardless of the origin of the grafted cells, died with evidence of tumor metastasis in the spleen and liver, thus showing the absence of a GVL effect in NBB-grafted mice as in TCD BM- and ISO-grafted mice.
Effect on GVHD development of delayed infusion of donor spleen cells to grafted recipients.
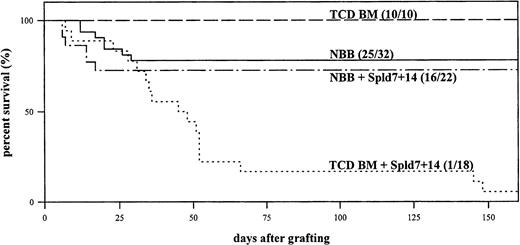
Several studies have reported a beneficial antitumoral effect after injection of donor lymphocytes several days or weeks after TCD BM transplantation, but GVHD was frequently described.20-22.We first examined whether infusion of 106 B10.D2 donor spleen cells 7 and 14 days after transplantation of day-0 NBB, or of adult TCD BM, induced lethal GVHD. Because engraftment was better with day-0 than with day-2 NBB cells, and because their phenotype and functional characteristics do not differ significantly, we used day-0 NBB as the source of transplantable cells for the subsequent experiments. We eliminated day-5 NBB cells because they induced some degree of GVHD. The survival of F1 recipients grafted with NBB alone (78%) was not significantly affected by the two additional injections of donor splenocytes (73%) (Fig 3). Conversely, the injection of splenocytes into F1 recipients grafted with TCD BM significantly (P < .001) increased the percentage of mortality (95% with an MST = 48 days) by inducing GVHD.
In vivo survival of lethally irradiated (DBA/2 × B10.D2)F1 mice grafted with B10.D2 cells from adult TCD BM (– –) or from NBB (––) collected on the day of birth. 106B10.D2 donor splenocytes (Spl) were injected or not 7 and 14 days after the graft of NBB (–·–) or of TCD BM (···) cells. Mortality was recorded daily and mice were examined for the presence of clinical GVHD (number of live mice/total number of mice).
In vivo survival of lethally irradiated (DBA/2 × B10.D2)F1 mice grafted with B10.D2 cells from adult TCD BM (– –) or from NBB (––) collected on the day of birth. 106B10.D2 donor splenocytes (Spl) were injected or not 7 and 14 days after the graft of NBB (–·–) or of TCD BM (···) cells. Mortality was recorded daily and mice were examined for the presence of clinical GVHD (number of live mice/total number of mice).
Influence of delayed infusion of NBB-grafted recipients with donor spleen cells on GVL effect.
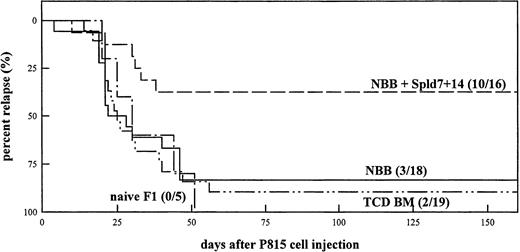
P815 tumor cells (103) were administered intravenously to F1 recipients reconstituted 3 months earlier with NBB alone, NBB plus splenocytes, or TCD BM cells. Relapse rate was recorded and compared with that of naive F1 mice injected with the same number of P815 cells (Fig 4). Addition of splenocytes conferred significant protection against tumor growth in 10 out 16 mice (62%) grafted with NBB cells when compared with recipients grafted with NBB (P = .016) or with TCD BM (P = .004) cells alone.
Percent mortality by tumor relapse of lethally irradiated (DBA/2 × B10.D2)F1 mice grafted with B10.D2 cells from day-0 NBB either alone (––) or mixed with splenocytes (NBB+Spl, – –) or from TCD BM (–··–) alone. Naive F1 mice served as controls (–·–). All recipient mice were injected intravenously with 103 P815 tumor cells 2 to 3 months after grafting. Mortality was recorded daily and mice were examined for the presence of tumor metastasis (number of live mice/total number of mice).
Percent mortality by tumor relapse of lethally irradiated (DBA/2 × B10.D2)F1 mice grafted with B10.D2 cells from day-0 NBB either alone (––) or mixed with splenocytes (NBB+Spl, – –) or from TCD BM (–··–) alone. Naive F1 mice served as controls (–·–). All recipient mice were injected intravenously with 103 P815 tumor cells 2 to 3 months after grafting. Mortality was recorded daily and mice were examined for the presence of tumor metastasis (number of live mice/total number of mice).
Comparison of lymphokine messenger RNA (mRNA) expression by Con A-stimulated adult BM, spleen, and NBB cells.
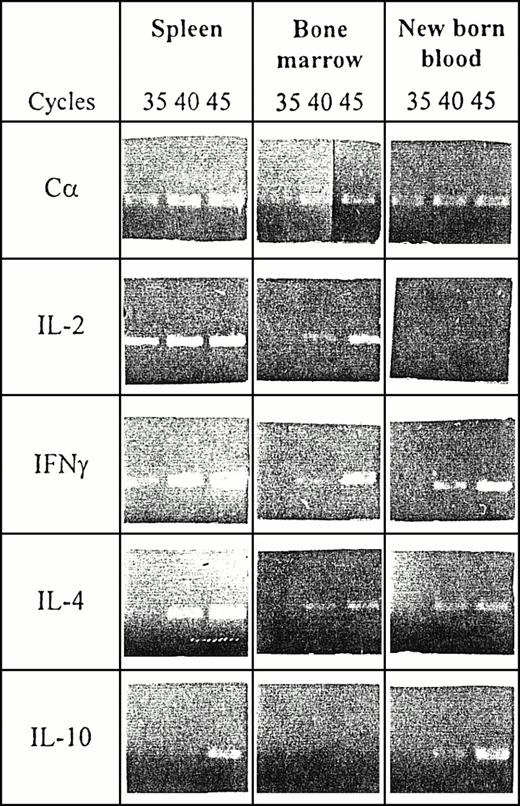
To understand why no GVHD developed after injection of splenocytes into mice grafted with NBB, as opposed to mice grafted with BM, we postulated that some cells present in NBB possess regulatory properties expressed through secreted soluble interleukins. It was found that on anti-CD3 stimulation early postnatal T cells produce abundant IL-4 that inhibited IL-2 secretion in response to primary stimulation in vitro.15 We therefore studied the lymphokine mRNA expression profile of BM and NBB cells on Con A stimulation and compared it with that of adult spleen cells. mRNA was extracted from NBB collected on the day of birth and from adult BM cells and spleen cells after stimulation with Con A for 24 hours. Lymphokine mRNA expression level was first measured by semiquantitative RT-PCR amplification by using IL-2, IFNγ, IL-4, IL-10, and Cα-specific primers. PCR products were collected after 35, 40, and 45 cycles of amplification and the results of mRNA expression are summarized in Fig 5. Approximately comparable levels of Cα mRNA were obtained with mRNA derived from spleen and NBB cells and slightly less for mRNA derived from BM cells. IL-2 and IFNγ mRNA were detectable in stimulated spleen cells after 35 cycles whereas IL-4 and IL-10 mRNA appeared after 40 cycles but at very low levels in the case of IL-10. Stimulated BM cells expressed similar but low levels of mRNA transcripts for IL-2, IFNγ, and IL-4 (detectable after 40 cycles) but not at all for IL-10. NBB cells expressed IFNγ and IL-4 mRNA after 40 cycles and very low levels of IL-2 mRNA transcripts at 45 cycles. In contrast, IL-10 transcripts were detectable after 40 cycles at higher levels than in spleen cells.
IL gene expression in adult spleen, BM, and in NBB. Cells from spleen, BM, and NBB were stimulated with Con A for 24 hours and mRNA extracted. Semiquantitative RT-PCR amplification was performed on cDNA using C-, IL-2–, IFNγ-, IL-4–, and IL-10–specific primers. PCR products were analyzed on agarose gel after 35, 40, and 45 cycles of amplification.
IL gene expression in adult spleen, BM, and in NBB. Cells from spleen, BM, and NBB were stimulated with Con A for 24 hours and mRNA extracted. Semiquantitative RT-PCR amplification was performed on cDNA using C-, IL-2–, IFNγ-, IL-4–, and IL-10–specific primers. PCR products were analyzed on agarose gel after 35, 40, and 45 cycles of amplification.
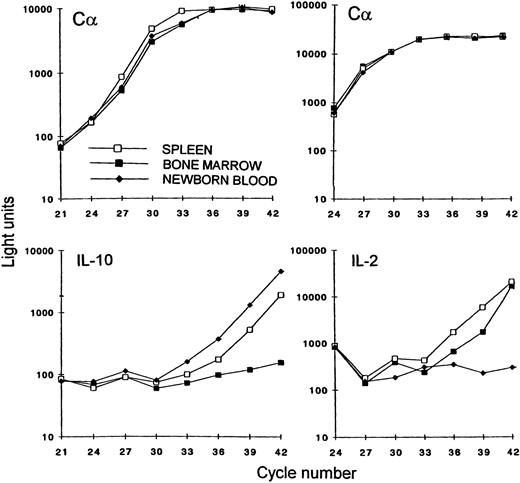
A quantitative RT-PCR assay was further developed19 to estimate the relative levels of mRNA for IL-2 and IL-10 and compare the number of amplification cycles necessary to generate similar amounts of cDNA PCR products. For a similar level of Cα mRNA, NBB cells expressed more IL-10 mRNA (two-cycle difference corresponding to a fourfold increase) than spleen cells, and BM cells did not reach detectable levels of mRNA (Fig 6). IL-2 mRNA was not detected in NBB cells whereas spleen cells expressed approximately four times more mRNA than BM cells.
Quantitation of C, IL-2, and IL-10 mRNA by RT-PCR amplification. At sequential cycle numbers, cDNA PCR samples synthesized from mRNA, prepared from adult spleen (□), adult BM (▪), and NBB (⧫). Con A-stimulated cells were collected and transferred onto avidin-coated microtiter plates. Quantitation of the amplified products was performed in a liquid-hybridization–ELISA assay with luminometry readings.
Quantitation of C, IL-2, and IL-10 mRNA by RT-PCR amplification. At sequential cycle numbers, cDNA PCR samples synthesized from mRNA, prepared from adult spleen (□), adult BM (▪), and NBB (⧫). Con A-stimulated cells were collected and transferred onto avidin-coated microtiter plates. Quantitation of the amplified products was performed in a liquid-hybridization–ELISA assay with luminometry readings.
DISCUSSION
Our experimental model was designed to evaluate the GVHD incidence and the antileukemic potential associated with the transplantation of PB from newborn mice in comparison with the transplantation of T-cell–depleted adult BM. We previously showed that the blood of one newborn mouse contained a sufficient number of progenitors to reconstitute lethally irradiated F1 recipients with about 80% engraftment.13 In the genetic combination used, donor and recipient differed in multiple mHAgs and the injection of BM mixed with mature lymphoid cells caused 100% GVHD mortality, whereas injection of TCD BM or NBB cells generated no GVHD signs. The phenotypic and functional immaturity of T cells from NBB explained these results13 and prompted us to investigate the influence of T-cell maturation during the neonatal period and of the acquisition of immune reactivity on the degree of engraftment, the incidence of GVHD, and the antileukemic potential.
There was a progressive increase in NBB of CD4+ T cells expressing TCR α/β and a concomitant decrease in CD4+CD8+ T cells. These observations are in accordance with studies of T-cell maturation that identified CD4+CD8+ immature T cells in lymph nodes but not in the spleens of newborn mice.16 These CD4+CD8+ cells are thymus-derived and exported during the first few days of life. They had dropped in number by day 8 and disappeared by day 10.16 The percentage of SCA-1+ progenitor cells fluctuated but differences were not statistically significant. Simultaneously, T cells acquired the capacity to proliferate on stimulation with PHA and allogeneic cells, although less so than adult PB. The degree of engraftment of F1 mice grafted with day-2 NBB was significantly reduced, probably because of graft failure shown on autopsy by the absence of cells in lymphoid organs. In contrast, F1 recipients grafted with day-5 NBB reconstituted but some mice died with clinical signs of GVHD. We interpreted these data by postulating that the presence of 13% of mature T cells in the blood at that time favors the engraftment but induces a partial antihost response.
The antileukemic potential was tested by intravenously injecting 105 P815 cells into F1 recipients 1 day before lethal irradiation (which eliminated 90% to 99% of tumor cells) and cell reconstitution. This protocol was first used to mimic the human situation in which tumor cells pre-exist in the patient before conditioning and transplantation. At this P815 dose, 87% of recipients grafted with TCD BM cells and 93% grafted with F1 isogeneic cells relapsed with evidence of spleen and liver metastasis because of the absence of antihost T-cell responses. Nearly all the recipients grafted with day-2 and day-5 NBB cells died of graft failure before day 15. To explain this observation, we postulate that tumor cell growth prevented the cell reconstitution of lymphoid organs by NBB progenitors that are more immature and therefore require more time than BM progenitors to engraft. Mice grafted with day-0 NBB cells that died after day 18 exhibited evidence of tumor metastasis. In this case, the functional unresponsiveness of T cells was responsible for the lack of GVL effect for ISO- and TCD BM-engrafted mice.
It has been reported in experimental and human BMT, that a GVL effect can be generated by the delayed infusion of donor T cells,20-22 but a substantial incidence of GVHD is associated with this therapy. In our model, injection of 106 donor B10.D2 spleen cells 7 and 14 days after the graft of adult TCD BM cells induced marked GVHD that was lethal for 17 of 18 recipients. Interestingly, the delayed splenocytes treatment applied to F1 recipients engrafted with day-0 NBB cells did not cause GVHD. To explain this observation, we hypothesized that an active suppression mediated by neonatal cells or factors is responsible for the tolerization of mature T cells specific for host mHAgs. It was shown that CD4+ T cells from neonatal lymph nodes secrete large amounts of IL-4 on stimulation with anti-CD3 that inhibit IL-2 production by adult T cells.15 In addition, susceptibility of newborns to transplantation tolerance has been attributed to their high level of IL-4 production.23 We therefore compared the pattern of cytokines produced by NBB and BM cells. We found that BM cells expressed a moderate amount of IL-2, IFNγ, and IL-4 mRNA but no IL-10 mRNA, whereas NBB cells expressed mRNA transcripts for IFNγ, IL-4, and IL-10 but very little for IL-2. Studies in mice showed that in newborn spleen or lymph node cells, the secretion of interleukins15 or the expression of interleukin genes17 on stimulation was low for IL-2, IFNγ, and IL-10, and high for IL-4 and thus differed from that of peripheral NBB cells. Interestingly, single-positive CD4+ thymocytes differ from their progeny, naive peripheral CD4+ cells, because they produce mainly IL-4, IL-10, and IFNγ, but little IL-2.17,24 In view of the presence of CD4+CD8+ cells and of the lymphokine pattern that we found, it appears that NBB cells resemble thymocytes more than peripheral cells. This hypothesis is consistent with results showing that the functional phenotype of recent thymic emigrants represents the exclusive T-cell type in the periphery during the first week of life both in mice15,17 and in humans.4
Comparison between BM and NBB cells showed no difference in IL-4 mRNA expression and thus excludes the implication of this cytokine in the GVHD inhibition. In contrast, IL-2 mRNA is expressed in BM cells and not in NBB cells and, conversely, IL-10 mRNA is expressed in NBB cells and not in BM cells. Although lymphokine protein was not measured in the assays, it is reasonable to assume that mRNA expression for a particular lymphokine indicates that the corresponding protein was secreted. IL-10 is known to be synthesized by Th2 cells or by other types of cells such as B cells, macrophages, and mast cells.25 It immunosuppresses cytokine production and antigen-specific proliferation of Th1 cells26 and also induces the differentiation of a new regulatory CD4+ T-cell subset.27 Recent data showed that chronic activation of both human and murine CD4+ T cells in the presence of IL-10 gives rise to CD4+ T-cell clones of low proliferative capacity, producing low levels of IL-2 and no IL-4.27 These antigen-specific T-cell clones suppress the proliferation of CD4+ T cells in response to antigen and prevent a pathogenic T-cell response. In our model, IL-10 produced by NBB cells when stimulated by incompatible host DBA/2 mHAgs might inhibit the activation of mature T splenocytes injected after the graft of NBB cells, and thus prevent induction of GVHD. Conversely, the delayed infused splenic T cells were able to induce GVHD when combined with adult BM cells that are unable to synthesize IL-10. This finding does not exclude the participation of other immunosuppressive cytokines such as transforming growth factor (TGF)β not measured in this work.
We further showed that the delayed infusion of splenocytes induced resistance to P815 tumor growth in 62% F1 mice grafted 2 to 3 months earlier with NBB cells, whereas injection of the same dose of tumor cells induced relapse in 83% mice grafted with NBB cells alone. Most importantly, these experiments point to a dissociation between the capacity of mature T cells to achieve GVHD and GVL reactions. The restricted tissue expression of some mHAgs10,28,29raises the possibility that mHAgs present on leukemic cells are not expressed on normal cell targets of GVHD and hence that effector T cells implicated in GVHD differ from those implicated in GVL. To explain why this adoptive treatment induced a GVL effect but no GVHD in NBB-engrafted mice, we hypothesized that donor T cells that became tolerant to host mHAgs implicated in GVHD,13 further tolerized (infectious tolerance) delayed infused splenic mature T cells specific of host mHAgs but not of T cells specific of tissue antigens expressed on P815 mastocytoma cells. Those T cells were not tolerized because of the absence of tumor cells at the time of mature T-cell infusion, thus explaining the preserved GVL effect.
Despite phenotypic and functional differences, murine NBB and human CB cells share common immunological features such as a low capacity to induce a GVHD,1,2,9 alterations in the cytokine production pattern,7,12,30-32 and presence of suppressor T cells or factors.33,34 Although recorded with a model that does not exactly reflect the human situation, the present results suggest that, in terms of GVHD incidence, the delayed infusion of mature T cells as post-transplant adoptive immunotherapy would be more effective in eliminating residual disease or in treating leukemia relapse when applied after CB transplantation than after BMT. A recent clinical report35 supports this assumption because complete remission was achieved in a child with acute lymphoblastic leukemia who, following CB transplantation, was administered adoptive immunotherapy consisting of several infusions of donor PB leukocytes.
ACKNOWLEDGMENT
We thank N. Riché and L. Majbruch for technical assistance and J. Roué for typing the manuscript.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal