Abstract
BACKGROUND: Mantle cell lymphoma (MCL) typically has a poor outcome with overall survival of only 3–4 years. Higher treatment response and event-free survival has been demonstrated with aggressive high dose chemotherapy followed by autologous hematopoietic stem cell support, though long term cure rates remain unclear(Dreger P. Hematol J. 2000;vol.2). Modest response rates have also been reported with the monoclonal antibody (MoAb) rituximab and ALEMTUZUMAB (Foran, JM. JCO 2000; vol. 2. Faderl S. Blood 2003; vol. 9). We therefore combined dose-dense therapy with MoAbs to explore response rate and event free survival (EFS) in mantle cell lymphoma. The strength of this trial design is ability to follow all patients from induction chemotherapy through high dose therapy and transplant in order to gauge clinical outcome on all enrolled patients, not just the subpopulation who is able to proceed to high dose therapy.
PATIENTS AND METHODS: Induction therapy consisted of 1 cycle of high dose cytarabine (3gm/m2 IV over 1 hour Q12H for 8 doses), mitoxantrone (10mg/m2 daily for 3 days), and ALEMTUZUMAB 30mg IV 3 times a week for 6 weeks with growth factor support. All responding patients were mobilized with cyclophosphamide 4gm/m2 and G-CSF 10 mcg/kg/day and/or bone marrow harvest. The transplant preparative regimen was carmustine 15mg/kg over 2 hours day -6, etoposide 60mg/kg over 4 hours day -4, and cyclophosphamide 100mg/kg over 2 hours day -2 followed by autologous reinfusion on day zero. Consolidation was given with rituximab 375mg/m2 weekly for 4 doses at 6 weeks and 6 months post transplant.
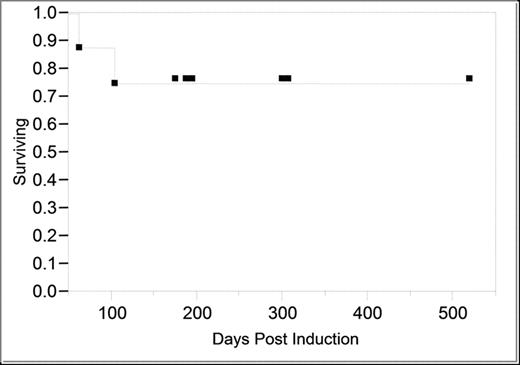
RESULT: 9 patients with advanced disease (7 stage IV, 1 stage III, 1 stage IIA) and median age of 60 (48 – 65 years) have been accrued and treated since February 2003. Four were newly diagnosed and 5 had relapsed/refractory disease. Seventy eight percent (7/9) had complete response and 22% (2/9) had partial response (PR) following induction therapy. One patient had severe infection after induction and was unable to proceed to transplant. Another had constitutional decline preventing further therapy and each died within 4 months of withdrawal from the protocol. Both had relapse/refractory disease at accrual. The remaining 7 patients proceeded to the transplant phase. With a median follow-up of 7 months (range 3–16 months), all 7 patients remain in CR for 1 –16 months. Significant induction therapy toxicity included neutropenia in all 9 patients with average duration of 10.7 days, non-disseminated CMV reactivation in 44% of patients, one overwhelming fungal infection, and one patient with delay in engraftment.
CONCLUSION: Our preliminary data show a high induction and transplant phase completion rate, manageable toxicity, and excellent overall response rate in this group of elderly patients with advanced disease. Larger numbers of patients and longer follow-up is needed to confirm these promising results.
Author notes
Corresponding author