Abstract
This study reassesses the occurrence of Epstein-Barr virus (EBV) diversity and coinfection versus dominance of a single viral strain within immunocompetent normal carriers. Polymerase chain reaction analysis of several different polymorphic loci of the EBV genome was performed on collections of peripheral blood mononuclear cells and multiple lymphoid and epithelial tissues of the same individuals. Autopsy specimens from 15 individuals who died of causes unrelated to EBV infection served as normal viral carriers. Unexpectedly, coinfection of multiple distinct strains of EBV of the same type (usually type 1) and less frequently of both types 1 and 2 was found to be very high within individual viral carriers. These data indicate that coinfection with multiple EBV strains is much more prevalent in normal carriers than previously appreciated, which in turn has direct implications on EBV persistence, host–viral interaction and pathogenesis.
Persistence of Epstein-Barr virus (EBV) in healthy immunocompetent viral carriers has been thought to be characterized by dominance of a single EBV-transforming strain.1,2 In contrast, immunocompromised male homosexual cohorts infected with human immunodeficiency virus (HIV)3 and HIV-infected hemophilic individuals4 are frequently infected with multiple viral strains, both of the same (usually type 1) and different (types 1 and 2) types. It has been suggested that the immune response to an existing EBV strain may protect the immunocompetent host from infection with additional exogenous viral strains.3,4 Although earlier data of healthy donors were derived from analysis of virus isolates rescued from the peripheral blood mononuclear cells (PBMCs) and throat washings of healthy donors into lymphoblastoid cell lines (LCLs),1 direct polymerase chain reaction (PCR) analysis of EBV genomes in normal viral carriers has demonstrated the presence of multiple viral strains in some individuals.5-7
Sixbey et al5 were the first group to report the detection of both types (types 1 and 2) of EBV by PCR in the throat washings of 9% of healthy viral carriers and provided evidence for EBV coinfection in immunocompetent hosts. Apolloni and Sculley6 also reported the detection of both EBV types by PCR in 14% of throat washings and 27% of PBMCs of healthy viral carriers. PCR analysis of the EBV genomes contained in normal nasal tissues and nasal T/natural killer (NK)-cell lymphomas of our population by Chiang et al7 suggested the presence of multiple viral infection in 29% of immunocompetent individuals and selection of particular EBV strains in nasal T/NK-cell lymphomas. The present study reassessed whether immunocompetent normal individuals can be infected with more than 1 strain of EBV. PCR analysis of a large panel of polymorphic EBV genome markers was performed on PBMCs and different lymphoid and epithelial tissues from normal individual viral carriers for the identification of EBV genotype. The outcome of this study has important implications for EBV persistence and pathogenesis.
Study design
Case selection
Fifteen autopsy subjects were selected according to the following criteria8: absence of clinical symptoms suggestive of active EBV infection; absence of chronic debilitating illness (eg, malignancy, diabetes mellitus); and absence of immunosuppression. Tissue blocks from different lymphoid and epithelial sites were collected from autopsies performed at the Department of Pathology, University of Hong Kong, Queen Mary Hospital, Hong Kong. All patients were Chinese. These multiple autopsy specimens of these viral carriers (designated VC1-15) served as sources for analysis of EBV strains in normal viral carriers in our population. Peripheral blood specimens were available from VC1-7.
PCR-based genotype identification of EBV
DNA was extracted from PBMCs and from multiple lymphoid and epithelial tissues of individual viral carriers, and 0.5 μg genomic DNA was amplified by PCR using EBV genome-specific primers for a large panel of polymorphic gene markers (EBV subtypes [EBNA2, EBNA3C],9 LMP1 30 bp deletion,10 LMP1 33 bp repeats,11 and BamHI F2 and Z12polymorphism). The PCR conditions used for EBNA typing and LMP (deletion and repeats) study were as described in Chiang et al,7 and for BamHI F/f polymorphism analysis were as described in Khanim et al.2 For BamHI Z/Z* polymorphism, primer Zc was used as the internal probe as described by Chen et al.12 The EBV-positive cell lines B95-8 and Jijoye were used as controls.7 DNA extracted from a frozen block of rat splenic tissue was also used as a negative control. As a positive amplification control, primers (PC03 and PC04) for β-globin gene were used in PCR analysis for any sample negative for EBV, as described by Cheung et al.8
Results and discussion
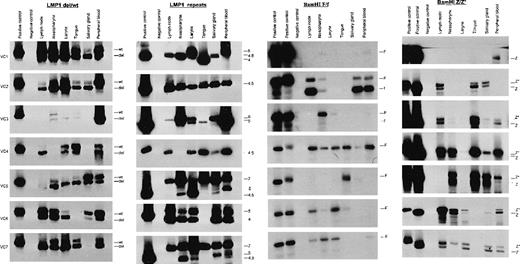
The PCR-based identification of EBV genotype of PBMCs and multiple lymphoid and epithelial tissues obtained from 15 normal viral carriers showed clearly that multiple independent EBV strains of the same type (usually type 1) could be found within virtually all carriers; less frequently, coinfection with both types 1 and 2 strains was detected in 8 of 15 (53%) of the carriers (Figure 1and Table 1). The BamHI F restriction fragment length polymorphism was informative in showing mixed infection of F and f viral variants in 8 of 15 (53%) viral carriers, and almost every viral carrier (14 of 15, 93%) harbored mixed infections of LMP1 deletion and wild-type variants. The latter results confirm our previous findings of frequent mixed deletion and wild-type LMP1 variants in normal nasal tissue.7 Multiple PCR bands of LMP1 repeats in 12 of 15 (80%) and the codetection of Z and Z* variants in 5 of 7 (71%) carriers could have arisen from intrastrain recombination/deletion during viral replication. The Z and Z* variants frequently coexist at both epithelial and lymphoid sites, which did not support the data of Chen et al12 showing epithelial specific viral strains.
Genotype identification of EBV.
Direct PCR analysis was used to determine the genotype identification of EBV of several different polymorphic loci of the EBV genome in peripheral blood mononuclear cells (PBMCs) and multiple lymphoid and epithelial tissues obtained at different anatomic sites of the normal individual viral carriers (VC1-7). Multiple viral strains were detected at different tissues and PBMCs within individual viral carriers. Considerable variability in amplification of viral strains was also noted at different anatomic sites within the same person. Coresident viruses were designated as distinct strains when PCR analysis detected either (i) both type 1 and 2 viruses or (ii) mixed infection of both deletion and wild-type LMP1 variants or (iii) mixed infection of both BamHI F and f.
Genotype identification of EBV.
Direct PCR analysis was used to determine the genotype identification of EBV of several different polymorphic loci of the EBV genome in peripheral blood mononuclear cells (PBMCs) and multiple lymphoid and epithelial tissues obtained at different anatomic sites of the normal individual viral carriers (VC1-7). Multiple viral strains were detected at different tissues and PBMCs within individual viral carriers. Considerable variability in amplification of viral strains was also noted at different anatomic sites within the same person. Coresident viruses were designated as distinct strains when PCR analysis detected either (i) both type 1 and 2 viruses or (ii) mixed infection of both deletion and wild-type LMP1 variants or (iii) mixed infection of both BamHI F and f.
Results of PCR-based analysis of the EBV genotype of the normal viral carriers (VC1-15)
| Virus Carrier . | Sex/ Age . | Anatomic Sites . | Types T1/T2 . | LMP1 wt/del . | LMP1 Repeats . | BamHI F/f . | BamHI Z/Z* . |
|---|---|---|---|---|---|---|---|
| VC 1 | F/73 | Mediastinal lymph node | T1 | wt/del | 4.5 | — | — |
| Nasopharynx | T1 | wt/del | 4.5 | F | — | ||
| Larynx | — | wt/del | 5 | — | — | ||
| Anterior tongue | T1 | wt/del | 4 | — | — | ||
| Submandibular gland | T1 | del | 4.5 | — | — | ||
| Peripheral blood | — | wt/del | 5 | F | Z | ||
| VC 2 | F/89 | Mediastinal lymph node | T1 | wt/del | 4.5 | F/f | Z/Z* |
| Nasopharynx | T1 | del | 4.5 | F/f | Z* | ||
| Larynx | T1 | wt/del | 4.5 | — | Z* | ||
| Anterior tongue | T1 | wt/del | 4.5 | F/f | Z/Z* | ||
| Submandibular gland | T1 | wt/del | 4.5 | F/f | Z/Z* | ||
| Peripheral blood | T1 | wt/del | 4.5 | F/f | — | ||
| VC 3 | F/72 | Mediastinal lymph node | — | — | 6 | — | Z/Z* |
| Nasopharynx | T1 | wt/del | 6 | F | Z/Z* | ||
| Larynx | T1 | wt/del | 5/6 | F | Z/Z* | ||
| Anterior tongue | — | wt/del | 5 | — | Z/Z* | ||
| Submandibular gland | T1 | — | 6 | — | Z/Z* | ||
| Peripheral blood | T1 | del | 5 | F | Z/Z* | ||
| VC 4 | M/82 | Mediastinal lymph node | T1/T2 | wt/del | 4.5 | F | Z/Z* |
| Nasopharynx | T1/T2 | wt/del | — | F | Z/Z* | ||
| Larynx | T1/T2 | wt/del | 4.5 | F | Z* | ||
| Anterior tongue | T1/T2 | wt/del | 4.5 | F | Z* | ||
| Submandibular gland | T1/T2 | wt/del | 4.5 | F | Z* | ||
| Peripheral blood | T1/T2 | wt/del | 4.5 | F | Z* | ||
| VC 5 | M/77 | Mediastinal lymph node | T1 | del | 7 | F | — |
| Nasopharynx | T1 | wt/del | 4.5/7 | — | Z/Z* | ||
| Larynx | T1 | wt/del | 4.5/7 | F | Z/Z* | ||
| Anterior tongue | T1 | wt/del | 7 | F | Z/Z* | ||
| Submandibular gland | T1 | wt/del | 4.5/7 | F | Z/Z* | ||
| Peripheral blood | T1 | wt/del | 5/7 | — | Z | ||
| VC 6 | M/68 | Mediastinal lymph node | T1/T2 | wt/del | 4/5 | F | Z/Z* |
| Nasopharynx | T1/T2 | wt/del | 4/5 | F | Z/Z* | ||
| Larynx | T1/T2 | wt/del | 4/5 | F | Z/Z* | ||
| Anterior tongue | nd | nd | nd | nd | nd | ||
| Submandibular gland | T1/T2 | wt/del | 4/5 | F | Z/Z* | ||
| Peripheral blood | T1 | wt/del | 4/5 | F | Z/Z* | ||
| VC 7 | F/83 | Mediastinal lymph node | T1 | del | 7 | F | Z/Z* |
| Nasopharynx | T1/T2 | wt/del | 4.5/7 | F | Z/Z* | ||
| Larynx | T1 | wt/del | 4.5/7 | F | Z/Z* | ||
| Anterior tongue | T2 | wt/del | 7 | F | — | ||
| Submandibular gland | T2 | wt/del | 5/7 | F | Z/Z* | ||
| Peripheral blood | T1/T2 | wt/del | 5/7 | F | Z/Z* | ||
| VC 8 | M/57 | Cervical lymph node | T1 | wt/del | 4/4.5 | F | nd |
| Mediastinal lymph node | T1 | del | 4/4.5 | F | nd | ||
| Para-aortic lymph node | T1 | wt/del | — | F | nd | ||
| Nasopharynx | T1 | del | 4 | F | nd | ||
| Thyroid | T1 | wt/del | 4.5 | — | nd | ||
| Tonsil (palatine) | T1 | wt/del | 4/4.5 | F | nd | ||
| Submandibular gland | T1 | wt/del | 4.5 | — | nd | ||
| Spleen | T1 | wt/del | 4.5 | — | nd | ||
| Thymus | T1 | wt/del | — | — | nd | ||
| VC 9 | F/70 | Cervical lymph node | T1 | wt | 4.5 | F | nd |
| Mediastinal lymph node | T1 | wt | 4.5 | F | nd | ||
| Para-aortic lymph node | — | wt | — | F | nd | ||
| Nasopharynx | T1 | wt | 4.5 | F/f | nd | ||
| Thyroid | — | wt | 4.5 | — | nd | ||
| Tonsil (palatine) | T1 | wt | 4.5 | F | nd | ||
| Submandibular gland | — | wt | 4.5 | — | nd | ||
| Spleen | — | wt | 4.5 | — | nd | ||
| VC 10 | F/26 | Cervical lymph node | T1 | — | 4.5/5 | F/f | nd |
| Mediastinal lymph node | — | — | 4.5 | F/f | nd | ||
| Para-aortic lymph node | T1 | — | 4.5 | — | nd | ||
| Nasopharynx | T1 | — | 4.5/5 | F/f | nd | ||
| Thyroid | T1 | — | 4.5 | — | nd | ||
| Tonsil (palatine) | T1 | wt/del | 4.5/5 | F/f | nd | ||
| Tonsil (lingual) | T1 | wt/del | 4.5 | — | nd | ||
| Lung (central) | T1/T2 | del | 4.5 | — | nd | ||
| Lung (peripheral) | T1 | del | 4.5 | — | nd | ||
| Spleen | T1 | — | 4.5 | — | nd | ||
| Thymus | T1 | — | 4.5 | — | nd | ||
| VC 11 | M/40 | Cervical lymph node | T1 | wt/del | — | — | nd |
| Nasopharynx | T1/T2 | wt/del | 4.5 | F/f | nd | ||
| Larynx | T1 | wt | 4.5/5/6 | — | nd | ||
| Oropharynx | T1 | — | 4.5 | — | nd | ||
| Tonsil | T1 | wt | 4.5 | — | nd | ||
| Parotid gland | — | wt/del | — | F | nd | ||
| Submandibular gland | T1 | del | 4/4.5/5/6 | F | nd | ||
| Penis | T1 | wt | 4.5/5/6 | — | nd | ||
| VC 12 | M/33 | Cervical lymph node | — | wt/del | — | — | nd |
| Nasopharynx | T1 | wt/del | 4.5/5 | F | nd | ||
| Larynx | — | del | — | — | nd | ||
| Oropharynx | — | wt/del | — | — | nd | ||
| Tonsil | — | del | 4.5 | F/f | nd | ||
| Parotid gland | T1 | del | 4.5 | — | nd | ||
| Submandibular gland | T1 | del | 4.5 | — | nd | ||
| Penis | — | del | — | F/f | nd | ||
| VC 13 | M/69 | Cervical lymph node | T1 | wt/del | 4.5 | F/f | nd |
| Nasopharynx | T1 | del | 4/4.5/5/6 | F/f | nd | ||
| Larynx | — | wt/del | — | — | nd | ||
| Oropharynx | — | wt/del | — | — | nd | ||
| Tonsil | T1 | wt/del | 4.5 | F/f | nd | ||
| Parotid gland | T1/T2 | wt/del | 4.5 | F | nd | ||
| Submandibular gland | T1 | wt/del | 4.5 | — | nd | ||
| Penis | T1 | wt/del | 4.5 | — | nd | ||
| VC 14 | M/88 | Cervical lymph node | T1/T2 | del | 4.5/5/6 | F | nd |
| Mediastinal lymph node | T1 | del | 5/6 | F | nd | ||
| Para-aortic lymph node | T1 | del | 5/6 | F | nd | ||
| Thyroid | T1 | del | 4.5 | F | nd | ||
| Lung (peripheral) | T1 | del | 4/4.5/6 | F | nd | ||
| Lung (central) | T1 | del | 4/4.5/6 | F | nd | ||
| Tonsil (palatine) | — | wt/del | 4.5 | — | nd | ||
| Tonsil (lingual) | T1 | del | 4.5/5/6/7 | F/f | nd | ||
| Submandibular gland | — | — | 4.5/6 | — | nd | ||
| Spleen | — | del | 4.5 | F | nd | ||
| VC 15 | F/67 | Cervical lymph node | T1 | del | 4.5/6 | F | nd |
| Nasopharynx | T1 | wt/del | 4.5 | — | nd | ||
| Larynx | T1 | — | — | F/f | nd | ||
| Oropharynx | — | del | — | — | nd | ||
| Tonsil | T1/T2 | del | 4.5/6 | F | nd | ||
| Parotid gland | T1 | — | 4.5 | — | nd | ||
| Submandibular gland | T1 | — | 4.5 | — | nd | ||
| Cervix | T1 | — | 4.5/6 | F | nd |
| Virus Carrier . | Sex/ Age . | Anatomic Sites . | Types T1/T2 . | LMP1 wt/del . | LMP1 Repeats . | BamHI F/f . | BamHI Z/Z* . |
|---|---|---|---|---|---|---|---|
| VC 1 | F/73 | Mediastinal lymph node | T1 | wt/del | 4.5 | — | — |
| Nasopharynx | T1 | wt/del | 4.5 | F | — | ||
| Larynx | — | wt/del | 5 | — | — | ||
| Anterior tongue | T1 | wt/del | 4 | — | — | ||
| Submandibular gland | T1 | del | 4.5 | — | — | ||
| Peripheral blood | — | wt/del | 5 | F | Z | ||
| VC 2 | F/89 | Mediastinal lymph node | T1 | wt/del | 4.5 | F/f | Z/Z* |
| Nasopharynx | T1 | del | 4.5 | F/f | Z* | ||
| Larynx | T1 | wt/del | 4.5 | — | Z* | ||
| Anterior tongue | T1 | wt/del | 4.5 | F/f | Z/Z* | ||
| Submandibular gland | T1 | wt/del | 4.5 | F/f | Z/Z* | ||
| Peripheral blood | T1 | wt/del | 4.5 | F/f | — | ||
| VC 3 | F/72 | Mediastinal lymph node | — | — | 6 | — | Z/Z* |
| Nasopharynx | T1 | wt/del | 6 | F | Z/Z* | ||
| Larynx | T1 | wt/del | 5/6 | F | Z/Z* | ||
| Anterior tongue | — | wt/del | 5 | — | Z/Z* | ||
| Submandibular gland | T1 | — | 6 | — | Z/Z* | ||
| Peripheral blood | T1 | del | 5 | F | Z/Z* | ||
| VC 4 | M/82 | Mediastinal lymph node | T1/T2 | wt/del | 4.5 | F | Z/Z* |
| Nasopharynx | T1/T2 | wt/del | — | F | Z/Z* | ||
| Larynx | T1/T2 | wt/del | 4.5 | F | Z* | ||
| Anterior tongue | T1/T2 | wt/del | 4.5 | F | Z* | ||
| Submandibular gland | T1/T2 | wt/del | 4.5 | F | Z* | ||
| Peripheral blood | T1/T2 | wt/del | 4.5 | F | Z* | ||
| VC 5 | M/77 | Mediastinal lymph node | T1 | del | 7 | F | — |
| Nasopharynx | T1 | wt/del | 4.5/7 | — | Z/Z* | ||
| Larynx | T1 | wt/del | 4.5/7 | F | Z/Z* | ||
| Anterior tongue | T1 | wt/del | 7 | F | Z/Z* | ||
| Submandibular gland | T1 | wt/del | 4.5/7 | F | Z/Z* | ||
| Peripheral blood | T1 | wt/del | 5/7 | — | Z | ||
| VC 6 | M/68 | Mediastinal lymph node | T1/T2 | wt/del | 4/5 | F | Z/Z* |
| Nasopharynx | T1/T2 | wt/del | 4/5 | F | Z/Z* | ||
| Larynx | T1/T2 | wt/del | 4/5 | F | Z/Z* | ||
| Anterior tongue | nd | nd | nd | nd | nd | ||
| Submandibular gland | T1/T2 | wt/del | 4/5 | F | Z/Z* | ||
| Peripheral blood | T1 | wt/del | 4/5 | F | Z/Z* | ||
| VC 7 | F/83 | Mediastinal lymph node | T1 | del | 7 | F | Z/Z* |
| Nasopharynx | T1/T2 | wt/del | 4.5/7 | F | Z/Z* | ||
| Larynx | T1 | wt/del | 4.5/7 | F | Z/Z* | ||
| Anterior tongue | T2 | wt/del | 7 | F | — | ||
| Submandibular gland | T2 | wt/del | 5/7 | F | Z/Z* | ||
| Peripheral blood | T1/T2 | wt/del | 5/7 | F | Z/Z* | ||
| VC 8 | M/57 | Cervical lymph node | T1 | wt/del | 4/4.5 | F | nd |
| Mediastinal lymph node | T1 | del | 4/4.5 | F | nd | ||
| Para-aortic lymph node | T1 | wt/del | — | F | nd | ||
| Nasopharynx | T1 | del | 4 | F | nd | ||
| Thyroid | T1 | wt/del | 4.5 | — | nd | ||
| Tonsil (palatine) | T1 | wt/del | 4/4.5 | F | nd | ||
| Submandibular gland | T1 | wt/del | 4.5 | — | nd | ||
| Spleen | T1 | wt/del | 4.5 | — | nd | ||
| Thymus | T1 | wt/del | — | — | nd | ||
| VC 9 | F/70 | Cervical lymph node | T1 | wt | 4.5 | F | nd |
| Mediastinal lymph node | T1 | wt | 4.5 | F | nd | ||
| Para-aortic lymph node | — | wt | — | F | nd | ||
| Nasopharynx | T1 | wt | 4.5 | F/f | nd | ||
| Thyroid | — | wt | 4.5 | — | nd | ||
| Tonsil (palatine) | T1 | wt | 4.5 | F | nd | ||
| Submandibular gland | — | wt | 4.5 | — | nd | ||
| Spleen | — | wt | 4.5 | — | nd | ||
| VC 10 | F/26 | Cervical lymph node | T1 | — | 4.5/5 | F/f | nd |
| Mediastinal lymph node | — | — | 4.5 | F/f | nd | ||
| Para-aortic lymph node | T1 | — | 4.5 | — | nd | ||
| Nasopharynx | T1 | — | 4.5/5 | F/f | nd | ||
| Thyroid | T1 | — | 4.5 | — | nd | ||
| Tonsil (palatine) | T1 | wt/del | 4.5/5 | F/f | nd | ||
| Tonsil (lingual) | T1 | wt/del | 4.5 | — | nd | ||
| Lung (central) | T1/T2 | del | 4.5 | — | nd | ||
| Lung (peripheral) | T1 | del | 4.5 | — | nd | ||
| Spleen | T1 | — | 4.5 | — | nd | ||
| Thymus | T1 | — | 4.5 | — | nd | ||
| VC 11 | M/40 | Cervical lymph node | T1 | wt/del | — | — | nd |
| Nasopharynx | T1/T2 | wt/del | 4.5 | F/f | nd | ||
| Larynx | T1 | wt | 4.5/5/6 | — | nd | ||
| Oropharynx | T1 | — | 4.5 | — | nd | ||
| Tonsil | T1 | wt | 4.5 | — | nd | ||
| Parotid gland | — | wt/del | — | F | nd | ||
| Submandibular gland | T1 | del | 4/4.5/5/6 | F | nd | ||
| Penis | T1 | wt | 4.5/5/6 | — | nd | ||
| VC 12 | M/33 | Cervical lymph node | — | wt/del | — | — | nd |
| Nasopharynx | T1 | wt/del | 4.5/5 | F | nd | ||
| Larynx | — | del | — | — | nd | ||
| Oropharynx | — | wt/del | — | — | nd | ||
| Tonsil | — | del | 4.5 | F/f | nd | ||
| Parotid gland | T1 | del | 4.5 | — | nd | ||
| Submandibular gland | T1 | del | 4.5 | — | nd | ||
| Penis | — | del | — | F/f | nd | ||
| VC 13 | M/69 | Cervical lymph node | T1 | wt/del | 4.5 | F/f | nd |
| Nasopharynx | T1 | del | 4/4.5/5/6 | F/f | nd | ||
| Larynx | — | wt/del | — | — | nd | ||
| Oropharynx | — | wt/del | — | — | nd | ||
| Tonsil | T1 | wt/del | 4.5 | F/f | nd | ||
| Parotid gland | T1/T2 | wt/del | 4.5 | F | nd | ||
| Submandibular gland | T1 | wt/del | 4.5 | — | nd | ||
| Penis | T1 | wt/del | 4.5 | — | nd | ||
| VC 14 | M/88 | Cervical lymph node | T1/T2 | del | 4.5/5/6 | F | nd |
| Mediastinal lymph node | T1 | del | 5/6 | F | nd | ||
| Para-aortic lymph node | T1 | del | 5/6 | F | nd | ||
| Thyroid | T1 | del | 4.5 | F | nd | ||
| Lung (peripheral) | T1 | del | 4/4.5/6 | F | nd | ||
| Lung (central) | T1 | del | 4/4.5/6 | F | nd | ||
| Tonsil (palatine) | — | wt/del | 4.5 | — | nd | ||
| Tonsil (lingual) | T1 | del | 4.5/5/6/7 | F/f | nd | ||
| Submandibular gland | — | — | 4.5/6 | — | nd | ||
| Spleen | — | del | 4.5 | F | nd | ||
| VC 15 | F/67 | Cervical lymph node | T1 | del | 4.5/6 | F | nd |
| Nasopharynx | T1 | wt/del | 4.5 | — | nd | ||
| Larynx | T1 | — | — | F/f | nd | ||
| Oropharynx | — | del | — | — | nd | ||
| Tonsil | T1/T2 | del | 4.5/6 | F | nd | ||
| Parotid gland | T1 | — | 4.5 | — | nd | ||
| Submandibular gland | T1 | — | 4.5 | — | nd | ||
| Cervix | T1 | — | 4.5/6 | F | nd |
Peripheral blood was available from VC1-7. Some specific PCR bands are not shown in the figure but were detected in blots of longer exposure, which accounts for the discrepancies between the data summarized in the table and those shown in the figure.
nd indicates PCR assays not performed or insufficient samples for analysis; —, not detected.
In this study, direct analysis of EBV genomes contained in clinical specimens provided more accurate information about coinfecting viral strains within normal carriers than previous in vitro isolation studies.1,2 The EBV genome analysis of a large number of tissues at multiple sites provided a more complete picture of the individual viral carrier status than that from previous studies that usually used the PBMCs or throat washings.5,6 Overall, the present study demonstrated a much higher rate of coinfection of multiple distinct EBV strains within normal carriers than previously thought and added to the increasing evidence for coinfection in the immunocompetent hosts.5-7 This infers that the EBV carrier status in immunocompromised HIV-infected persons3,4is not different from that in immunocompetent normal carriers; the multiplicity of infection in HIV-infected persons has merely been more readily detected, likely because of a higher viral load. It further implies that the immune response elicited by an existing EBV infection may not protect the host from infection with additional exogenous viral strains, either from the same or different types. Coinfection with different viral strains may enable EBV to generate diversity by genetic recombination. This phenomenon is observed in the HIV-associated oral hairy leukoplakia,13 14 in which viral variants arise through intrastrain and interstrain recombination of multiple EBV strains during exuberant productive replication.
Both deletion and wild-type LMP1 variants could be detected in 6 of 7 peripheral blood specimens indicating that both deletion and wild-type LMP1 variants can be transmitted and coresident in PBMCs. In addition, equal viral diversity was observed in both the epithelial and circulating B-cell (lymphoid and peripheral blood) compartments. Taken together, our data imply that the coinfecting EBV strains are capable of establishing long-term persistence in immunocompetent hosts. Because no discernible differences were observed in the EBV strains harbored in multiple epithelial tissues and in the B-cell pool, our data do not support the concept of epithelial-specific or lymphoid-specific viral variants in normal carriers.
An unexpectedly high level of coinfection of the deletion and wild-type LMP1 viral variants was observed within the normal carriers. Thus, mixed infection of deletion and wild types (14 of 15, 93%) or wild-type singly (1 of 15, 7%) was detected within the viral carriers. In contrast, the deletion-type LMP1 variant singly was predominant in nasal T/NK-cell lymphomas (21 of 23, 91%)7 of the same population (P < 0.001, Fischer's exact test). The marked discrepancy in distribution of deletion and wild-type LMP1 viral variants between normal and tumor tissues substantiates the hypothesis of preferential selection of deletion LMP1 variants in EBV-associated malignancies.7
Reprints:Gopesh Srivastava, Department of Pathology, University Pathology Building, Queen Mary Hospital Compound, Pok Fu Lam Rd, Hong Kong; e-mail: gopesh@pathology.hku.hk.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal