Hematopoietic cells are often exposed to transient hypoxia and reoxygenation as they develop and migrate. Given that bone marrow (BM) failure occurred in patients with Fanconi anemia (FA), we reason that hypoxia-then-reoxygenation represents a physiologically relevant stress for FA hematopoietic progenitor/stem cells. Here we show that expansion of Fancc–/– BM cells enriched for progenitor and stem cells was significantly decreased after 2 continuous cycles of hyperoxic-hypoxic-hyperoxic treatments compared with wild-type (WT) BM cells. This inhibition was attributable to a marked decrease of lineage-depleted (Lin–) ScaI– c-kit+ cells and more primitive Lin– ScaI+ c-kit+ cells in Fancc–/– BM cells following reoxygenation. Evaluation of the cell-cycle profile of long-term BM culture (LTBMC) revealed that a vast majority (70.6%) of reoxygenated Fancc–/– LTBMC cells was residing in the G0 and G1 phases compared with 55.8% in WT LTBMC cells. Fancc–/– LTBMC cells stained intensely for SA-β-galactosidase activity, a biomarker for senescence; this was associated with increased expression of senescence-associated proteins p53 and p21WAF1/CIP1. Taken together, these results suggest that reoxygenation induces premature senescence in Fancc–/– BM hematopoietic cells by signaling through p53, up-regulating p21, and causing senescent cell-cycle arrest. Thus, reoxygenation-induced premature senescence may be a novel mechanism underlying hematopoietic cell depletion and BM failure in FA.
Introduction
Hypoxia represents a stress that induces cell growth arrest and injury.1 In tumorigenesis, hypoxia can act as a selective pressure for the elimination of cells with apoptotic potential and the clonal expansion of cancer cells.2 In response to hypoxia, cells increase expression of a variety of gene products such as erythropoietin, vascular endothelial growth factor (VEGF), glycolytic enzymes, and p27 to prevent death or slow growth.3-5 The transcriptional factor hypoxia inducible factor-1α (HIF-1α) is known to play fundamental roles in hypoxic response.6-8 The tumor suppressor p53, stabilized by HIF-1α, facilitates growth arrest or cell death under hypoxic condition through its downstream genes such as p21WAF1/CIP1 and bax.9-11
In the blood system, hematopoietic cells are often exposed to transient hypoxia and reoxygenation as they develop and migrate between blood and tissues. Continuous cycles of hypoxia-then-reoxygenation have long been known to increase in the production of oxidants,12 which could cause DNA damage, protein oxidation, and lipid peroxidation.13,14 It has been proposed that bone marrow (BM) hematopoietic stem and progenitor cells are distributed in areas of different oxygen (O2) concentrations, with stem cells residing in hypoxic areas and progenitor cells in high O2 areas.15,16 Migration between these areas of different oxygen gradients can generate reoxygenated oxidative stress. Indeed, elevated levels of reactive oxygen species (ROSs) have been implicated in the pathways of reperfusion injury to stem cells and myocardial tissue.17-19 Oxidative stress generated by hypoxia-reoxygenation can also cause hemorrhagic shock, which often requires replacement of immune and other blood cells.20-22 In human colorectal cell line RKO and lymphoblasts, hypoxia-then-reoxygenation induces DNA damage and activates p53, which can be inhibited by the ROS scavenger N-acetyl-L-cysteine (NAC).23 Furthermore, reoxygenation-induced DNA damage and p53 activation are dependent on the protein kinase ATM.23 Oxidative stress-induced DNA damage is well known to cause loss of cell replication and multiple molecular changes involved in premature senescence, such as up-regulation of senescence-associated proteins p53, p21WAF1/CIP1, and p16INK4A, and permanent growth arrest.24
Fanconi anemia (FA) is a genetic disease characterized by progressive BM failure, variable congenital anomalies, and a predisposition to cancer.25-27 Somatic cell fusion studies show that FA is genetically heterogeneous, with at least 11 complementation groups identified thus far.28 The genes encoding the groups A (FANCA), B (FANCB), C (FANCC), D1 (FANCD1/BRCA2), D2 (FANCD2), E (FANCE), F (FANCF), G (FANCG), and L (FANCL) have been cloned.29-37 The most important clinical features of FA are hematologic, as the progressive BM failure represents the hallmark of the disease and the leading cause of patient death.38 It has been proposed that BM failure in aplastic anemia including FA results from hematopoietic stem cell (HSC) depletion.39 Since FA hematopoietic progenitor and stem cells have high rates of stress-induced apoptosis and reduced repopulating ability,26,40 the FA proteins are believed to play important roles in the maintenance of HSCs. Indeed, consistent with the observations that the cells derived from FA patients are intolerant of oxidative stress, it has been reported that FA proteins, particularly the complementation group C (FANCC) protein, play a crucial role in oxidative stress signaling in a variety of cell types including hematopoietic cells.41-46 Given that hematopoietic cells are often exposed to transient hypoxia as they develop and migrate between blood and tissues, we hypothesized that hypoxia-reoxygenation represents a physiologic stress for FA hematopoietic progenitor/stem cells and sought to determine the effects of reoxygenation in the survival and maintenance of FA hematopoietic progenitor/stem cells. Our study demonstrates that oxidative stress induced by hyperoxic-hypoxic-hyperoxic treatments can induce senescence of Fancc–/– hematopoietic progenitor/stem cells and suggests that stress-induced premature senescence may be a novel mechanism underlying HSC depletion and BM failure in FA.
Materials and methods
Mice
Wild-type (WT) and Fancc–/– mice were generated by interbreeding the heterozygous Fancc+/– mice (a generous gift from Dr Manuel Buchwald, University of Toronto; Chen et al47 ). The genetic background of the mice is C57BL/6. All of the mice were used at approximately 8 to 10 weeks of age. All experimental procedures conducted in this study were approved by the Institutional Animal Care and Use Committee of Cincinnati Children's Hospital Medical Center.
Isolation of BM Lin– cells and short-term culture
The femora and tibiae were harvested from the mice immediately after they were killed with CO2. BM cells were flushed from the bones into Iscoves modified Dulbecco medium (IMDM; Invitrogen, Frederick, MD) containing 10% fetal calf serum (FCS) using a 21-gauge needle and syringe. Low-density BM mononuclear cells (BMMNCs) were separated by Ficoll-Hypaque density gradient (Sigma, St Louis, MO) and washed with IMDM. BMMNCs were depleted of lineage-committed cells using a lineage cell depletion kit (Miltenyi Biotec, Auburn, CA) in accordance with the manufacturer's instruction. BMMNCs were enriched for HSCs and progenitors by staining with biotin-conjugated lineage antibodies specific for murine CD5, Mac-1, CD45R/B220, Ter-119, and Gr-1. The efficiency of depletion was approximately 95% as analyzed using a Quality-Control Staining kit provided by the manufacturer, which contains a Biotin Lineage cocktail against lineage markers/antibiotin-APC (catalog no. 130-090-865; Miltenyi Biotec). The resulting BM lineage-depleted (Lin–) cells were cultured in IMDM medium containing 100 ng/mL stem cell factor (SCF), 20 ng/mL interleukin-6 (IL-6), and 50 ng/mL Flt-3 ligand (Flt-3L; R & D Systems, Minneapolis, MN). There were 3 sets of cells incubated in parallel: (1) the control cultures were incubated at 37°C in hyperoxia (humidified air with 21% O2, 5% CO2); (2) the reoxygenated cultures were subjected to 2 cycles of hypoxia (within a modular incubator chamber [BioSpherix, Redfield, NY] filled with 1% O2, 5%CO2, and balance N2) for 4 hours then hyperoxia for 1 hour; (3) the reoxygenated NAC cultures were the same as those in number 2 except that the medium contained the ROS scavenger NAC at a concentration of 1 mM. The cells were then incubated in 21% oxygen for 10 days.
Construction of retroviral expression vectors and transduction
The full-length human FANCC cDNA35 was amplified by polymerase chain reaction (PCR), using Pfu DNA polymerase (Stratagene, La Jolla, CA) from pLXSN-FANCC48 and subcloned into the NotI site of retroviral vector MIEG3 (a gift from Dr Yi Zheng, Cincinnati Children's Hospital Medical Center) to create MIEG3-FANCC. The MIEG3 and MIEG3-FANCC plasmids (10 μg each) were used to produce retroviral supernatant. The Fancc–/– Lin– BM cells were prestimulated with 100 ng/mL SCF, 20 ng/mL IL-6, and 50 ng/mL Flt-3L (R & D Systems) for 48 hours. After prestimulation, cells were infected with the MIEG3 and MIEG3-FANCC retroviruses on recombinant human fibronectin fragment CH-296, RetroNectin (Takara, Kyoto, Japan). Viruses were removed after 24 hours and fresh viruses were added for additional 24 hours. After final removal of virus-containing media, cells were cultured in growth medium for analysis of expansion and progenitor activity.
Long-term BM culture (LTBMC)
LTBMC was performed essentially as described by Frimberger et al.49 Briefly, BMMNCs at 3 × 106/mL in 10 mL IMDM supplemented with 20% horse serum, 10–5 M hydrocortisone, 10–5 M 2-mercaptoethanol, 100 units/mL penicillin, and 100 μg/mL streptomycin were subjected to hyperoxic or hyperoxic-hypoxia-hyperoxic treatments as described in “Isolation of BM Lin– cells and short-term culture.” The cells were overlaid on the pre-established FBMD-1 feeder stoma layers, and fed weekly by removal of one-half of the supernatant medium and replacement with fresh medium. After 2 weeks of culture, nonadherent hematopoietic cells were collected from supernatant, and adherent cells were harvested after digestion of stromal cell layer with trypsin and removal of stromal cells by brief adherence of the cells to plastic for 1 hour at 37°C. The nonadherent and adherent hematopoietic cells were counted and harvested for further analyses.
Apoptosis assay
Aliquots of 5 × 105 to 1 × 106 BM Lin– or LTBMCs were resuspended in 1x binding buffer (100 μL containing 10 mM HEPES [N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid, pH 7.4], 140 mM NaCl, and 2.5 mM CaCl2) containing 3 μL annexin V–fluorescein isothiocyanate (FITC; PharMingen, San Diego, CA). The cell suspension was gently mixed and incubated for 15 minutes at room temperature. The cells were diluted in 1× binding buffer (400 μL) and analyzed by flow cytometry, using a FACSCalibur (Becton Dickinson, San Jose, CA). For apoptosis in the Lin– ScaI– c-kit+ and Lin– ScaI+ c-kit+ cell populations, BM Lin– cells were stained with Sca-1–phycoerythrin (PE) and c-kit–APC antibodies for 20 minutes at 4°C in the dark. These cells were washed twice with 0.1% bovine serum albumin (BSA)/phosphate-buffered saline (PBS) (1 mL) before annexin V staining. These experiments also included PE and APC isotype controls, and FITC-positive and -negative controls. Apoptosis was therefore analyzed in different populations of Lin– cells. For apoptosis in the LTBMCs, we used a polyclonal antibody (PharMingen) to the active form of caspase 3 in a flow cytometric assay to detect cells in the early stages of apoptosis, which has been described in detail elsewhere.50 Cell cycle was analyzed by fluorescence-activated cell sorter (FACS) of DNA content using propidium iodide staining. Briefly, the LTBMC cells were fixed by 0.25% formaldehyde in PBS, permeabilized by 0.3% nonidet P-40 (NP-40), and then stained with propidium iodide (PI) containing 1 mg/mL RNase A, followed by FACS analysis of the G0/G1, S, and G2/M populations.
Clonogenic progenitor cell assays
BM Lin– or LTBMCs (1 × 105) were pretreated as follows: for reoxygenated groups, cells were subjected to 2 cycles of hypoxia (1% O2) for 4 hours then hyperoxia (21% O2) for 1 hour; for control groups, cells were incubated in hyperoxia (21% O2) for the same period of time as the reoxygenated groups. All groups were then cultured in hyperoxia (21% O2) in a 35-mm tissue culture dish in 4 mL semisolid medium containing 3 mL MethoCult M 3134 (Stem Cell Technologies, Vancouver, BC) and the following growth factors: 100 ng/mL SCF, 10 ng/mL recombinant human IL-3 (rhIL-3), 100 ng/mL granulocyte colony-stimulating factor (G-CSF), and 4 U/mL erythropoietin. Colony-forming units of granulocyte-monocyte (CFU-GMs) and burst-forming units of erythroid (BFU-Es) were scored on days 7 and 14, respectively, using a dissecting microscope (model MZ125; Leica, Solms, Germany). Colony growth results were expressed as mean (of triplicate plates) ± SD colonies per 105 cells plated. Levels of significance were determined using Student t-distribution.
Comet assay
The generation of DNA strand breaks was assessed by the single-cell gel electrophoresis (comet) assay,51 using a Fpg-FLARE (fragment length analysis using repair enzymes) comet assay kit in accordance with the manufacturer's instructions (Trevigen, Gaithersburg, MD). For each experimental point, at least 3 different cultures were analyzed, and 50 cells were evaluated from each culture. Comet tail length and tail moment were measured under a fluorescence microscope (Nikon model 027012; Tokyo, Japan) using an automated image analysis system based on a public domain National Institutes of Health (NIH) image program.52
SA-β-gal activity analysis
SA-β-galactosidase (SA-β-gal) activity was determined using an SA-β-gal staining kit from Cell Signaling Technology (Beverly, MA) according to the manufacturer's instruction. Briefly, cells were washed in PBS and fixed in 2% formaldehyde–0.2% glutaraldehyde. Then the cells were washed and incubated at 37°C overnight with fresh senescence-associated β-gal stain solution (1 mg 5-bromo-4-chloro-3-indolyl-β-D-galactopyranoside [X-Gal] per mL, 40 mM citric acid–sodium phosphate [pH 6.0], 150 mM NaCl, 2 mM MgCl2, 5 mM potassium ferrocyanide, 5 mM potassium ferricyanide). Senescent cells were identified as blue-stained cells by standard light microscopy, and a total of 1000 cells were counted in random fields on a slide to determine the percentage of SA-β-gal–positive cells. Photography of cells was performed on a Leica microscope with Sony digital imaging.
Immunocytochemistry
Cells were cytospun onto slides and fixed in ice-cold methanol for 5 minutes in –20°C. After air drying, cells were blocked for 1 hour with 5% normal serum. Then cells were incubated with primary antibodies (anti-p53ser15 and anti-p21WAF1/CIP1; Cell Signaling) in PBS with 2% normal serum at room temperature for 1 hour. After extensive washes, cells were incubated with FITC-conjugated goat antirabbit (Roche, Milan, Italy) or PE-conjugated goat antimouse antibody (Jackson, Bar Harbor, ME). DNA was then labeled with DAPI (4,6 diamidino-2-phenylindole; Sigma). Slides were finally mounted in mounting medium (Vector, Burlingame, CA). Cells were viewed and photographed using a Leica DM IRB microscope at × 10 magnification with an ORCA-ER C4742-95 camera (Hamamatsu, Hamamatsu City, Japan). The captured images were processed using OpenLab 3.1 software (Improvision, Lexington, MA) and displayed with Adobe Photoshop V6.0 (San Jose, CA).
RNA isolation and reverse-transcriptase (RT)–PCR
Total RNA was prepared with RNeasy kit (Qiagen, Valencia, CA) following the manufacturer's procedure. Reverse transcription was performed with random hexamers and Superscript II RT (Invitrogen) and was carried out at 42°C for 60 minutes and stopped at 95°C for 5 minutes. These reactions were followed by PCR using primers specific for p16ink4a, TCCGCTGCAGACAGACTGGCCAG (sense) and CATCGCGCACATCCAGCCGAGC (antisense); p19Arf, AAGAAGTCTGCGTCGGCGAC (sense) and AGTACCGGAGGCATCTTGGACA (antisense), along with 18S rRNA-specific primers (Ambion), with thermal cycling parameters: 95°C for 5 minutes; 15, 20, or 30 cycles at 95°C for 1 minute, 55°C for 1 minute, and 72°C for 1 minute; and a final extension at 72°C for 10 minutes.
Statistics
Data were analyzed statistically using a Student t test. The level of statistical significance stated in the text was based on the P values. P < .05 was considered statistically significant. The number of individual replicates used to generate means for each experiment is mentioned in the figure legend.
Results
Hyperoxic-hypoxic-hyperoxic treatment inhibits expansion of Fancc–/– hematopoietic progenitor and stem cells
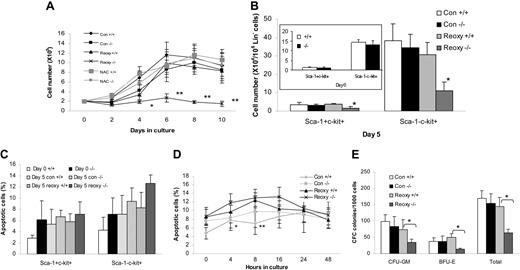
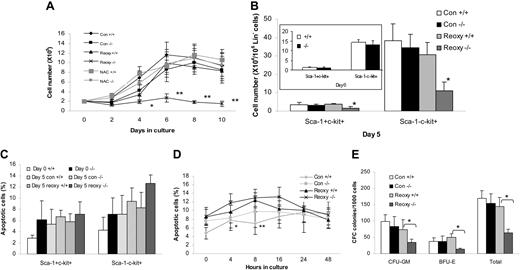
To study the effect of hypoxia-then-reoxygenation on the expansion and maintenance of Fancc–/– hematopoietic progenitor and stem cells, we subjected Lin– BM cells isolated from WT and Fancc–/– mice to 2 cycles of 1% O2 then 21% O2 treatments. It is known that the oxygen tension in bone marrow environment is approximately 3% to 5%, which is generally considered hypoxic.15,16 Therefore, the culture conditions at 1% or 21% oxygen used in our experiments are considered hypoxic or hyperoxic, respectively. Because the reoxygenated cultures underwent 21%-1%-21% oxygen shift, we use the nomenclature “hyperoxic-hypoxic-hyperoxic” throughout the text to accurately reflect the experimental conditions. Because the Fancc-deficient mice have a profound defect in the hematopoietic stem and progenitor cell compartment and because FA HSCs and progenitors are hypersensitive to a variety of stresses,26,38 we reasoned that hyperoxic-hypoxic-hyperoxic treatments might affect the survival and maintenance of Fancc–/– BM cells. Lin– BM cells were isolated from WT and Fancc–/– mice, and incubated in cytokine-conditioned medium under hyperoxia or 2 cycles of hyperoxic-hypoxic-hyperoxic treatments. These cells were then cultured in hyperoxia for 10 days. As shown in Figure 1A, the level of expansion of Fancc–/– BM cells was significantly decreased following reoxygenation, compared with WT BM cells under the same condition (1.3-fold vs 4.9-fold by day 6, respectively). In fact, the absolute number of reoxygenated Fancc–/– BM cells decreased at all time points except day 6 (Figure 1A). However, untreated FA BM cells continued to expand, albeit at a slower rate, during the 10-day period. The expansion of reoxygenated WT BM cells showed some degree of inhibition, albeit not statistically significant when compared with the control WT cells, within the first 2 days following reoxygenation but recovered quickly thereafter (Figure 1A). Treatment of WT and Fancc–/– BM cells with cycles of hyperoxic-hypoxic-hyperoxic treatments in the presence of the ROS scavenger NAC completely abrogated the inhibitory effect (Figure 1A), suggesting that the growth suppression was mediated by oxidative stress. It should be noted that addition of NAC to the normoxic cultures slightly increased growth rates of both WT and Fancc–/– BM cells (data not shown). To determine whether hyperoxic-hypoxic-hyperoxic treatments affected differentiation of the BM cells, we analyzed 0- and 10-day cultures for differentiation by staining the cells with antibodies for lineage (CD5, Mac-1, CD45R/B220, Ter-119, and Gr-1), primitive BM cell (Sca-1, c-kit), lymphoid (CD4, B220), and myeloid (Gr-1, Mac-1) markers. We found no significant difference in the context of differentiation between untreated and hyperoxic-hypoxic-hyperoxic–treated cells or between WT and Fancc–/– cells (Table 1). However, approximately 15% to 20% of BM cells were stained positive for myeloid markers Gr-1 and Mac-1 at day 10, suggesting that these starting Lin– BM cells underwent considerable differentiation after 10 days in culture.
We further analyzed the differential effect of hyperoxic-hypoxic-hyperoxic conditions on expansion of subsets of Lin– BM cells enriched for stem and progenitor cells during the 5-day culture (Figure 1B). WT ScaI+ c-kit+ and ScaI– c-kit+ cells cultured in hyperoxia expanded approximately 2-fold, and hypoxia-reoxygenation did not seem to significantly affect their survival and growth (Figure 1B). In contrast, reoxygenated Fancc–/– ScaI– c-kit+ cells hardly expanded during the 5-day culture. The expansion of Fancc–/– ScaI+ c-kit+ was also inhibited, albeit modestly, at a rate that was 60% slower than their WT counterparts under the same condition (Figure 1B). We next analyzed for apoptosis in the ScaI– c-kit+ and ScaI+ c-kit+ cell populations. Surprisingly, while hyperoxic-hypoxic-hyperoxic treatments increased modestly the percentage of apoptotic cells in Fancc–/– ScaI– c-kit+ cells (12.7% compared with 9.5% for untreated Fancc–/– control), it did not cause significant increase in apoptotic death of Fancc–/– ScaI+ c-kit+ cells (Figure 1C). Considering that apoptosis might have occurred within hours of hyperoxic-hypoxic-hyperoxic treatments, we also performed apoptotic analysis in ScaI+ c-kit+ cell populations at 0, 4, 8, 16, 24, and 48 hours after hyperoxic-hypoxic-hyperoxic treatments. Hyperoxic-hypoxic-hyperoxic treatments result in significant increase of apoptosis in treated Fancc–/– cells compared with untreated Fancc–/– cells 4 hours and 8 hours after treatments (Figure 1D). However, it appears that percentages of apoptotic cells decreased after 16 hours following treatments in both WT and Fancc–/– cells, and that there was almost no difference in apoptosis between the WT and mutant cells after 16 hours of treatments (Figure 1D).
Effects of hyperoxic-hypoxic-hyperoxic treatment on expansion of WT and Fancc–/–BM lin– cells. (A) Growth of WT and Fancc–/– BM lin– cells over 10 days. Cells were incubated in hyperoxia (21% O2; Con: control) only or first subjected to 2 cycles of hypoxia (1% O2) for 4 hours then hyperoxia for 1 hour (Reoxy: reoxygenation). The cells were then incubated in hyperoxia for 10 days. The NAC cultures were the same as the reoxygenated cells except that the medium contained N-acetyl-L-cysteine (NAC) at a concentration of 1 mM. Data represent the mean ± SD of 3 independent experiments. *P < .05 between reoxygenated Fancc–/– cells and untreated Fancc–/– or WT NAC or Fancc–/– NAC samples; **P < .05 between reoxygenated Fancc–/– cells and any one of all other groups. (B) Expansion of BM cells enriched for HSCs and progenitor cells. The inserted panel shows the initial numbers of the Sca-1+ c-kit+ and Sca-1– c-kit+ subpopulations in the BM Lin– cells. WT and Fancc–/– BM lin– cells (1 × 105/mL) were treated as described in panel A. At day 5, the cells were counted and then stained with Sca-1–PE and c-kit–APC antibodies and analyzed by flow cytometry. The cell numbers were calculated by multiplication of the total numbers of cells harvested with the percentage of each phenotype of Lin– cells determined by flow cytometric analysis. The mean ± SD of 3 independent experiments is shown. *Statistical significance between WT and Fancc–/– samples at P < .01. (C) WT and Fancc–/– BM lin– cells described in panel B were counted on day 0 and day 5 after hyperoxic-hypoxic-hyperoxic treatment, stained with Sca-1–PE and c-kit–APC antibodies, and then with annexin V–FITC. Percentages of apoptosis in the 2 subpopulations were analyzed by flow cytometry. Data represent the mean ± SD of 3 independent experiments. (D) Apoptosis in WT and Fancc–/– BM lin– cells described in panel D except that analysis was conducted at 0, 4, 8, 16, 24, and 48 hours after hyperoxic-hypoxic-hyperoxic treatment. Data represent the mean ± SD of 3 independent experiments. *P < .05 between reoxygenated Fancc–/– cells and untreated Fancc–/– cells. **P < .01 between reoxygenated Fancc–/– and reoxygenated WT cells. (E) Effect of reoxygenation on BM progenitor activity. The colony-forming cell (CFC) activity of WT and Fancc–/– BM lin– cells was evaluated after hyperoxia (Con) only or 2 cycles of hyperoxic-hypoxic-hyperoxic treatments (Reoxy). Data shown represent the number (mean ± SD) of CFU-GMs, BFU-Es, and total number of colonies from 3 independent experiments. *Statistical significance between WT and Fancc–/– samples at P < .05.
Effects of hyperoxic-hypoxic-hyperoxic treatment on expansion of WT and Fancc–/–BM lin– cells. (A) Growth of WT and Fancc–/– BM lin– cells over 10 days. Cells were incubated in hyperoxia (21% O2; Con: control) only or first subjected to 2 cycles of hypoxia (1% O2) for 4 hours then hyperoxia for 1 hour (Reoxy: reoxygenation). The cells were then incubated in hyperoxia for 10 days. The NAC cultures were the same as the reoxygenated cells except that the medium contained N-acetyl-L-cysteine (NAC) at a concentration of 1 mM. Data represent the mean ± SD of 3 independent experiments. *P < .05 between reoxygenated Fancc–/– cells and untreated Fancc–/– or WT NAC or Fancc–/– NAC samples; **P < .05 between reoxygenated Fancc–/– cells and any one of all other groups. (B) Expansion of BM cells enriched for HSCs and progenitor cells. The inserted panel shows the initial numbers of the Sca-1+ c-kit+ and Sca-1– c-kit+ subpopulations in the BM Lin– cells. WT and Fancc–/– BM lin– cells (1 × 105/mL) were treated as described in panel A. At day 5, the cells were counted and then stained with Sca-1–PE and c-kit–APC antibodies and analyzed by flow cytometry. The cell numbers were calculated by multiplication of the total numbers of cells harvested with the percentage of each phenotype of Lin– cells determined by flow cytometric analysis. The mean ± SD of 3 independent experiments is shown. *Statistical significance between WT and Fancc–/– samples at P < .01. (C) WT and Fancc–/– BM lin– cells described in panel B were counted on day 0 and day 5 after hyperoxic-hypoxic-hyperoxic treatment, stained with Sca-1–PE and c-kit–APC antibodies, and then with annexin V–FITC. Percentages of apoptosis in the 2 subpopulations were analyzed by flow cytometry. Data represent the mean ± SD of 3 independent experiments. (D) Apoptosis in WT and Fancc–/– BM lin– cells described in panel D except that analysis was conducted at 0, 4, 8, 16, 24, and 48 hours after hyperoxic-hypoxic-hyperoxic treatment. Data represent the mean ± SD of 3 independent experiments. *P < .05 between reoxygenated Fancc–/– cells and untreated Fancc–/– cells. **P < .01 between reoxygenated Fancc–/– and reoxygenated WT cells. (E) Effect of reoxygenation on BM progenitor activity. The colony-forming cell (CFC) activity of WT and Fancc–/– BM lin– cells was evaluated after hyperoxia (Con) only or 2 cycles of hyperoxic-hypoxic-hyperoxic treatments (Reoxy). Data shown represent the number (mean ± SD) of CFU-GMs, BFU-Es, and total number of colonies from 3 independent experiments. *Statistical significance between WT and Fancc–/– samples at P < .05.
We evaluated the effect of hyperoxic-hypoxic-hyperoxic treatments on the clonogenic activity of BM Lin– cells. The total number of clonogenic progenitors (CFCs) was decreased slightly for reoxygenated WT but significantly for the Fancc–/– BM progenitors exposed to the same treatment (Figure 1E). While not statistically significant, reoxygenated WT BM progenitors gave rise to higher BFU-E but lower CFU-GM colonies than untreated WT control (Figure 1E). However, reoxygenated Fancc–/– BM progenitors produced significantly lower amounts of both BFU-E and CFU-GM colonies. These findings indicate that hyperoxic-hypoxic-hyperoxic treatments have an inhibitory effect on Fancc–/– BM progenitor activity.
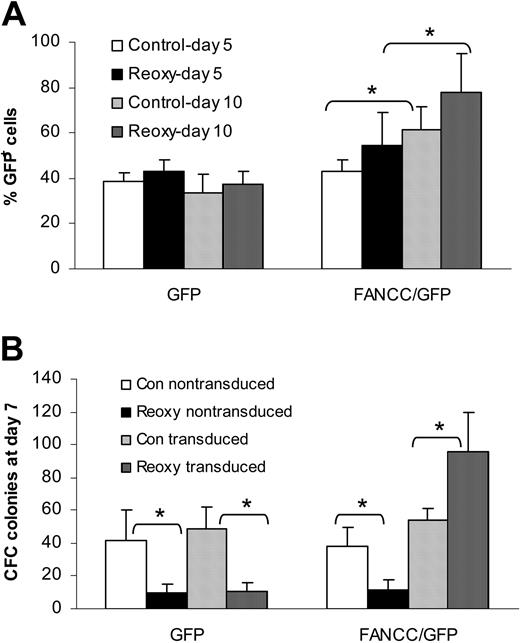
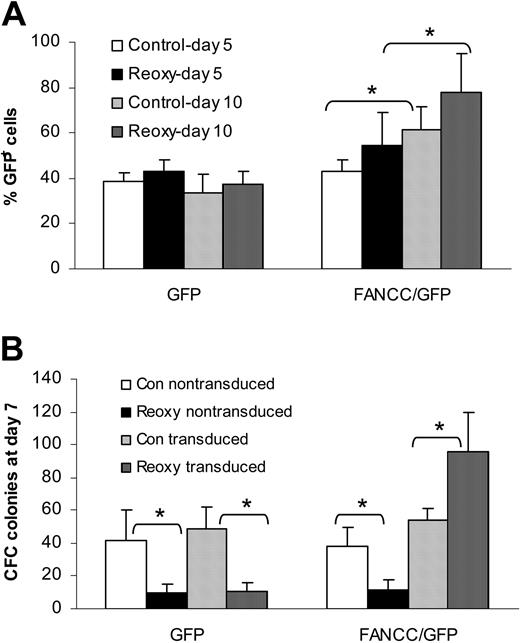
Expansion of FANCC-expressing BM lin– cells exposed to hyperoxic-hypoxic-hyperoxic treatment. (A) Proportions of transduced (GFP+) cells in GFP and FANCC/GFP cultures. The increase in GFP+ cells in the FANCC/GFP culture reflects a growth advantage conferred by FANCC expression. Data are the mean ± SD of triplicate determinations. *Statistical significance between day 5 and day 10 samples at P < .05. (B) Growth of clonogenic progenitors (CFC) of nontransduced and transduced Fancc–/– BM lin– cells. Note that while the proportion of GFP+ CFCs decreased in reoxygenated GFP culture, the GFP+ CFCs were dramatically increased in the FANCC/GFP culture. Data are the mean ± SD of triplicate determinations. *Statistical significance between untreated (Con) and treated (Reoxy) samples at P < .01.
Expansion of FANCC-expressing BM lin– cells exposed to hyperoxic-hypoxic-hyperoxic treatment. (A) Proportions of transduced (GFP+) cells in GFP and FANCC/GFP cultures. The increase in GFP+ cells in the FANCC/GFP culture reflects a growth advantage conferred by FANCC expression. Data are the mean ± SD of triplicate determinations. *Statistical significance between day 5 and day 10 samples at P < .05. (B) Growth of clonogenic progenitors (CFC) of nontransduced and transduced Fancc–/– BM lin– cells. Note that while the proportion of GFP+ CFCs decreased in reoxygenated GFP culture, the GFP+ CFCs were dramatically increased in the FANCC/GFP culture. Data are the mean ± SD of triplicate determinations. *Statistical significance between untreated (Con) and treated (Reoxy) samples at P < .01.
We next wished to determine whether the FANCC protein plays a role in stress response of BM progenitor cells to hyperoxic-hypoxic-hyperoxic treatments. To this end, Lin– BM cells were isolated from Fancc–/– mice, grown for 2 days in the presence of serum and hematopoietic cytokines, and infected with retroviruses expressing either enhanced green fluorescent protein (eGFP) alone (vector group) or both FANCC and eGFP (FANCC group). Infected BM cells were either untreated or subjected to 2 cycles of hyperoxic-hypoxic-hyperoxic treatments. Growth of GFP+ cells and clonogenic progenitors was measured by culturing the transduced Lin– BM cells in liquid or semisolid methylcellulose medium. During the 10-day period, the content of GFP+ cells in vector group (cells transduced with vector alone) remained steady at approximately 40% regardless of treatments (Figure 2A), which was close to initial transduction efficiency of 42%. In contrast, in the FANCC group (34% transduction efficiency) expression of FANCC exhibited a significant growth advantage to total cells, particularly in reoxygenated cultures where nearly 80% of the cells expressed the FANCC protein at day 10 (Figure 2A). Similarly, analysis of the clonogenic activity of the transduced Fancc–/– Lin– BM cells after 10 days of culture (lineage-committed progenitors) demonstrated that while expression of FANCC increased the number of clonogenic progenitors (CFC) in untreated cultures (Figure 2B), the predominance of GFP+ progenitors was observed only in the FANCC group that had been subjected to 2 cycles of hyperoxic-hypoxic-hyperoxic treatments. Taken together, these results indicate a selective expansion of FANCC-expressing progenitor cells, suggesting that loss of FA function renders BM progenitors hypersensitive to reoxygenation stress.
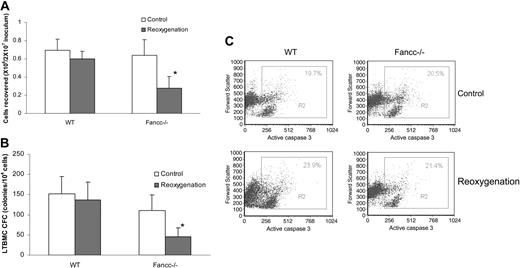
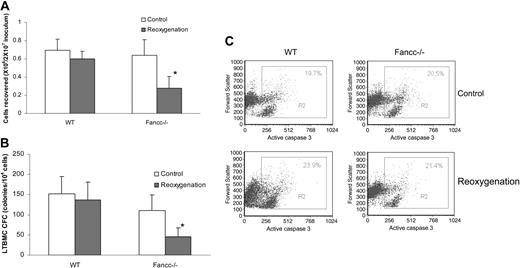
Hyperoxic-hypoxic-hyperoxic treatment inhibits Fancc–/– BM cell hematopoietic function via induction of cell-cycle arrest
Because Fancc–/– BM cells did not undergo further apoptosis but did stop expanding after 24 hours following hyperoxic-hypoxic-hyperoxic treatments, we used LTBMC to determine whether hyperoxic-hypoxic-hyperoxic treatments inhibited Fancc–/– BM cell expansion through additional mechanisms. The stromal cell–supported LTBMC provides a unique approach for the study of the regulation and maintenance of primitive hematopoietic cells, such as HSCs and progenitors, under conditions that reproduce many aspects of the marrow microenvironment.53 An equal number (2 × 107) of WT or Fancc–/– BMMNCs were treated with 2 cycles of hyperoxic-hypoxic-hyperoxic treatments or left untreated, and then grown on preformed FBMD-1 stromal layers in hyperoxia. After a 2-week culture, the recovery of viable WT LTBMC cells was not affected by hyperoxic-hypoxic-hyperoxic treatments (Figure 3A). In Fancc–/– LTBMCs, the number of viable cells recovered from untreated culture was not significantly different from that of WT LTBMC BM cells cultured under the same condition. However, a more than 2-fold decrease in recovery was observed in reoxygenated Fancc–/– LTBMC (Figure 3A). We next evaluated the effect of hyperoxic-hypoxic-hyperoxic treatments on hematopoietic function of the Fancc–/– LTBMC cells using a clonogenic assay (Figure 3B). While hyperoxic-hypoxic-hyperoxic treatments did not inhibit colony formation of WT LTBMCs, reoxygenated Fancc–/– LTBMCs exhibited diminished clonogenic ability (2.4-fold fewer colonies than untreated Fancc–/– LTBMCs). The decrease in survival of LTBMCs suggests that the Fancc–/– BM cells might have undergone apoptosis or/and cell-cycle arrest in response to the stress generated by reoxygenation.
We therefore evaluated the apoptotic profile and cell cycle of these LTBMC cells. To our surprise, hyperoxic-hypoxic-hyperoxic treatments failed to induce more apoptosis in both WT and Fancc–/– LTBMC cells (Figure 3C). This lack of apoptotic effect led us to analyze the cell cycle of the WT and Fancc–/– LTBMC cells after 2 weeks of stroma-supported culture. Less than 30% of reoxygenated Fancc–/– LTBMC cells were found in S and G2/M phases compared with 46.4% in untreated cultures (Table 2). Thus, the slower rate of expansion of Fancc–/– BM cells following 2 cycles of hyperoxic-hypoxic-hyperoxic treatments might have been at least in part due to decreased cell divisions. We also found that a vast majority (70.6%) of reoxygenated Fancc–/– LTBMC cells was residing in the G0 and G1 phases compared with 54.6% in untreated cultures, suggesting that most reoxygenated Fancc–/– LTBMC cells were resting and/or underwent G0/G1 arrest.
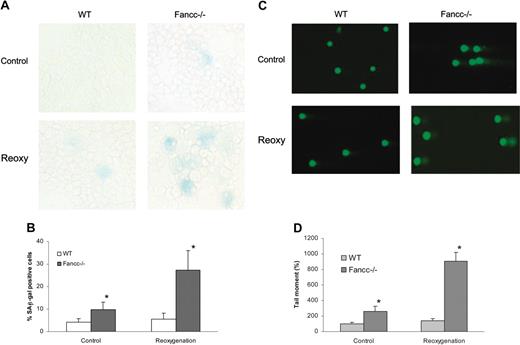
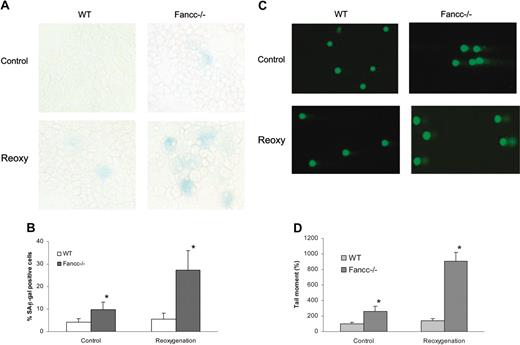
Hyperoxic-hypoxic-hyperoxic treatment induces expression of SA-β-gal and accumulation of DNA damage in Fancc–/– BM cells
Because slower expansion of reoxygenated Fancc–/– LTBMC cells was apparently due to mechanism(s) in addition to apoptosis, we reasoned that these mutant BM cells might have undergone senescence. To examine this possibility, we determined the 2-week LTBMC cells for the activity of SA-β-gal, a biomarker for senescence.54 There was no SA-β-gal staining in the 2-week–cultured WT LTBMC cells, regardless of culture conditions (Figure 4A-B). Similarly, no significant SA-β-gal activity was detected in untreated Fancc–/– BM cells. However, reoxygenated Fancc–/– LTBMC cells stained intensely for SA-β-gal activity. Morphologically, these SA-β-gal–positive Fancc–/– LTBMC cells showed enlarged and flat, characteristic of senescence. This result indicates that hyperoxic-hypoxic-hyperoxic treatments can induce senescence of Fancc–/– LTBMC cells only after 2 weeks of in vitro culture.
Effects of hypoxia-reoxygenation on LTBMC. (A) LTBMC was established for BM cells that were untreated (Control) or exposed to 2 cycles of hyperoxic-hypoxic-hyperoxic treatment (reoxygenation). Viable cells harvested from LTBMC after 2 weeks of culture were counted and presented as mean of 3 independent experiments. *Statistical significance between reoxygenated WT and Fancc–/– samples at P < .01. (B) Effect of reoxygenation on LTBMC progenitor activity. The colony-forming cell (CFC) activity of WT and Fancc–/– LTBMC cells was evaluated after hyperoxia (Control) only or 2 cycles of hyperoxic-hypoxic-hyperoxic treatment (Reoxygenation). Data shown represented the total number of colonies (mean ± SD) from 3 independent experiments. *Statistical significance between reoxygenated WT and Fancc–/– samples at P < .01. (C) Analysis of apoptosis in WT and Fancc–/– LTBMC cells by quantification of the fraction of cells containing activated caspase 3 (gated in R3). Shown are representative flow cytometric presentations of 3 independent experiments.
Effects of hypoxia-reoxygenation on LTBMC. (A) LTBMC was established for BM cells that were untreated (Control) or exposed to 2 cycles of hyperoxic-hypoxic-hyperoxic treatment (reoxygenation). Viable cells harvested from LTBMC after 2 weeks of culture were counted and presented as mean of 3 independent experiments. *Statistical significance between reoxygenated WT and Fancc–/– samples at P < .01. (B) Effect of reoxygenation on LTBMC progenitor activity. The colony-forming cell (CFC) activity of WT and Fancc–/– LTBMC cells was evaluated after hyperoxia (Control) only or 2 cycles of hyperoxic-hypoxic-hyperoxic treatment (Reoxygenation). Data shown represented the total number of colonies (mean ± SD) from 3 independent experiments. *Statistical significance between reoxygenated WT and Fancc–/– samples at P < .01. (C) Analysis of apoptosis in WT and Fancc–/– LTBMC cells by quantification of the fraction of cells containing activated caspase 3 (gated in R3). Shown are representative flow cytometric presentations of 3 independent experiments.
It is known that oxidative stresses that induce growth arrest induce DNA damage.13,23,24 To determine whether hyperoxic-hypoxic-hyperoxic treatments induced DNA damage in the Fancc–/– LTBMC cells that appear to have undergone G0/G1 arrest (Table 2), we examined these BM cells with the comet assay.55,56 This assay measures DNA breakage including single- and double-strand DNA breaks through an increase in the mobility of denatured genomic DNA in single-cell electrophoresis (Figure 4C). The relative amount of damage can be quantified by measuring the distance DNA moves in an agarose gel or the length of the comet tail.56 As shown in Figure 4D, there was no significant accumulation of DNA damage in untreated or reoxygenated WT LTBMC cells, indicating that either 2-cycle hyperoxic-hypoxic-hyperoxic treatments have a very limited effect on WT BM cells or DNA damage induced by reoxygenation-generated oxidative stress had been mostly repaired in these WT BM cells. Strikingly, reoxygenated Fancc–/– LTBMC cells induced significantly (6.4-fold) more DNA strand breakage than reoxygenated WT LTBMC cells (Figure 4D). Interestingly, untreated Fancc–/– LTBMC cells cultured in hyperoxia (21% O2) for 2 weeks accumulated more than 2-fold more DNA damage than did WT LTBMC cells grown in the same oxygen tension. Taken together, hypoxia-reoxygenation represents a physiologically relevant stress for the Fancc–/– BM hematopoietic cells, which induces premature senescence of BM progenitor and stem cells, possibly in a DNA damage–dependent manner.
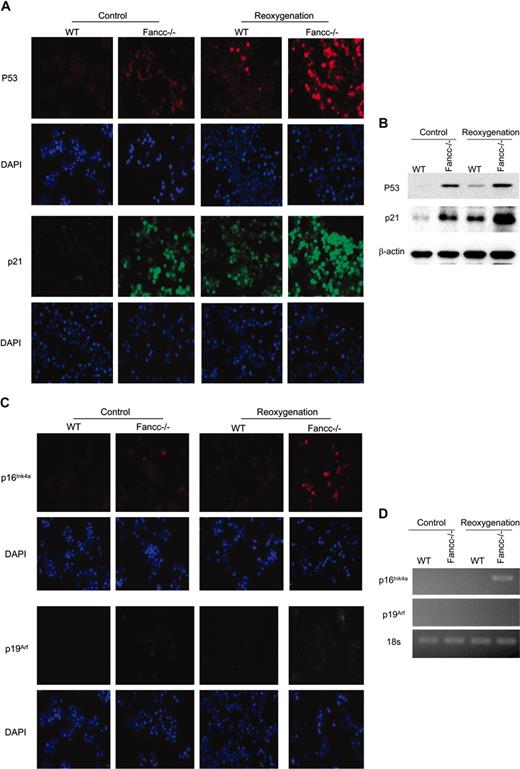
Induction of senescence-associated proteins in long-term cultures of Fancc–/– BM hematopoietic cells
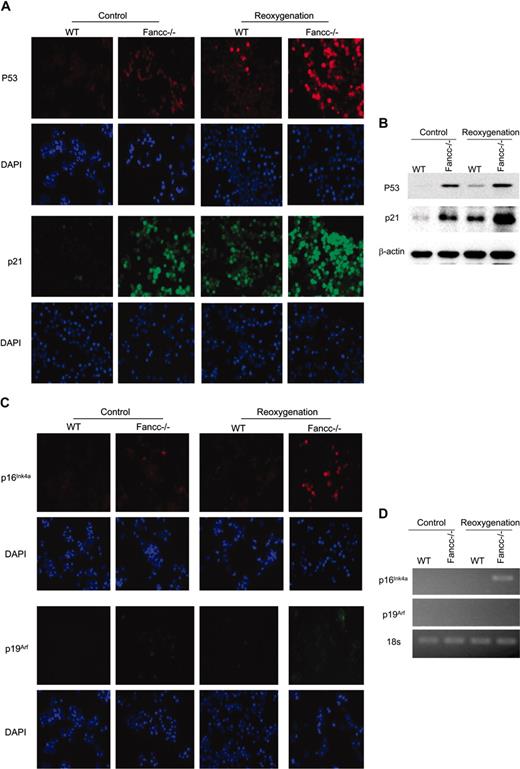
To investigate the molecular mechanism of premature senescence induction by hypoxia-reoxygenation, we examined the expression of senescence-associated proteins in WT and Fancc–/– LTBMC cells. Expression of p53, p21WAF1, p16INK4A, and p19Arf has been known to be increased in senescent cells.57-59 Indeed, we found that more than 50% of the 2-week–cultured reoxygenated Fancc–/– LTBMC cells were stained positive for p53, significantly higher than either parallel untreated Fancc–/– cultures (∼ 20%) or reoxygenated WT LTBMC cells (< 10%). No p53 protein was detected in untreated WT LTBMC cells (Figure 5A). The accumulation of p21WAF1 was also observed in reoxygenated Fancc–/– LTBMC cells (Figure 5A). This was confirmed by Western blot analysis of the levels of p53 and p21 proteins in these LTBMC cells (Figure 5B). Furthermore, the accumulation of p16INK4A was evident in reoxygenated Fancc–/– LTBMC cells (Figure 5C), albeit to a much lesser extent than that apparent for p53 and p21WAF1. However, both WT and Fancc–/– LTBMC cells did not appear to express p19Arf, even after reoxygenation (Figure 5C). To confirm the immunostaining results, we performed RT-PCR to determine mRNA levels of these senescence-associated components. Indeed, the expression of p16Ink4a was increased in reoxygenated Fancc–/– LTBMC cells; whereas p19Arf mRNAs were not detected in any of the groups tested (Figure 5D). The higher expression of p53 and p21WAF1 in reoxygenated Fancc–/– LTBMC cells is likely due to accumulation of DNA damage (Figure 4B), which would subsequently induce p53 and p21WAF1. Thus, these results suggest that stress-induced premature senescence in reoxygenated Fancc–/– BM hematopoietic cells is associated with up-regulation of p53, p21WAF1, and to a lesser degree, p16Ink4a.
Reoxygenation-induced premature senescence in Fancc–/– BM cells. (A) Reoxygenated Fancc–/– LTBMC cells exhibited increased SA-β-gal activity. The hematopoietic cells harvested from a 2-week LTBMC were stained for SA-β-gal activity. (B) The percentage of the cells stained positive for SA-β-gal was quantified by counting a total of 1000 cells in random fields on a slide. The data represent the mean ± SD. *Statistical significance between reoxygenated WT and Fancc–/– samples at P < .05. (C) Reoxygenated Fancc–/– LTBMC cells accumulated high levels of oxidative DNA damage. DNA strand breaks were analyzed by a single-cell gel electrophoresis (comet) assay, in which nuclei and comet images visualized by SYBR Green staining. Shown are representative images of the comet assays. (D) DNA damage quantified by determining the comet tail movement (increasing values represent increasing amounts of DNA damage). The mean tail moment of the WT without treatment (Control) is expressed as 100%. For each treatment, 30 cells were scored for tail moment from random sampling. Data reflect means ± SD of 3 independent experiments performed. *Statistical significance between reoxygenated WT and Fancc–/– samples at P < .05.
Reoxygenation-induced premature senescence in Fancc–/– BM cells. (A) Reoxygenated Fancc–/– LTBMC cells exhibited increased SA-β-gal activity. The hematopoietic cells harvested from a 2-week LTBMC were stained for SA-β-gal activity. (B) The percentage of the cells stained positive for SA-β-gal was quantified by counting a total of 1000 cells in random fields on a slide. The data represent the mean ± SD. *Statistical significance between reoxygenated WT and Fancc–/– samples at P < .05. (C) Reoxygenated Fancc–/– LTBMC cells accumulated high levels of oxidative DNA damage. DNA strand breaks were analyzed by a single-cell gel electrophoresis (comet) assay, in which nuclei and comet images visualized by SYBR Green staining. Shown are representative images of the comet assays. (D) DNA damage quantified by determining the comet tail movement (increasing values represent increasing amounts of DNA damage). The mean tail moment of the WT without treatment (Control) is expressed as 100%. For each treatment, 30 cells were scored for tail moment from random sampling. Data reflect means ± SD of 3 independent experiments performed. *Statistical significance between reoxygenated WT and Fancc–/– samples at P < .05.
Discussion
Because the cellular mechanism by which the dysfunction of HSCs leads to BM failure diseases has not been established, we attempted to characterize the effects of physiologically relevant hypoxia-reoxygenation on the survival and expansion of FA BM hematopoietic progenitor and stem cells. The results represented here demonstrated that expansion of Fancc–/– BM cells enriched for progenitor and stem cells was significantly decreased after 2 continuous cycles of hyperoxic-hypoxic-hyperoxic treatments, compared with WT BM cells under the same conditions. This inhibition was attributable to a marked decrease of Fancc–/– ScaI– c-kit+ cells, as well as a slower expansion of Fancc–/– ScaI+ c-kit+ cells than the WT BM cells during a short-term liquid culture following reoxygenation. With respect to the maintenance of progenitor activity, WT and Fancc–/– BM progenitors responded differently to the stress generated by hyperoxic-hypoxic-hyperoxic treatments. Reoxygenated WT BM progenitors gave rise to higher BFU-E but lower CFU-GM colonies, albeit not statistically significantly, than untreated WT progenitors (Figure 1E). However, reoxygenated Fancc–/– BM progenitors produced significantly lower amounts of both BFU-E and CFU-GM colonies compared with untreated Fancc–/– BM progenitors. These findings suggest that FA BM progenitors are hypersensitive to oxidative stress generated by 2 continuous cycles of hyperoxic-hypoxic-hyperoxic treatments.
An extensive body of evidence has demonstrated that the FA proteins play important roles in cellular responses to oxidative stress. For example, the FANCC protein has been found to interact with nicotinamide adenine dinucleotide phosphate (NADPH) cytochrome P450 reductase and glutathione S-transferase P1-1,41,42 2 enzymes involved in either triggering or detoxifying reactive intermediates, including ROSs. In addition, mice with combined deficiencies of the antioxidative enzyme, Cu/Zn superoxide dismutase, and Fancc genes demonstrated a defective hematopoiesis.43 Another FA protein, FANCG, interacts with cytochrome P450 2E1, a member of the P450 superfamily that is associated with the production of reactive oxygen intermediates, suggesting a possible role of FANCG in protection against oxidative DNA damage.44 More recently, Saadatzadeh et al45 showed that oxidant hypersensitivity of Fancc–/– cells was due to an altered redox regulation and ASK1 hyperactivation. Moreover, oxidative stress induces complex formation by 2 major FA proteins, FANCA and FANCG.46 Our present finding that reoxygenation-generated oxidative stress induces premature cell senescence in Fancc–/– BM cells corroborates a critical role for oxidative stress in FA phenotype and disease progression.
Hypoxia-reoxygenation increases expression of senescence-associated proteins. (A) Reoxygenated Fancc–/– LTBMC cells showed strong immunostaining for p53 and p21Waf1. The hematopoietic cells harvested from a 2-week LTBMC were stained with the antibodies against p53 and p21Waf1 and then counterstained with DAPI. Representative photomicrographs of p53 and p21Waf1 immunofluorescent staining are shown. (B) Expression of p53 and p21Waf1 as analyzed by immunoblotting. Equal loading was ensured by reprobing the blot with antibody for β-actin. (C) Reoxygenated Fancc–/– LTBMC cells increased moderately the accumulation of p16Ink4a, but not p19Arf. The hematopoietic cells harvested from a 2-week LTBMC were stained with the antibodies against p16Ink4a and p19Arf. (D) Expression of p16Ink4a and p19Arf in WT and Fancc–/– LTBMC cells, as analyzed by RT-PCR.
Hypoxia-reoxygenation increases expression of senescence-associated proteins. (A) Reoxygenated Fancc–/– LTBMC cells showed strong immunostaining for p53 and p21Waf1. The hematopoietic cells harvested from a 2-week LTBMC were stained with the antibodies against p53 and p21Waf1 and then counterstained with DAPI. Representative photomicrographs of p53 and p21Waf1 immunofluorescent staining are shown. (B) Expression of p53 and p21Waf1 as analyzed by immunoblotting. Equal loading was ensured by reprobing the blot with antibody for β-actin. (C) Reoxygenated Fancc–/– LTBMC cells increased moderately the accumulation of p16Ink4a, but not p19Arf. The hematopoietic cells harvested from a 2-week LTBMC were stained with the antibodies against p16Ink4a and p19Arf. (D) Expression of p16Ink4a and p19Arf in WT and Fancc–/– LTBMC cells, as analyzed by RT-PCR.
To evaluate the role of the FANCC protein in response of BM progenitor cells to reoxygenated stress, we expressed the human FANCC protein in Fancc–/– Lin– BM cells and found that Fancc–/– BM cells enriched for progenitors transduced with FANCC retroviruses exhibited a significant growth advantage to untransduced cells in both the short-term liquid culture and clonogenic assays (Figure 2). This growth predominance was particularly evident in hyperoxic-hypoxic-hyperoxic conditions where the growth of Fancc–/– BM cells transduced with the control retroviruses was severely suppressed. The role of FANCC protein in the response of BM cells to reoxygenation-generated stress remains unclear at this time. Forced expression of FANCC did not further increase the level of the HIF-1α protein (data not shown), which is a transcriptional activator of genes encoding for a variety of survival factors including erythropoietin and VEGF.60-62 The FANCC protein has been shown to function in signaling pathways involving stress response. A special or perhaps central role of FANCC in hematopoietic cell survival signaling would be anticipated from work of many laboratories on the function of FANCC that has established a consistent signaling abnormality in hematopoietic cells bearing FANCC mutations. It has been shown that suppression of FANCC expression represses clonal growth of normal erythroid and granulocyte-macrophage progenitor cells and disruption of the Fancc gene, in mice, renders hematopoietic progenitor cells hypersensitive to the proapoptotic effect of interferon γ (IFN-γ) and tumor necrosis factor α (TNF-α).26,40,50,63,64 The multifunctional property of the FANCC protein appears to explain the clinical observations that patients in complementation group C had a significantly more severe phenotype than other complementation groups.65 However, whether FANCC functions to prevent hematopoietic progenitor and stem cells from premature senescence remains to be elucidated.
To investigate the mechanism underlying growth suppression of Fancc–/– BM cells enriched for progenitors induced by hyperoxic-hypoxic-hyperoxic treatments, we evaluated the apoptotic profile and cell cycle of LTBMC. We found that reoxygenation induced modest levels of apoptosis in WT and Fancc–/– LTBMC cells after a 2-week culture following hyperoxic-hypoxic-hyperoxic treatments (Figure 3C). Significantly, a vast majority (70.6%) of reoxygenated Fancc–/– LTBMC cells was residing in the G0 and G1 phases compared with 54.6% in untreated cells (Table 2). This observation suggests that reoxygenated Fancc–/– BM hematopoietic cells underwent G0/G1 arrest and probably became senescent. Induction of G1 arrest by hypoxia has been reported in tumor2,66 and endothelial cells.67 In fibroblasts, hypoxia can inhibit the G1/S transition through up-regulation of p27 expression.5 It should be noted that hyperoxic-hypoxic-hyperoxic treatments did result in a significant increase of apoptosis in Fancc–/– cells during the first 8 hours after treatment (Figure 1D), suggesting that apoptosis plays a role in the reduced expansion of Fancc–/– cells during the first hours following hyperoxic-hypoxic-hyperoxic treatments. It is possible that oxidative stress generated by the hyperoxic-hypoxic-hyperoxic treatments may have induced different levels of injury among individual cells. Since Fancc–/– cells are more vulnerable to oxidative stress–induced DNA damage than WT cells are, possibly due to a defect in DNA damage repair, it is not surprising that more Fancc–/– cells contain high levels of DNA damage and undergo apoptosis shortly after treatments. However, a substantial portion of Fancc–/– cells may also contain lower levels of DNA damage that do not reach the threshold of apoptosis but would otherwise have been repaired in the WT cells. These Fancc–/– cells may have survived and undergone permanent growth arrest (senescence). Therefore, the growth inhibition induced by hyperoxic-hypoxic-hyperoxic treatments we observed in Fancc–/– BM hematopoietic cells may have been via both apoptosis-dependent and -independent mechanisms.
That reoxygenated stress does not further induce apoptosis in Fancc–/– BM cells (compared with their WT counterparts under the same stress) enriched for progenitors and stem cells is a novel and unexpected finding, because previous studies showed that Fancc–/– BM progenitors and stem cells are extremely vulnerable to apoptotic death when exposed to a variety of stresses.26,40,50,63,64 However, we found substantial accumulation of DNA damage in the Fancc–/– BM hematopoietic cells in LTBMCs following reoxygenation (Figure 4C-D). Strikingly, reoxygenated Fancc–/– LTBMC cells stained intensely for SA-β-gal activity (Figure 4A-B) and increased the expression of senescence-associated proteins p53 and p21WAF1 (Figure 5). Surprisingly, we found that while there was some degree of p16INK4A elevation, p19Arf was not expressed in these senescent Fancc–/– BM hematopoietic cells. Up-regulation of p16INK4A and p19Arf expression have been implicated in induction and maintenance of permanent cell-cycle arrest through inhibition of cyclin-dependent kinases and activation of p53/p21 pathway, respectively.68-70 Therefore, our data suggest that up-regulation of p53 and p21 in senescent Fancc–/– BM hematopoietic cells may involve an upstream signaling transducer other than p16INK4A or p19Arf. Nevertheless, these results suggest that reoxygenation induces premature senescence in Fancc–/– BM hematopoietic cells by signaling through p53, up-regulating p21, and causing senescent cell-cycle arrest.
In conclusion, we showed that continuous cycles of hyperoxic-hypoxic-hyperoxic treatments, a condition that is physiologically relevant, inhibit hematopoietic function of Fancc–/– BM cells enriched for progenitors and stem cells. We also demonstrated that these Fancc–/– BM cells underwent premature senescence after exposure to cycles of hyperoxic-hypoxic-hyperoxic treatments. The induction of premature senescence may in part be responsible for the observed inhibition of Fancc–/– BM hematopoietic function by hyperoxic-hypoxic-hyperoxic treatments. Senescence, together with apoptosis, may constitute a major mechanism of hematopoietic cell depletion, which occurs in BM failure diseases. Therefore, our study suggests that stress-induced premature senescence triggered by hypoxia-reoxygenation may be a novel mechanism underlying BM failure in FA.
Prepublished online as Blood First Edition Paper, March 15, 2005; DOI 10.1182/blood-2004-08-3033.
Supported by a Fanconi Anemia Research Fund grant, an American Cancer Society (Ohio Division) Support grant, and a Trustee grant from the Cincinnati Children's Hospital Medical Center to Q.P.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank Dr Manuel Buchwald (Hospital for Sick Children, University of Toronto) for the Fancc–/– mice, and Dr Yi Zheng (Cincinnati Children's Hospital Medical Center) for reagents and helpful discussion. Q.P. thanks Dr Grover Bagby (Oregon Health Science University) for continued support.