Abstract
Ifosfamide, a clinically potent chemotherapeutic agent, causes the depletion of intracellular glutathione (GSH) levels in various cell types. GSH is the major intracellular reductant against oxidative stress. 4-Hydroxyifosfamide (4-OH-IF), the activated form of ifosfamide, depletes GSH levels in T cells and natural killer (NK) cells; this is accompanied by a decrease in T-cell and NK-cell function. Here we demonstrate for the first time that human monocyte-derived dendritic cells (DCs) express higher constitutive levels of GSH and are less sensitive to 4-OH-IF-induced GSH depletion than T cells and NK cells. Treatment of DCs with 4-OH-IF significantly reduced their ability to stimulate allogeneic T-cell proliferation and interferon-γ (IFN-γ) production. Ifosfamide also decreased DC interleukin-12p70 (IL-12p70) production after stimulation with lipopolysaccharide (LPS) and IFN-γ. The decrease in allostimulatory capacity and in IFN-γ and IL-12 production correlated with a decrease in intracellular GSH in the DCs. The responses could be restored by reconstituting DC GSH levels with glutathione monoethyl ester (GSH-OEt). 4-OH-IF had no inhibitory effect on the ability of DCs to present exogenously added tyrosinase peptide to tyrosinase-specific cytotoxic T lymphocytes (CTLs). These studies suggest that in cancer patients treated with ifosfamide, protection strategies based on glutathione reconstitution may enhance DC function. (Blood. 2003;102: 3668-3674)
Introduction
Ifosfamide, which is a commonly used antineoplastic agent in the treatment of malignancies such as lymphomas, breast cancer, and sarcomas1-3 has been shown to reduce glutathione (GSH) levels in various cell types.4,5 Previously, we demonstrated that ifosfamide-induced GSH depletion in T cells and natural killer (NK) cells was accompanied by a corresponding decrease in T-cell function and NK-cell cytotoxicity.6,7
In vivo ifosfamide is metabolically activated by hepatic mixed-function oxidases into 4-hydroxyifosfamide (4-OH-IF). In our studies we used the prodrug 4-hydroperoxyifosfamide (4-OOH-IF), which in aqueous solution spontaneously gives rise to pharmacologically equivalent amounts of 4-OH-IF, the activated form of ifosfamide.8
GSH is a tripeptide consisting of glutamate, cysteine, and glycine, and it takes part in many metabolic and cell-cycle-dependent functions such as detoxification of free radicals and exogenous toxins, protein synthesis, transport, and maintenance of intracellular redox balance.9 In addition to housekeeping properties, GSH influences lymphocyte proliferation,10-12 polymorphonuclear cell function,13 and chemokine and cytokine production by different cell types.14-16
Antigen-presenting cells (APCs) derived from murine spleen have been shown to direct T-cell responses toward a TH1- or TH2-type response, depending on the level of intracellular glutathione. TH2 responses occur when glutathione levels are low.17 Suppression of tumor cell growth is favored by a TH1 response in which cytokines such as interferon-γ (IFN-γ) and interleukin-12 (IL-12) play important roles.18,19 Dendritic cells (DCs) are the most potent APCs in the body, and their unique ability to stimulate a primary T-cell response places them at the center of an immune response toward tumors.20,21 Immature DCs specialize in capturing and processing antigens, whereas mature DCs present antigenic peptides to T cells.22 We have therefore made a comparison of the effect of 4-OH-IF on GSH levels in immature and mature DCs and monocytes with GSH levels in T cells and NK cells. In addition, we studied the effect of 4-OH-IF-induced GSH depletion on DC functional properties. We found that when comparing cells from the same donors, DCs had higher constitutive levels of GSH than T cells and NK cells and were less sensitive to GSH depletion by 4-OH-IF. Treatment of DCs with 4-OH-IF or L-buthionine-sulfoximine (BSO) (which inhibits GSH biosynthesis by blocking γ-glutamyl-cysteine synthetase) reduced the ability of immature DCs to stimulate an allogeneic response but had no effect on the ability of mature DCs to present exogenously added tyrosinase peptide to tyrosinase-specific cytotoxic T lymphocytes (CTLs). IFN-γ production was also reduced in allogeneic cultures containing 4-OH-IF-treated DCs. 4-OH-IF also impaired the ability of DCs to produce IL-12p70 after lipopolysaccharide (LPS) and IFN-γ stimulation. The allostimulatory capacity of DCs and the cytokine production by peripheral blood leukocytes (PBLs) (IFN-γ) or DCs (IL-12p70) were found to be regulated by DC intracellular GSH levels because the treatment of DCs with GSH-OEt reconstituted GSH levels and their ability to stimulate T-cell proliferation and cytokine production.
Materials and methods
Cell isolation
Peripheral blood mononuclear cells (PBMCs) were isolated from heparinized venous blood from healthy volunteers by density gradient centrifugation over Ficoll-Hypaque (Pharmacia Biotech, Uppsala, Sweden). Monocytes, lymphocytes, and NK cells were isolated by the incubation of PBMCs with micromagnetic beads coated with antibodies to CD14, CD3, and CD56, respectively (Miltenyi Biotech, San Francisco, CA) followed by passage through a separating column in a strong magnetic field (MACS, Miltenyi Biotech). The purity of each cell population was determined by fluorescence-activated cell sorter (FACS) analysis and ranged from 90% to 95% for CD3+ cells, 85% to 95% for CD56+ cells, and 80% for CD14+ cells. The institutional review board of Ludwig-Maximillians-University approved these studies. Informed consent was provided according to the Declaration of Helsinki.
Generation of DCs
PBMCs were prepared as described and cultured at 5 × 106 in 2 mL medium per well in 6-well plates (Costar). After 2 hours the cells were gently agitated, and the nonadherent cells were removed. Adherent PBMCs were then cultured in the presence of granulocyte macrophage-colony-stimulating factor (GM-CSF) (800 U/mL) (Novartis, Nuremberg, Germany) and IL-4 (500 U/mL) (PromoCell, Heidelberg, Germany) for 8 days in RPMI VLE (Biochrom, Berlin, Germany) supplemented with 2 mM glutamine, 100 U/mL penicillin/streptomycin (all from Life Technologies, Karlsruhe, Germany), and 5% low endotoxin fetal calf serum (FCS; BioWhittaker, Verviers, Belgium). GM-CSF and IL-4 were added again on day 4 of culture. Mature DCs were obtained by adding tumor necrosis factor-α (TNF-α) (800 U/mL) (Biomol, Hamburg, Germany) from days 6 to 8 of culture. Immature DCs were 85% to 95% CD1a+, and mature DCs were 80% to 95% CD83+, as determined by FACS analysis.
4-OH-IF and BSO treatment of NK cells, T cells, monocytes, immature DCs, and mature DCs
The prodrug 4-OOH-IF (kindly provided by Baxter Medical, Munich, Germany) rapidly gives rise to equivalent amounts of 4-OH-IF after dissolution in phosphate-buffered saline (PBS), pH 7.4. NK cells, T cells, monocytes, immature DCs, and mature DCs (0.5 × 106 cells/mL) were treated with 0, 50, 100, or 200 μM 4-OH-IF at 37°C for 90 minutes or with 0.5 mM to 5 mM BSO at 37°C for 24 hours. Untreated cells were used as controls. 4-OH-IF- or BSO-treated cells were given no further treatment or were washed and incubated with GSH monoethyl-glycyl-ester (GSH-OEt) (Bachem, Heidelberg, Germany) at a final concentration of 0.4 mM for 5 hours after 4-OH-IF treatment or with GSH-OEt at a final concentration of 5 mM for 5 hours after BSO treatment. Cells were harvested, and GSH levels were measured using high-performance liquid chromatography (HPLC).
Determination of intracellular GSH levels
Total soluble intracellular GSH (reduced or oxidized form) from T cells, NK cells, monocytes, and immature or mature DCs—treated with 4-OH-IF or BSO or left untreated—was quantitated using a modified HPLC method,23 as previously described.24 The cell pellet was treated with 1 N perchloric acid, and γ-glutamyl glutamate was added as an internal standard. After derivatization of the free thiol groups with iodoacetic acid and the amino groups with 1-fluoro-2,4-dinitrobenzene, the reaction mixtures were separated by HPLC. Aliquots were injected onto a μ Bondapak amine column (4 × 250 mm; Waters, Eschborn, Germany) and were eluted with a sodium acetate gradient (flow rate, 2 mL/min) in a water/methanol/acetic acid solvent at pH 4.5. The dinitro-phenyl derivatives were detected at 360 nm. GSH was quantified in relation to the internal standard. Protein was determined according to the method of Lowry et al.25
FACS analysis
The antibodies used to assess the level of DC maturation included anti-CD1a, CD40, CD86, HLA-DR (PharMingen, Hamburg, Germany), CD14, and CD83 (Immunotech, Hamburg, Germany) and major histocompatibility complex (MHC) class 1 (W6/32).26 The isotype controls used included immunoglobulin G1 (IgG1), IgG2a, and IgG2b (Immunotech). Cells were washed in PBS containing 5% FCS. Staining was performed at 4°C for 30 minutes using mouse mAbs to the markers mentioned. The cells were then washed and incubated with phycoerythrin (PE)-conjugated goat antimouse IgG (DAKO, Hamburg, Germany) for 30 minutes at 4°C. Cells were washed once more and were resuspended in 400 μL PBS (Life Technologies) plus 5% FCS (Biochrom). All FACS analyses were performed on a FACScan (Becton Dickinson, Mountain View, CA) using standard Cell Quest software (Becton Dickinson).
Mixed-leukocyte reactions
DCs were cultured as described with either BSO (0.5 mM) added on day 7 for 24 hours or 4-OH-IF (100 μM) added on day 8 for 90 minutes. Untreated cells from parallel day-8 cultures were used as control cells. 4-OH-IF- or BSO-treated cells were given no further treatment or were washed and then incubated with GSH-OEt at a final concentration of 0.4 mM for 5 hours after 4-OH-IF treatment or with GSH-OEt at a final concentration or 5 mM for 5 hours after BSO treatment. DCs were irradiated, washed, and resuspended in RPMI medium plus 10% FCS and incubated with allogeneic PBMCs (105/well) in 96-well plates at different responder-to-stimulator ratios for 6 days. Control wells contained BSO-treated DCs alone, 4-OH-IF-treated DCs alone, untreated DCs alone, or PBLs alone. T-cell proliferation was assessed by measuring the uptake of [3H]-thymidine (1 μCi/well [0.037 MBq]) (Amersham, Pharmacia Biotech, Freiburg, Germany) during the last 24 hours of culture using a microBeta counter (Beckman, Germany).
DCs treated in parallel with 4-OH-IF or BSO plus or minus GSH-OEt were also added to allogeneic PBLs, and culture supernatants were collected after 6 days. Enzyme-linked immunosorbent assay (ELISA) kits specific for IFN-γ and IL-12p70 (Becton Dickinson, Heidelberg, Germany) were used to determine the levels of IFN-γ and IL-12p70 in the allogeneic culture supernatants after 6 days.
LPS and IFN-γ stimulation of IL-12p70 production
DCs generated as described were treated on day 8 with 4-OH-IF (100 μM) for 90 minutes. Some cells were additionally treated with GSH-OEt (0.4 mM) for 5 hours. Untreated cells were used as controls. Cells were plated at a final concentration of 5 × 104/well and were stimulated with 1 μg/mL LPS or 1 μg/mL LPS and 1 ng/mL IFN-γ for 24 to 48 hours, after which the supernatants were collected and IL-12p70 levels were determined using an IL-12p70-specific ELISA.
Antigen-specific T-cell stimulation
Monocytes were isolated from an HLA-A*0201-positive donor, and immature DCs were generated as described. To obtain mature DCs, TNF-α (800 U/mL) was added from days 6 to 8 of culture, BSO (0.5 mM) was added for 24 hours on day 7 of culture, and 4-OH-IF (100 μM) was added to the DCs for 90 minutes on day 8. Untreated cells from parallel day-8 cultures were used as controls. The cells were then harvested, washed, and resuspended at 1 × 104 DCs/well in 100 μL medium in 96-well, round-bottom plates (Nunc) and were pulsed with the tyrosinase peptide (aa 368-376; YMNGT-MSQV) (1-10 μg/mL) for 2 hours. The tyrosinase peptide was synthesized and purified by Dr M. Eulitz in our in-house facilities at the GSF Institute of Molecular Immunology (Munich, Germany). Tyrosinase-specific T cells (2 × 104) clone TyrF827 in 100 μL RPMI medium (Biochrom) containing 10% FCS and 100 U/mL IL-2 (Biomol) were then added to each well. Control wells contained non-tyrosinase-pulsed DCs and CTLs or DCs alone or CTLs alone. Supernatants (100 μL) were removed after 24 hours of culture. The amount of IFN-γ produced was determined using an IFN-γ-specific ELISA kit (Becton Dickinson, Heidelberg, Germany).
Apoptosis detection
Immature DCs generated as described were treated with 4-OH-IF (100 μM) for 90 minutes and tested for viability immediately or 48 hours after 4-OH-IF treatment. DC viability was also tested after treatment with BSO (5 mM) for 24 hours. DCs (2-5 × 105) were incubated with 5 μL fluorescein isothiocyanate (FITC)-conjugated Annexin V in binding buffer (Bender MedSystems; Alexis Deutschland, Grünberg, Germany) for 10 minutes at room temperature. Cells were incubated with Annexin V alone or propidium iodide (PI) (1 μg/mL) was added to the Annexin-V-stained cells just before analysis by flow cytometry. Cells were also stained with PI alone.
Statistical analysis
Data are expressed as the mean ± SD of triplicate samples. Statistical significance of the differences was determined using the unpaired 2 tailed Student t test. Differences were considered statistically significant for P < .05.
Results
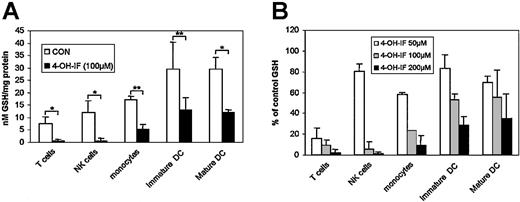
4-OH-IF significantly decreases intracellular GSH levels in T cells, NK cells, monocytes, immature DCs, and mature DCs
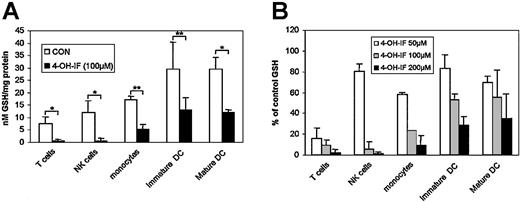
4-OH-IF significantly decreased intracellular GSH levels in T cells, NK cells, monocytes, immature DCs, and mature DC. When comparing cells from the same donors, T cells and NK cells had lower constitutive levels of GSH than DCs (Figure 1A).
Reduction in intracellular GSH levels by 4-OH-IF. (A) T cells, NK cells, monocytes, immature DCs, and mature DCs (0.5 × 106/mL) were treated with 4-OH-IF (100 μM) for 90 minutes. Untreated cells were used as controls. Cells were then washed, and GSH levels were measured by HPLC. Results are expressed as nM GSH/mg protein, and they represent the mean ± SD from 3 separate donors. *P < .05; **P < .01. (B) T cells, NK cells, monocytes, immature DCs, and mature DCs (0.5 × 106/mL) were treated with increasing concentrations (50, 100, 200 μM) of 4-OH-IF for 90 minutes. Untreated cells were used as controls. Cells were then washed, and GSH levels were measured by HPLC. Results are expressed as the percentage of control values and represent the mean ± SD of 2 separate experiments from 2 separate donors.
Reduction in intracellular GSH levels by 4-OH-IF. (A) T cells, NK cells, monocytes, immature DCs, and mature DCs (0.5 × 106/mL) were treated with 4-OH-IF (100 μM) for 90 minutes. Untreated cells were used as controls. Cells were then washed, and GSH levels were measured by HPLC. Results are expressed as nM GSH/mg protein, and they represent the mean ± SD from 3 separate donors. *P < .05; **P < .01. (B) T cells, NK cells, monocytes, immature DCs, and mature DCs (0.5 × 106/mL) were treated with increasing concentrations (50, 100, 200 μM) of 4-OH-IF for 90 minutes. Untreated cells were used as controls. Cells were then washed, and GSH levels were measured by HPLC. Results are expressed as the percentage of control values and represent the mean ± SD of 2 separate experiments from 2 separate donors.
After treatment with 4-OH-IF (100 μM) for 90 minutes, GSH was reduced to 10% and 5% of control values, respectively, for T cells and NK cells (Figure 1B, gray bars). Monocyte GSH was reduced to 25% of control values, and immature and mature DC GSH was reduced to approximately 50% of control values (Figure 1B).
When we compared the decrease in GSH level after treatment with varying concentrations of 4-OH-IF (range, 50-200 μM), we found that T cells were more sensitive to 4-OH-IF than NK cells because NK GSH levels were 80% of control values and T-cell GSH was 20% of control values after treatment with the lowest concentration (50 μM) of ifosfamide used (Figure 1B).
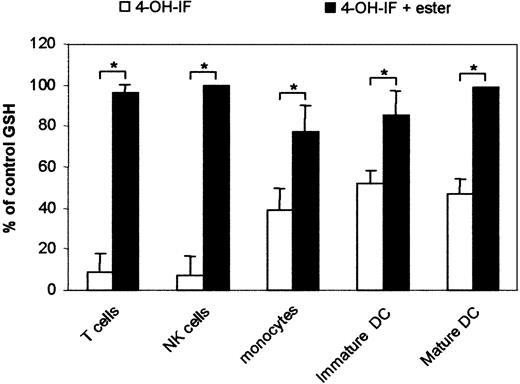
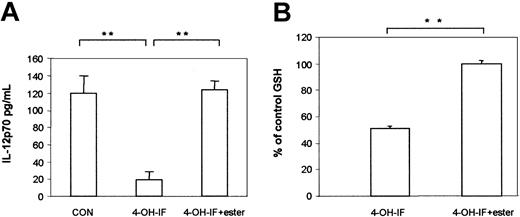
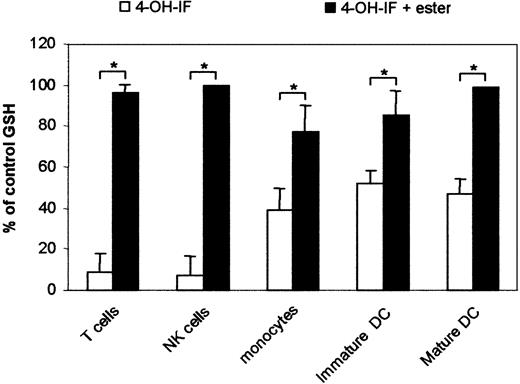
Reconstitution of cellular GSH levels by glutathione-monoethyl ester after 4-OH-IF treatment
GSH levels in T cells, NK cells, monocytes, and immature and mature DCs could be reconstituted after 4-OH-IF treatment by adding GSH-OEt to the cells for 5 hours (Figure 2). GSH alone is not efficiently transported into many cell types28 ; however, the monoethyl-(glycyl) ester of GSH is efficiently transported and intracellularly hydrolyzed to GSH.29,30 After the addition of GSH-OEt (0.4 mM) to 4-OH-IF-treated cells, GSH levels were reconstituted to 90% to 100% of control values (Figure 2).
Reconstitution of cellular GSH levels with GSH-OEt. T cells, NK cells, monocytes, immature DCs, and mature DCs (0.5 × 106/mL) were treated with 4-OH-IF (100 μM) for 90 minutes. GSH-OEt was added at a final concentration of 0.4 mM for 5 hours. Untreated cells were used as controls. Cells were then washed, and GSH levels were determined. Results are expressed as the percentage of control values and represent the mean ± SD from 3 separate experiments. *P < .05.
Reconstitution of cellular GSH levels with GSH-OEt. T cells, NK cells, monocytes, immature DCs, and mature DCs (0.5 × 106/mL) were treated with 4-OH-IF (100 μM) for 90 minutes. GSH-OEt was added at a final concentration of 0.4 mM for 5 hours. Untreated cells were used as controls. Cells were then washed, and GSH levels were determined. Results are expressed as the percentage of control values and represent the mean ± SD from 3 separate experiments. *P < .05.
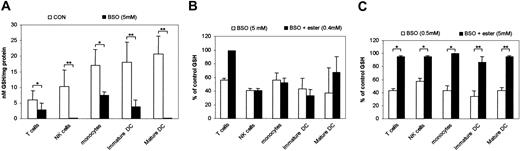
BSO significantly depletes GSH levels in T cells, NK cells, monocytes, and immature and mature DCs: effect of glutathione-monoethyl ester concentration on reconstitution
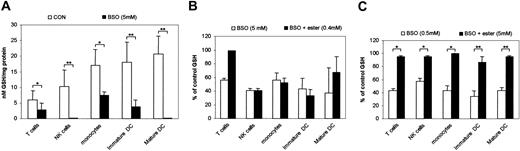
BSO, which inhibits GSH biosynthesis by inactivating γ-glutamyl-cysteine synthetase,28 significantly depleted GSH levels in T cells, NK cells, monocytes, and DCs (Figure 3A). However, with the exception of T cells, the decrease could not be overcome by the addition of GSH-OEt at the concentration used (0.4 mM) to restore GSH levels after 4-OH-IF treatment (Figure 3B). Lower concentrations of BSO (500 μM) also caused a significant reduction in GSH levels, from 35% to 60% of control values, which could be reconstituted to 90% to 100% of control values using higher concentrations of GSH-OEt (5 mM) (Figure 3C).
Effect of BSO on intracellular GSH levels. (A) T cells, NK cells, monocytes, immature DCs, and mature DCs (0.5 × 106/mL) were treated with BSO (5 mM) for 24 hours. Untreated cells were used as controls. Cells were then washed, and GSH levels were measured by HPLC. Results are expressed as nM GSH/mg protein and represent the mean ± SD from 3 separate experiments. *P < .05; **P < .01. (B) Cells were treated as in panel A, GSH-OEt was added at a final concentration of 0.4 mM for 5 hours, and GSH levels were measured by HPLC. Untreated cells were used as controls. Results are expressed as a percentage of control values and represent the mean ± SD from 3 separate experiments. (C) T cells, NK cells, monocytes, immature DCs, and mature DCs (0.5 × 106/mL) were treated with BSO (0.5 mM) for 24 hours. GSH-OEt was added at a final concentration of 5 mM for 5 hours. Cells were then washed, and GSH levels were determined. Untreated cells were used as controls. Results are expressed as the percentage of control values and represent the mean ± SD from 3 separate experiments. *P < .05; **P < .01.
Effect of BSO on intracellular GSH levels. (A) T cells, NK cells, monocytes, immature DCs, and mature DCs (0.5 × 106/mL) were treated with BSO (5 mM) for 24 hours. Untreated cells were used as controls. Cells were then washed, and GSH levels were measured by HPLC. Results are expressed as nM GSH/mg protein and represent the mean ± SD from 3 separate experiments. *P < .05; **P < .01. (B) Cells were treated as in panel A, GSH-OEt was added at a final concentration of 0.4 mM for 5 hours, and GSH levels were measured by HPLC. Untreated cells were used as controls. Results are expressed as a percentage of control values and represent the mean ± SD from 3 separate experiments. (C) T cells, NK cells, monocytes, immature DCs, and mature DCs (0.5 × 106/mL) were treated with BSO (0.5 mM) for 24 hours. GSH-OEt was added at a final concentration of 5 mM for 5 hours. Cells were then washed, and GSH levels were determined. Untreated cells were used as controls. Results are expressed as the percentage of control values and represent the mean ± SD from 3 separate experiments. *P < .05; **P < .01.
Effect of 4-OH-IF and BSO on DC viability
DCs were incubated with the maximum dose of BSO we used in our experiments—5 mM for 24 hours—and then viability was measured. DCs were also incubated with 4-OH-IF (100 μM) for 90 minutes. Viability was measured immediately or 48 hours after treatment. The effect on cell viability was assessed after staining the cells with annexin V, a marker of apoptotic cells, and PI, a marker of necrotic cells. We found that after treatment, DC viability did not differ from that of untreated control cells (Table 1).
4-OH-IF or BSO reduces the ability of DCs to stimulate allogeneic T cells and is restored by treatment of the DCs with GSH-OEt
Immature DCs treated with 4-OH-IF (100 μM) for 90 minutes or untreated control cells were added to allogeneic PBLs for 6 days, and the amount of cell proliferation was measured. Ifosfamide significantly (P < .05) decreased the ability of DCs to stimulate allogeneic T cells (Figure 4A). The reduction in DC allostimulatory capacity could be overcome by treating the DCs with GSH-OEt for 5 hours after 4-OH-IF treatment. DCs treated with BSO also showed a significant reduction in their capacity to stimulate allogeneic T cells, which could be restored by treatment with GSH-OEt (Figure 4B).
Reduction in DC allostimulatory capacity after 4-OH-IF and BSO treatment and restoration with GSH-OEt. (A) DCs were treated with 4-OH-IF (100 μM) alone for 90 minutes on day 8 or with 4-OH-IF for 90 minutes and then with GSH-OEt (0.4 mM) for 5 hours. Untreated cells from parallel day-8 cultures were used as controls. DCs were irradiated and incubated with PBLs (105/well) at different PBL/DC ratios for 6 days. Results are shown for the PBL/DC ratio of 32:1. *P < .05. (B) DCs were treated with BSO (0.5 mM) alone on day 7 for 24 hours or with BSO for 24 hours and then with GSH-OEt (5 mM) for 5 hours. DCs were irradiated and resuspended in RPMI medium plus 10% FCS and incubated with allogeneic PBLs (105/well) in 96-well plates at PBL/DC ratios ranging from 2:1 to 64:1 for 6 days. Results are shown for the PBL/DC ratio of 64:1. BSO-treated DCs alone, 4-OH-IF-treated DCs alone, untreated DCs alone, or PBLs alone were used as controls. The amount of [3H]-thymidine incorporated during the last 24 hours of culture was measured (A-B). Results are expressed as the mean ± SD of cpm values of triplicate cultures from 1 of 3 representative experiments. *P < .05. (C) 4-OH-IF and 4-OH-IF plus GSH-OEt-treated DCs and (D) BSO and BSO plus GSH-OEt-treated DCs were also washed, and GSH levels were measured by HPLC. Untreated cells were used as controls. Results are expressed as the percentage of control values and represent the mean ± SD from 3 treatments. *P < .05.
Reduction in DC allostimulatory capacity after 4-OH-IF and BSO treatment and restoration with GSH-OEt. (A) DCs were treated with 4-OH-IF (100 μM) alone for 90 minutes on day 8 or with 4-OH-IF for 90 minutes and then with GSH-OEt (0.4 mM) for 5 hours. Untreated cells from parallel day-8 cultures were used as controls. DCs were irradiated and incubated with PBLs (105/well) at different PBL/DC ratios for 6 days. Results are shown for the PBL/DC ratio of 32:1. *P < .05. (B) DCs were treated with BSO (0.5 mM) alone on day 7 for 24 hours or with BSO for 24 hours and then with GSH-OEt (5 mM) for 5 hours. DCs were irradiated and resuspended in RPMI medium plus 10% FCS and incubated with allogeneic PBLs (105/well) in 96-well plates at PBL/DC ratios ranging from 2:1 to 64:1 for 6 days. Results are shown for the PBL/DC ratio of 64:1. BSO-treated DCs alone, 4-OH-IF-treated DCs alone, untreated DCs alone, or PBLs alone were used as controls. The amount of [3H]-thymidine incorporated during the last 24 hours of culture was measured (A-B). Results are expressed as the mean ± SD of cpm values of triplicate cultures from 1 of 3 representative experiments. *P < .05. (C) 4-OH-IF and 4-OH-IF plus GSH-OEt-treated DCs and (D) BSO and BSO plus GSH-OEt-treated DCs were also washed, and GSH levels were measured by HPLC. Untreated cells were used as controls. Results are expressed as the percentage of control values and represent the mean ± SD from 3 treatments. *P < .05.
The changes in T-cell proliferation correlated with changes in DC GSH levels because treatment of DCs with 4-OH-IF or BSO decreased GSH levels (P < .05) to approximately 50% of control values. Further treatment with GSH-OEt reconstituted GSH levels to 90% and 95% of control values, respectively, after 4-OH-IF and BSO treatment (Figure 4C-D).
Effect of BSO and 4-OH-IF on HLA-DR, MHC class 1, CD86, CD40, and CD83 expression on DCs
We looked at the expression of MHC and costimulatory molecules in addition to CD83 expression on DCs after BSO or 4-OH-IF treatment to determine whether the reduction in DC allostimulatory capacity was caused by a decrease in the expression of these molecules. The expression of MHC class 1 and HLA-DR molecules, in addition to CD83 and CD86 expression, was not decreased after treatment. CD40 expression on DCs was decreased after 4-OH-IF but not BSO treatment; however, the decrease observed did not reach a significant level (Table 2).
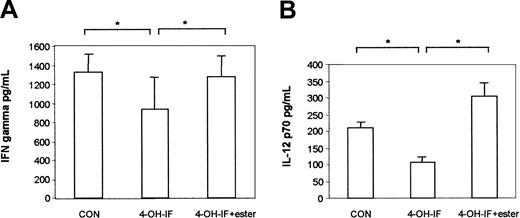
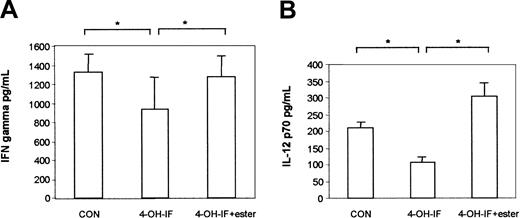
IFN-γ production in allogeneic cultures is reduced after treatment of DCs with 4-OH-IF
Supernatants were also collected from the cultures of allogeneic DCs and PBLs after 6 days. IFN-γ production was lower in cultures containing 4-OH-IF-treated DCs plus normal PBLs in comparison with untreated DCs plus normal PBLs (Figure 5A).
IFN-γ and IL-12p70 production are reduced in allogeneic cultures containing 4-OH-IF-treated DCs. DCs were treated with 4-OH-IF (100 μM) alone for 90 minutes on day 8 or with 4-OH-IF then GSH-OEt at a final concentration of 0.4 mM for 5 hours. Untreated cells were used as controls. DCs were washed and resuspended in RPMI medium plus 10% FCS and incubated with allogeneic PBLs (105/well) in 96-well plates at different PBL/DC ratios for 6 days. Results are shown for the PBL/DC ratio of 64:1. Additional controls included DC alone, 4-OH-IF-treated DCs alone, or PBLs alone. Cell culture supernatants were collected after 6 days, and (A) IFN-γ and (B) IL-12p70 levels were determined using ELISA specific for each cytokine. Results in panel A represent the mean of triplicate samples ± SD from 3 separate experiments. Results in panel B represent the mean of triplicate samples ± SD from 1 experiment. *P < .05.
IFN-γ and IL-12p70 production are reduced in allogeneic cultures containing 4-OH-IF-treated DCs. DCs were treated with 4-OH-IF (100 μM) alone for 90 minutes on day 8 or with 4-OH-IF then GSH-OEt at a final concentration of 0.4 mM for 5 hours. Untreated cells were used as controls. DCs were washed and resuspended in RPMI medium plus 10% FCS and incubated with allogeneic PBLs (105/well) in 96-well plates at different PBL/DC ratios for 6 days. Results are shown for the PBL/DC ratio of 64:1. Additional controls included DC alone, 4-OH-IF-treated DCs alone, or PBLs alone. Cell culture supernatants were collected after 6 days, and (A) IFN-γ and (B) IL-12p70 levels were determined using ELISA specific for each cytokine. Results in panel A represent the mean of triplicate samples ± SD from 3 separate experiments. Results in panel B represent the mean of triplicate samples ± SD from 1 experiment. *P < .05.
IFN-γ production could be restored by reconstituting the GSH levels in 4-OH-IF-treated DCs with GSH-OEt at the start of the culture (Figure 5A). Given that allogeneic cultures were set up in parallel to measure lymphocyte proliferation and IFN-γ production, Figure 4C illustrates the GSH levels for DCs used in both systems. GSH levels in 4-OH-IF-treated DCs were 50% of control values, and further treatment with GSH-OEt reconstituted GSH levels to 90% of control values (Figure 4C). IL-12p70 was detectable in only 1 of 4 allogeneic cultures, but a result similar to that for IFN-γ was obtained in that allogeneic cultures containing 4-OH-IF-treated DCs had lower levels of IL-12p70 than cultures containing untreated DCs. IL-12p70 production was also restored in cultures containing 4-OH-IF- and GSH-OEt-treated DCs (Figure 5B).
4-OH-IF reduces LPS- and IFN-γ-induced IL-12p70 production by DCs
To confirm that 4-OH-IF could inhibit DC IL-12 p70 production, we used an alternative system whereby IL-12p70 was more readily detectable after DC stimulation. DCs treated with LPS and IFN-γ produced low but detectable levels of IL-12p70. Treating the DCs with 4-OH-IF before adding LPS and IFN-γ significantly reduced their ability to produce IL-12p70 in contrast to DCs treated with LPS and IFN-γ alone. Adding GSH-OEt to 4-OH-IF-treated DCs restored their ability to produce IL-12p70 after stimulation with LPS and IFN-γ (Figure 6A). GSH levels were 50% of control values after 4-OH-IF treatment and 100% of control values after 4-OH-IF plus GSH-OEt treatment (Figure 6B).
Ifosfamide reduces IL-12p70 production by LPS- and IFN-γ-stimulated DCs. (A).DCs were treated with 4-OH-IF for 90 minutes or with 4-OH-IF and then GSH-OEt at a final concentration of 0.4 mM for 5 hours. Untreated cells were used as controls. DCs at 5 × 104/well were then treated with 1 μg/mL LPS and 1 ng/mL IFN-γ for 24 hours, after which the supernatants were collected and IL-12p70 levels determined using ELISA. Results represent the mean ± SD of triplicate samples from 3 separate experiments. **P < .01. (B) 4-OH-IF- and 4-OH-IF plus GSH-OEt-treated DCs were washed, and GSH levels were measured by HPLC. Untreated cells were used as controls. Results are expressed as the percentage of control values and represent the mean ± SD from 3 treatments. **P < .01.
Ifosfamide reduces IL-12p70 production by LPS- and IFN-γ-stimulated DCs. (A).DCs were treated with 4-OH-IF for 90 minutes or with 4-OH-IF and then GSH-OEt at a final concentration of 0.4 mM for 5 hours. Untreated cells were used as controls. DCs at 5 × 104/well were then treated with 1 μg/mL LPS and 1 ng/mL IFN-γ for 24 hours, after which the supernatants were collected and IL-12p70 levels determined using ELISA. Results represent the mean ± SD of triplicate samples from 3 separate experiments. **P < .01. (B) 4-OH-IF- and 4-OH-IF plus GSH-OEt-treated DCs were washed, and GSH levels were measured by HPLC. Untreated cells were used as controls. Results are expressed as the percentage of control values and represent the mean ± SD from 3 treatments. **P < .01.
Treating DCs with 4-OH-IF or BSO did not significantly reduce their capacity to present exogenously added tyrosinase peptide to tyrosinase-specific CTLs
Treating mature DCs with 4-OH-IF or BSO did not significantly inhibit their ability to present exogenously added tyrosinase peptide in association with MHC class 1 molecules to tyrosinase-specific CTLs, as measured by IFN-γ production (Figure 7A). 4-OH-IF and BSO significantly reduced GSH levels in DCs to 45% and 52% of control values, respectively (Figure 7B).
Ifosfamide and BSO have no effect on DC antigen-specific T-cellstimulation. (A) DCs were cultured for 6 days in medium containing GM-CSF and IL-4 alone. TNF-α (800 U/mL) was added from days 6 to 8 of culture. BSO (0.5 mM) was added for 24 hours on day 7, and ifosfamide (100 μM) was added for 90 minutes on day 8. Treated and untreated DCs were then plated at 104/well in 100 μL medium in 96-well round-bottom plates and pulsed with tyrosinase peptide (1-10 μg/mL) for 2 hours. Tyrosinase-specific T cells (2 × 104) were then added in a final volume of 100 μL to each well in medium containing 20% FCS and 100 U/mL IL-2. Control cultures containing non-tyrosinase-pulsed DCs, DCs alone, or CTLs alone were also included. Supernatants (100 μL) were removed from each well after 24 hours and assayed for IFN-γ production using an ELISA kit specific for IFN-γ. Results represent the mean ± SD of triplicate samples from 1 of 3 representative experiments. (B) 4-OH-IF- or BSO-treated DCs were washed, and GSH levels were measured by HPLC. Untreated cells were used as controls. Results are expressed as the percentage of control values and represent the mean ± SD from 3 treatments. *P < .05.
Ifosfamide and BSO have no effect on DC antigen-specific T-cellstimulation. (A) DCs were cultured for 6 days in medium containing GM-CSF and IL-4 alone. TNF-α (800 U/mL) was added from days 6 to 8 of culture. BSO (0.5 mM) was added for 24 hours on day 7, and ifosfamide (100 μM) was added for 90 minutes on day 8. Treated and untreated DCs were then plated at 104/well in 100 μL medium in 96-well round-bottom plates and pulsed with tyrosinase peptide (1-10 μg/mL) for 2 hours. Tyrosinase-specific T cells (2 × 104) were then added in a final volume of 100 μL to each well in medium containing 20% FCS and 100 U/mL IL-2. Control cultures containing non-tyrosinase-pulsed DCs, DCs alone, or CTLs alone were also included. Supernatants (100 μL) were removed from each well after 24 hours and assayed for IFN-γ production using an ELISA kit specific for IFN-γ. Results represent the mean ± SD of triplicate samples from 1 of 3 representative experiments. (B) 4-OH-IF- or BSO-treated DCs were washed, and GSH levels were measured by HPLC. Untreated cells were used as controls. Results are expressed as the percentage of control values and represent the mean ± SD from 3 treatments. *P < .05.
Discussion
The alkylating drug ifosfamide is a widely used antineoplastic agent.1-3 In the present study we used 4-hydroperoxyifosfamide as a prodrug for 4-hydroxyifosfamide (4-OH-IF), the activated form of ifosfamide. In addition to its cytostatic effects, activated ifosfamide and its major decomposition product, acrolein, cause the depletion of intracellular glutathione levels in different cell types.4,5 Glutathione is the major intracellular thiol compound that protects cells against oxidative injury and is the major intracellular redox buffer in many cell types.31 We have previously shown that 4-OH-IF dose dependently inhibits the proliferation and cytotoxic responses of subpopulations of lymphocytes. These effects were shown to be dependent on the availability of intracellular GSH.6 NK-cell GSH levels and cytotoxic activity are more resistant to ifosfamide or mafosfamide treatment than CTLs because of the higher initial GSH levels and the elevated level of GSH synthesis in NK cells.6,7 Although the effect of 4-OH-IF and the subsequent GSH depletion has been studied in T cells and NK cells, little is known about the effects of 4-OH-IF on GSH depletion in APCs such as monocytes and DCs. In the present study we compared GSH levels in T cells, NK cells, monocytes, and immature and mature DCs and found that when comparing cells from the same donors, monocytes and DCs had higher constitutive levels of GSH than T cells and NK cells. 4-OH-IF (100 μM) reduced GSH levels in DCs to 50% of control values, whereas T-cell and NK-cell GSH levels were reduced to 10% of control values. In agreement with our previous study,6 we found that NK cells were less sensitive to 4-OH-IF treatment than T cells because 4-OH-IF (50 μM) reduced GSH levels to only 80% of control values in NK cells but to approximately 20% of the control values in T cells.
BSO, which inhibits GSH synthesis by inactivating γ glutamyl-cysteine synthetase, the enzyme catalyzing the rate-limiting step in glutathione biosynthesis,32 significantly reduced GSH levels in all the cell types studied. We also studied the effect of 4-OH-IF and BSO on human monocyte-derived DC function. BSO and 4-OH-IF treatment led to a significant reduction in GSH levels in immature and mature DCs, which was accompanied by a significant reduction in the ability of the DCs to stimulate T-cell proliferation in an allogeneic mixed-leukocyte reaction (MLR). GSH-OEt, which reconstituted DC GSH levels after 4-OH-IF treatment, also restored the allostimulatory capacity of DCs and their ability to stimulate T-cell IFN-γ production in allogeneic cultures. The reduction in cell proliferation and cytokine production observed was not caused by a direct cytotoxic effect of 4-OH-IF because there was no change in the viability of the cells after treatment. We have also previously shown that the proliferative activity of lymphocytes could be restored after GSH depletion with BSO but not after treatment with 4-OH-IF6 because 4-OH-IF irreversibly inhibits cell proliferation by alkylating biomolecule nucleophilic centers.33 The fact that the reduction in cell proliferation observed in our DC/PBL cultures could be reconstituted with GSH-OEt after ifosfamide or BSO treatment rules out the possibility that any residual 4-OH-IF directly inhibited T-cell proliferation and supports the view that DC GSH levels play an important role in T-cell proliferation and IFN-γ production.
The induction of alloreactive PBL proliferation by DCs can be influenced by several factors such as DC maturation, costimulatory molecule expression, and cytokine environment. We found no significant decrease in the expression of the DC maturation marker CD83, the costimulatory molecules CD40 and CD86, or MHC class 1 and HLA-DR molecules after 4-OH-IF or BSO treatment.
DCs from patients with hepatitis C virus infection (HCV-DC) stimulate allogeneic DCs to a lesser extent than normal DCs and have lower levels of IFN-γ in allogeneic cultures containing HCV-DCs. With the exception of CD86, HLA molecule expression and costimulatory molecule expression are the same in HCV-DCs and normal DCs.34 The reduction in cell proliferation and IFN-γ production could be overcome by adding IL-12 to the medium.34 Although HCV-DCs had a reduced allostimulatory capacity, their ability to stimulate T cells with recall antigens was unimpaired.34 In our study we found that 4-OH-IF-treated DCs had a reduced allostimulatory capacity, but their ability to stimulate tyrosinase-specific T cells with tyrosinase peptide was unimpaired.
Short and coworkers35 found, when using murine spleen cells, that severe GSH depletion in APCs (more than 70%) diminishes their ability to stimulate T-cell proliferation and cytokine production, though only a 20% decrease in APC GSH is sufficient to markedly decrease T-cell IFN-γ production.17 It has also been suggested that the key events that determine whether IFN-γ is produced occur almost immediately after APCs come into contact with responding T cells.17
Endogenous IL-12 plays a key role in cell proliferation at the sensitizing phase of an MLR,36 and IL-12 can also induce T-cell IFN-γ production.37 Intracellular GSH levels in macrophages are known to be critical for the secretion of IL-12.16,38,39 We found that 4-OH-IF could significantly reduce GSH levels and IL-12 production by DCs, suggesting that IL-12 may play a role in the decrease in T-cell stimulation and IFN-γ production observed in our study. The fact that GSH-OEt could overcome 4-OH-IF-induced DC GSH depletion and impaired cytokine production and T-cell stimulation indicated that the regulatory effect of 4-OH-IF was a result of its effects on intracellular GSH levels in the DCs.
Ifosfamide is also known to deplete the plasma thiols cysteine and homocysteine in addition to GSH.40,41 Cysteine released by macrophages can increase the intracellular GSH levels of activated T cells in the vicinity.42 Monocyte-derived DCs also release cysteine into the extracellular space after stimulation with allogeneic T cells, providing a reducing microenvironment that facilitates T-cell activation.43 Thus, ifosfamide may also inhibit T-cell responses in patients by reducing available cysteine levels.
Overall, our results suggest that the cytostatic drug ifosfamide, which is commonly used in the treatment of malignancies, can deplete intracellular GSH levels in human myeloid DCs, leading to reduced DC ability to activate naive T cells. The concentration of ifosfamide used in our study was within a clinically relevant range. GSH-OEt, which reconstitutes intracellular GSH levels, reversed the inhibitory effect of 4-OH-IF on DC/T-cell stimulatory capacity. Therefore, in patients with tumors, therapeutic strategies aimed at reconstituting GSH levels after ifosfamide treatment may promote DC functional activity.
Prepublished online as Blood First Edition Paper, July 10, 2003; DOI 10.1182/blood-2003-05-1408.
Supported by the Deutsche Krebshilfe project 702301-Is/2 and grant SFB 455, Project B9.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Baxter Medical, Munich, for providing the ifosfamide used in this study.

![Figure 4. Reduction in DC allostimulatory capacity after 4-OH-IF and BSO treatment and restoration with GSH-OEt. (A) DCs were treated with 4-OH-IF (100 μM) alone for 90 minutes on day 8 or with 4-OH-IF for 90 minutes and then with GSH-OEt (0.4 mM) for 5 hours. Untreated cells from parallel day-8 cultures were used as controls. DCs were irradiated and incubated with PBLs (105/well) at different PBL/DC ratios for 6 days. Results are shown for the PBL/DC ratio of 32:1. *P < .05. (B) DCs were treated with BSO (0.5 mM) alone on day 7 for 24 hours or with BSO for 24 hours and then with GSH-OEt (5 mM) for 5 hours. DCs were irradiated and resuspended in RPMI medium plus 10% FCS and incubated with allogeneic PBLs (105/well) in 96-well plates at PBL/DC ratios ranging from 2:1 to 64:1 for 6 days. Results are shown for the PBL/DC ratio of 64:1. BSO-treated DCs alone, 4-OH-IF-treated DCs alone, untreated DCs alone, or PBLs alone were used as controls. The amount of [3H]-thymidine incorporated during the last 24 hours of culture was measured (A-B). Results are expressed as the mean ± SD of cpm values of triplicate cultures from 1 of 3 representative experiments. *P < .05. (C) 4-OH-IF and 4-OH-IF plus GSH-OEt-treated DCs and (D) BSO and BSO plus GSH-OEt-treated DCs were also washed, and GSH levels were measured by HPLC. Untreated cells were used as controls. Results are expressed as the percentage of control values and represent the mean ± SD from 3 treatments. *P < .05.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/102/10/10.1182_blood-2003-05-1408/6/m_h82235226004.jpeg?Expires=1768307586&Signature=gKNO-jSd1rSXBrVPK87bZjMcCtjG-pz2vwdII9F-gNTNek5Df8JsMfwptVgmldiKlRTOvwG5gaM-thfsMnnfWMZob4f6MY0s9jky-XZEhn~kV1uILGItN-v088LW0bL~aYq~awyQq6SrOuRHnJoWFtwxZ38sv70gBHyo30HeViifAl8NNZhFJAuJUxBs~aIGc3i82-22~VNar6PMScSmvrgY~Q60AxosvdpyWm3IXaIKpy0rY4p9TWCUhS4RE2d3VdXyG92FDRxa0x-VB3U~I-8mtcjF7OH2In~er~yhrGja1u7k7mjfmjWZUkwIgJP1303wPCXFS0Oz3PMRxygWOA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


![Figure 4. Reduction in DC allostimulatory capacity after 4-OH-IF and BSO treatment and restoration with GSH-OEt. (A) DCs were treated with 4-OH-IF (100 μM) alone for 90 minutes on day 8 or with 4-OH-IF for 90 minutes and then with GSH-OEt (0.4 mM) for 5 hours. Untreated cells from parallel day-8 cultures were used as controls. DCs were irradiated and incubated with PBLs (105/well) at different PBL/DC ratios for 6 days. Results are shown for the PBL/DC ratio of 32:1. *P < .05. (B) DCs were treated with BSO (0.5 mM) alone on day 7 for 24 hours or with BSO for 24 hours and then with GSH-OEt (5 mM) for 5 hours. DCs were irradiated and resuspended in RPMI medium plus 10% FCS and incubated with allogeneic PBLs (105/well) in 96-well plates at PBL/DC ratios ranging from 2:1 to 64:1 for 6 days. Results are shown for the PBL/DC ratio of 64:1. BSO-treated DCs alone, 4-OH-IF-treated DCs alone, untreated DCs alone, or PBLs alone were used as controls. The amount of [3H]-thymidine incorporated during the last 24 hours of culture was measured (A-B). Results are expressed as the mean ± SD of cpm values of triplicate cultures from 1 of 3 representative experiments. *P < .05. (C) 4-OH-IF and 4-OH-IF plus GSH-OEt-treated DCs and (D) BSO and BSO plus GSH-OEt-treated DCs were also washed, and GSH levels were measured by HPLC. Untreated cells were used as controls. Results are expressed as the percentage of control values and represent the mean ± SD from 3 treatments. *P < .05.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/102/10/10.1182_blood-2003-05-1408/6/m_h82235226004.jpeg?Expires=1768307587&Signature=p3nlDnwad-UAT5KVle7Tka63Xjr0oZhSrBAoQVfR-zQvsLdeKDnRKLxPQiU-NdtZ9ixf2AzttYSvkmBGCtStSS~M-kXirDOQqHCIIfndCjEXSMsOcorncXZ1AHCHXWZFd~5Q5CJ0-FT~NWgWfk0ymlsf7Yqi6BKaSI6OBDM2aD12wMHkTsTf9ZK33LGkXLIMFWuuaICJ6oIH4x19fVo18hAT90nEJeCYpKHINYiErphe1BQHyv4bxbImZ~CuMldhCn0Gz7-AIpj3CJJHE1JvcxWmgUvyLi33GBncwqslxpFeMA-l1cCEE3oMbDpzglZqaWY07MiERy5VMfoXdoetJA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)