Abstract
STI571 induces sustained hematologic remission in patients with chronic myeloid leukemia (CML) in chronic phase. However, in advanced phases, especially blast crisis, the leukemia usually becomes resistant within months. It has been investigated whether resistance to STI571 is stable and immutable or whether it can be reversed in selected CML cell lines. Withdrawal of STI571 for varying lengths of time from cultures of 3 resistant lines (K562-r, KCL22-r, and Baf/BCR-ABL–r1) did not restore sensitivity to the inhibitor. In contrast, LAMA84-resistant cells experienced a sharp reduction in survival and proliferation during the first week of STI571 withdrawal but recovered thereafter. Moreover, when left off the inhibitor for 2 months or longer, this cell line reacquired sensitivity to STI571. It is hypothesized, therefore, that patients who have become resistant to the drug may respond again if STI571 therapy is temporarily interrupted.
Introduction
Chronic myeloid leukemia (CML) results from the oncogenic transformation of hematopoietic stem cells by theBCR-ABL fusion gene generated by the t(9;22)(q34;q11) translocation that produces the Philadelphia chromosome. The disease usually evolves in 3 stages, starting in a relatively “benign” chronic phase and progressing through an accelerated phase to an ultimately fatal blast crisis. Conventional treatment includes allogeneic stem cell transplantation, hydroxyurea, interferon-α, and cytosine arabinoside.1 Presently, an inhibitor of the deregulated Bcr-Abl tyrosine kinase named STI571 is being tested in clinical trials for CML. Preliminary results for patients treated in chronic phase are very encouraging.2 When given at accelerated phase or blast crisis, STI571 can induce frequent hematologic responses, but these are nearly always followed by relapse,3 suggesting development of de novo resistance to the drug or selection of a resistant clone.
We recently generated a series of STI571-sensitive and -resistant clones from BCR-ABL–positive cell lines in order to model the phenomenon of acquired resistance to this inhibitor.4In some of these lines the mechanism of resistance was attributable toBCR-ABL amplification and overexpression, multidrug resistance gene (MDR1) overexpression, or ineffective inhibition of Bcr-Abl tyrosine phosphorylation. An outstanding question from that study was the fate of resistant cell lines upon STI571 withdrawal. This is obviously an important question in the analogous context of STI571-resistant patients who are temporarily taken off therapy. We show here that whereas the resistance of some cell lines is unaltered even after various months in culture without STI571, in other lines the molecular mechanism of resistance is reversed and sensitivity to STI571 is restored.
Study design
The STI571-sensitive (s) and -resistant (r) cell lines Baf/BCR-ABL–s, Baf/BCR-ABL–r1, K562-s, K562-r, KCL22-s, KCL22-r, LAMA84-s, and LAMA84-r have been described previously.4 Baf/BCR-ABL was derived from the Ba/F3 murine hemopoietic line, whereas K562, KCL22, and LAMA84 were established from patients with CML in blast crisis.5 The sensitive lines were grown in RPMI 1640 supplemented with penicillin, streptomycin, l-glutamine, and 10% fetal calf serum (complete medium referred to as RF-10) and subcultured every 2 to 3 days as indicated by acidification of the supernatant. The resistant counterparts were routinely kept in RF-10 supplemented with 1 μM STI571 unless stated otherwise.
For each experiment, exponentially growing cells were centrifuged, washed 3 times in phosphate-buffered saline without Ca++ and Mg2+, and resuspended at 2 × 105/mL in media with or without 1 μM STI571. After variable time periods, resistant cells cultured in the absence of STI571 were reexposed to 1μM of the inhibitor. Throughout the experiment, 5 mL aliquots were harvested daily or at longer intervals for (1) cell counts on a hemocytometer, (2) assessment of viability by trypan blue exclusion on duplicate aliquots, and (3) analysis of proliferation by the MTS assay performed in quadruplicate wells according to the manufacturer's instructions (CellTiter 96 AQueous One Solution Cell Proliferation Assay, Promega, Southampton, United Kingdom). Each complete experiment was repeated 2 or 3 times.
The number of BCR-ABL gene copies was investigated by fluorescence in situ hybridization as previously reported.6 Analysis of Bcr-Abl protein expression was done by Western blotting as previously described4 and by intracytoplasmic staining with an anti-Abl monoclonal antibody (24-11; Santa Cruz Biotechnology, Santa Cruz, CA) using a fluorescein-conjugated goat antimouse immunoglobulin G (Becton Dickinson, Basingstoke, United Kingdom) as secondary reagent and reading on a FACScan flow cytometer (Becton Dickinson) as described elsewhere.7 Total phosphotyrosine content was assessed by Western blotting4 using an anti-pY monoclonal antibody (PY-99; Santa Cruz Biotechnology). Apoptosis was assessed by measuring the level of caspase-3 as previously reported.4
Results and discussion
The 4 STI571-resistant cell lines used in this study had been growing continuously in 1 μM STI571 for longer than 1 year, with a baseline viability of 80% to 98%. When K562-r and KCL22-r were washed free of STI571 and grown in RF-10 only for short (7-15 days) or longer (4-6 months) periods, no change in their behavior was observed. Moreover, reexposure of the 2 lines to STI571 after various periods of withdrawal did not result in significant cell death or reduction in proliferation as compared with resistant cells grown continuously with the inhibitor (data not shown). This was entirely expected for KCL22-r, because the parental KCL22 is itself exceptionally resistant to STI571.4,6 Neither cell line overexpressesBCR-ABL, and K562-r but not KCL22-r was shown to require larger concentrations of STI571 to inhibit the same proportion of Bcr-Abl autophosphorylation as its sensitive counterpart.4Although the exact mechanism of resistance in both lines is still unknown, it appears to be stable in the absence of STI571.
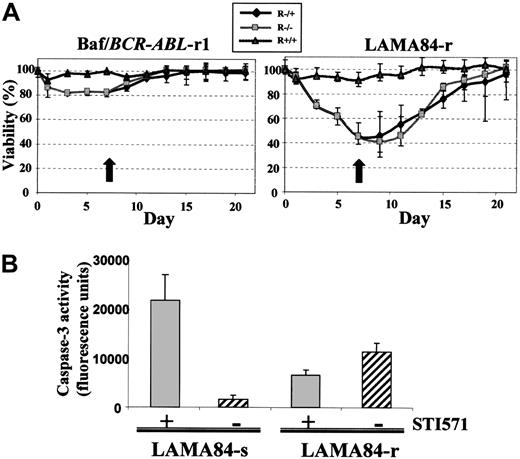
In the case of the Baf/BCR-ABL–r1 line, a 7-day withdrawal of STI571 led to a small but reproducible drop in viability and cell proliferation. The effect peaked around days 4 to 8 of withdrawal, after which the cultures began to recover with or without reexposure to the compound (Figure 1A). Likewise, resistant cells kept in the absence of STI571 for 14, 28, 35, or 125 days showed no restoration of sensitivity upon reinitiation of treatment with the inhibitor (not shown).
The effect of STI571 withdrawal.
(A) Viability of Baf/BCR-ABL–r1 and LAMA84-r cells upon withdrawal of STI571 from the culture. On day 0, exponentially growing cells were washed off the compound and replated in RF-10 media (R−/−), whereas control cells were maintained in media supplemented with 1 μM STI571 (R+/+). Subculturing with the respective media was done whenever necessary for each cell line. On day 7 (indicated by the black arrow), one half of the RF-10 culture was reexposed to 1 μM STI571 (R−/+) and the 3 cultures were observed for 1 additional week. Results are shown as the mean and range percentage of trypan blue–negative cells out of 200 cell counts from duplicate culture aliquots, in 1 of 3 representative experiments. (B) Caspase-3 activity in LAMA84-s and LAMA84-r cells after 3 days in culture with (+) and without (−) 1 μM STI571. Results represent the mean ± SD fluorescent units of quadruplicate cultures.
The effect of STI571 withdrawal.
(A) Viability of Baf/BCR-ABL–r1 and LAMA84-r cells upon withdrawal of STI571 from the culture. On day 0, exponentially growing cells were washed off the compound and replated in RF-10 media (R−/−), whereas control cells were maintained in media supplemented with 1 μM STI571 (R+/+). Subculturing with the respective media was done whenever necessary for each cell line. On day 7 (indicated by the black arrow), one half of the RF-10 culture was reexposed to 1 μM STI571 (R−/+) and the 3 cultures were observed for 1 additional week. Results are shown as the mean and range percentage of trypan blue–negative cells out of 200 cell counts from duplicate culture aliquots, in 1 of 3 representative experiments. (B) Caspase-3 activity in LAMA84-s and LAMA84-r cells after 3 days in culture with (+) and without (−) 1 μM STI571. Results represent the mean ± SD fluorescent units of quadruplicate cultures.
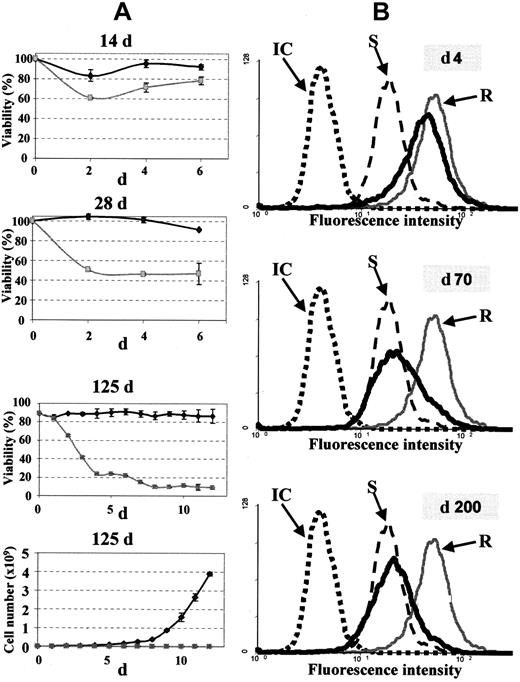
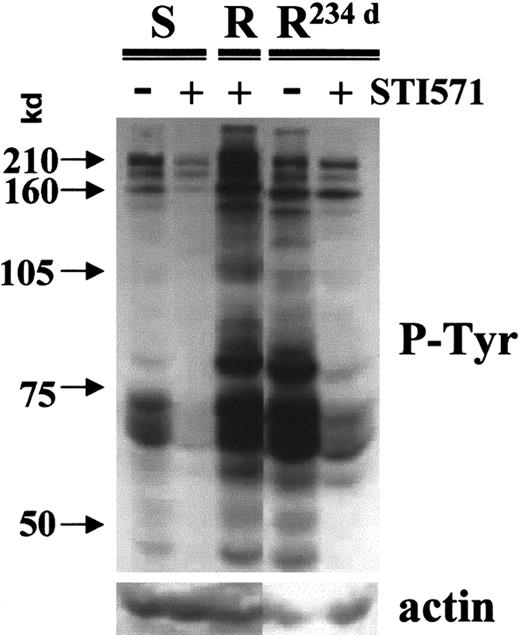
The profile of LAMA84-r cells was markedly different from the other lines. When washed thoroughly and replated in media without STI571, LAMA84-r cells showed a significant loss of viability and reduction in proliferation, starting around day 3 and peaking at days 5 to 9. Similarly to Baf/BCR-ABL–r1, these cells also recovered from the short (< 15 days) withdrawal interval and, with some additional delay (average 15 days vs 10 days for Baf/BCR-ABL-r1), returned to the viability and proliferation pattern exhibited when kept continuously in the presence of STI571 (Figure 1A). Nevertheless, when LAMA84-r cells were grown in RF-10 without the inhibitor for 2 weeks, a slight increase in cell death was observed upon reexposure to STI571. This effect was further accentuated if the period of withdrawal was extended to 4 weeks, and it culminated in a nearly complete restoration of sensitivity after 4 months without STI571 (Figure 2A). As expected, these cells became again prone to inhibition of Bcr-Abl autophosphorylation and tyrosine kinase activity by STI571, similarly to the original LAMA84-s cells and unlike the LAMA84-r clone kept continuously in STI571 (Figure 3).
Restoration of sensitivity to STI571.
(A) Viability (3 upper panels) and proliferation (bottom panel) of LAMA84-r cells in the presence (gray line) or absence (black line) of 1 μM STI571 after the indicated periods of withdrawal of the drug. Results are shown as the mean and range percentage of viable cells or absolute number of cells, respectively. (B) Flow cytometric histograms of LAMA84-s (S), LAMA84-r cells grown continuously in STI571 (R), and LAMA84-r grown in the absence of STI571 for the indicated periods (thick dark line) and stained with an anti-Abl antibody. One representative histogram of the 3 cell populations stained with an isotype control (IC) is shown. Note that the anti-Abl staining is due entirely to the Bcr-Abl protein, because LAMA84 does not express the normal ABL gene (no normal chromosome 9).8
Restoration of sensitivity to STI571.
(A) Viability (3 upper panels) and proliferation (bottom panel) of LAMA84-r cells in the presence (gray line) or absence (black line) of 1 μM STI571 after the indicated periods of withdrawal of the drug. Results are shown as the mean and range percentage of viable cells or absolute number of cells, respectively. (B) Flow cytometric histograms of LAMA84-s (S), LAMA84-r cells grown continuously in STI571 (R), and LAMA84-r grown in the absence of STI571 for the indicated periods (thick dark line) and stained with an anti-Abl antibody. One representative histogram of the 3 cell populations stained with an isotype control (IC) is shown. Note that the anti-Abl staining is due entirely to the Bcr-Abl protein, because LAMA84 does not express the normal ABL gene (no normal chromosome 9).8
Restoration of sensitivity to STI571.
Phosphotyrosine (p-Tyr) immunoblot of LAMA84-s (S), LAMA84-r (R), and resistant cells grown in the absence of STI571 for 234 days (R234d) exposed to 1 μ μM STI571 for 2 hours, as compared with nonexposed aliquots. Densitometric analysis of the p210 Bcr-Abl band corrected for the actin control showed a 2.1-fold decrease in phosphorylation of LAMA84-s and a 3.0-fold for the LAMA84-R234d line upon treatment with STI571. As previously shown,4 LAMA84-r cells kept continuously in the presence of STI571 have an elevated phosphotyrosine content.
Restoration of sensitivity to STI571.
Phosphotyrosine (p-Tyr) immunoblot of LAMA84-s (S), LAMA84-r (R), and resistant cells grown in the absence of STI571 for 234 days (R234d) exposed to 1 μ μM STI571 for 2 hours, as compared with nonexposed aliquots. Densitometric analysis of the p210 Bcr-Abl band corrected for the actin control showed a 2.1-fold decrease in phosphorylation of LAMA84-s and a 3.0-fold for the LAMA84-R234d line upon treatment with STI571. As previously shown,4 LAMA84-r cells kept continuously in the presence of STI571 have an elevated phosphotyrosine content.
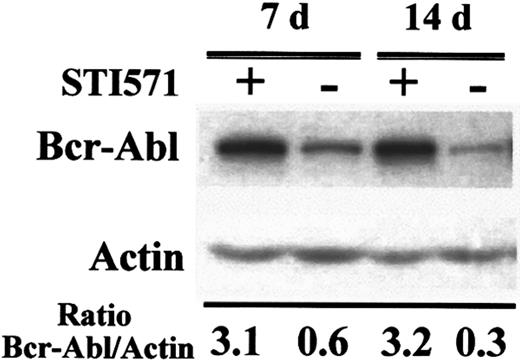
Because BCR-ABL gene amplification and overexpression were shown to underlie the STI571 resistance in both Baf/BCR-ABL–r and LAMA84-r, we investigated these phenomena in culture aliquots harvested at the various withdrawal time points. No reduction in Bcr-Abl overexpression was observed in Baf/BCR-ABL–r grown for up to 3 months in the absence of the inhibitor, in agreement with the fact that these cells retain their resistant phenotype under these conditions. In contrast, LAMA84-r cells experienced a progressive decrease in the level of Bcr-Abl protein with time after STI571 withdrawal (Figures 2B and4): The reduction was already noticeable at 4 days and became prominent at around 2 months. By 4 to 6 months, virtually all the cells from the original LAMA84-r culture had the same level of Bcr-Abl expression as the parental LAMA84-s line, coinciding with restoration of sensitivity to STI571. Fluorescence in situ hybridization analysis of these cells confirmed that the average number of BCR-ABL gene copies per cell was similar to that of LAMA84-s cells and approximately 5-fold lower than the number in LAMA84-r kept continuously in the presence of STI571 (not shown).
Reduction in Bcr-Abl protein expression upon withdrawal of STI571 from LAMA84-r cultures.
Total cellular protein was harvested from parallel cultures growing in the presence or absence of 1 μM STI571 for the periods indicated and subjected to Western analysis with anti-Abl (Bcr-Abl band shown) and antiactin antibodies. Densitometric analysis of the Bcr-Abl signal relative to that of actin is presented for each lane.
Reduction in Bcr-Abl protein expression upon withdrawal of STI571 from LAMA84-r cultures.
Total cellular protein was harvested from parallel cultures growing in the presence or absence of 1 μM STI571 for the periods indicated and subjected to Western analysis with anti-Abl (Bcr-Abl band shown) and antiactin antibodies. Densitometric analysis of the Bcr-Abl signal relative to that of actin is presented for each lane.
Our study reveals 2 interesting points. First, both resistant cell lines that overexpress BCR-ABL experience “withdrawal symptoms” when abruptly deprived of STI571. This surprising result suggests that the “acute” accumulation of a vast excess of kinase-active Bcr-Abl protein is in fact deleterious to cell viability and growth and may have a proapoptotic effect, as illustrated by the increase in caspase-3 activity in LAMA84-r cells after 3 days in the absence of STI571 (Figure 1B). Certainly, withdrawal of STI571 from LAMA84-r leads to a rapid and marked increase in Bcr-Abl autophosphorylation and total phosphotyrosine content (Figure5). This phenomenon may be analogous to the recent demonstration by Vigneri and Wang9 that forced nuclear entrapment of Bcr-Abl by treatment with STI571 and leptomycin-B followed by sudden withdrawal of the kinase inhibitor leads to apoptosis. We are presently investigating whether the “surplus” Bcr-Abl protein in the STI571-resistant lines has an altered cellular localization that could account for the early response of these lines to STI571 withdrawal. In any case, the effect in both Baf/BCR-ABL–r1 and LAMA84-r is transient, suggesting that the postulated imbalance of Bcr-Abl accumulation and localization may be rapidly “normalized” to allow survival in the absence of the inhibitor.
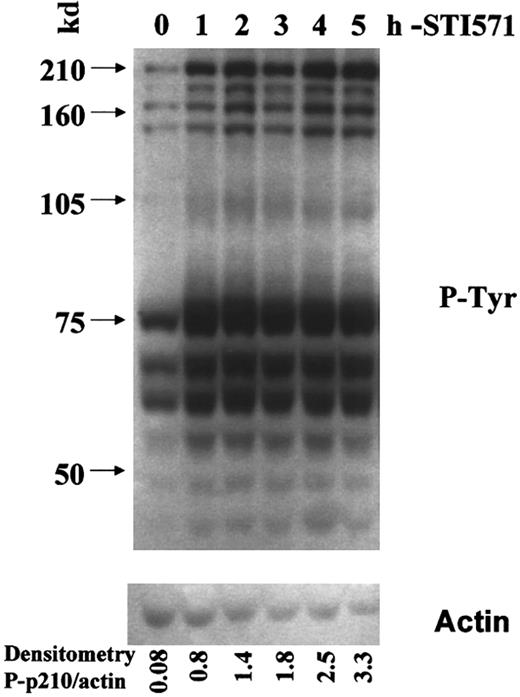
Increased phosphotyrosine content on withdrawal of STI571 from LAMA84-r cells.
Total cellular protein was harvested from cells grown continuously in the presence of 1 μM STI571 (time zero) and then hourly after thorough washing and reculture in media without STI571. The Western blot membrane was probed with an antiphosphotyrosine antibody (upper panel) and reprobed with an antiactin antisera (lower panel). The densitometric ratio of the phospho-Bcr-Abl (p-p210)/actin bands is shown for each time point and demonstrates a 41-fold increase in Bcr-Abl autophosphorylation after 5 hours of STI571 withdrawal.
Increased phosphotyrosine content on withdrawal of STI571 from LAMA84-r cells.
Total cellular protein was harvested from cells grown continuously in the presence of 1 μM STI571 (time zero) and then hourly after thorough washing and reculture in media without STI571. The Western blot membrane was probed with an antiphosphotyrosine antibody (upper panel) and reprobed with an antiactin antisera (lower panel). The densitometric ratio of the phospho-Bcr-Abl (p-p210)/actin bands is shown for each time point and demonstrates a 41-fold increase in Bcr-Abl autophosphorylation after 5 hours of STI571 withdrawal.
The second noteworthy result was the nearly complete restoration of sensitivity to STI571 in LAMA84-r cells maintained long-term off the drug. This clearly correlated with a loss of Bcr-Abl overexpression, probably due to absence of selection pressure for highBCR-ABL copy number and/or positive selection for lower expression. In Baf/BCR-ABL–r1 none of these phenotypic changes were observed, which may be attributed to the fact that this is not a true CML but, rather, a murine cell line whose transfectedBCR-ABL gene is under the control of an exogenous promoter that may allow cells with the amplified copies to be more stable in the absence of selective pressure.
Similarly to the situation in some cell lines, BCR-ABLamplification and overexpression have now been documented as a cause of acquired STI571 resistance in patients treated with this drug.10,11 In fact, in one patient recently described by Gorre et al10 in whom resistance to STI571 therapy was associated with BCR-ABL gene amplification, this phenomenon was no longer detectable 4 weeks after STI571 was discontinued and the patient was placed under alternative treatment for her leukemia. We conclude that, if the results from the present study are equally applicable to primary CML cells, it is possible that selected patients who become refractory to STI571 may benefit from a second course of therapy after an interval off this inhibitor.
We are grateful to Dr Elisabeth Buchdunger (Novartis Pharma, Basel, Switzerland) for the generous gift of STI571.
Supported by grants from the Leukaemia Research Fund, United Kingdom (A.J.T., J.M.G., J.V.M.), and the Association pour la Recherche sur le Cancer and Fondation de la Recherche Medicale, France (F.X.M., V.L.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Junia V. Melo, Dept of Haematology—ICSM, Hammersmith Hospital, Ducane Rd, London W12 0NN, United Kingdom; e-mail: j.melo@ic.ac.uk.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal