Abstract
Although recent data suggests that osteoblasts play a key role within the hematopoietic stem cell (HSC) niche, the mechanisms underpinning this remain to be fully defined. The studies described herein examine the role in hematopoiesis of Osteopontin (Opn), a multidomain, phosphorylated glycoprotein, synthesized by osteoblasts, with well-described roles in cell adhesion, inflammatory responses, angiogenesis, and tumor metastasis. We demonstrate a previously unrecognized critical role for Opn in regulation of the physical location and proliferation of HSCs. Within marrow, Opn expression is restricted to the endosteal bone surface and contributes to HSC transmarrow migration toward the endosteal region, as demonstrated by the markedly aberrant distribution of HSCs in Opn–/– mice after transplantation. Primitive hematopoietic cells demonstrate specific adhesion to Opn in vitro via β1 integrin. Furthermore, exogenous Opn potently suppresses the proliferation of primitive HPCs in vitro, the physiologic relevance of which is demonstrated by the markedly enhanced cycling of HSC in Opn–/– mice. These data therefore provide strong evidence that Opn is an important component of the HSC niche which participates in HSC location and as a physiologic-negative regulator of HSC proliferation.
Introduction
Hematopoietic stem cell (HSC) engraftment is a multistep process, involving homing, transmarrow migration (TMM), and lodgment within a bone marrow (BM) niche. Homing is the specific recruitment of HSCs to the BM and involves the recognition of HSCs by the BM microvascular endothelium and transendothelial cell migration into the hematopoietic space. Lodgment is defined as the selective migration of HSCs to a suitable niche within the extravascular compartment. In comparison to homing, very little is known about molecules that regulate HSC lodgment and, moreover, the retention of HSCs within these distinct anatomical locations.
In accord with the stem cell niche model proposed by Schofield,1 recent studies within our laboratory demonstrate that HSCs actively migrate toward and reside within the endosteal region at the bone and BM interface.2,3 This concept is supported by studies reported by Calvi et al,4 Zhang et al,5 and Arai et al,6 which highlight the importance of direct contact and interactions between HSCs and osteoblasts at the endosteal surface in the regulation of HSC proliferation. Further evidence that osteoblasts directly regulate hematopoiesis is provided by studies in which conditional ablation of osteoblasts results in significant reduction of marrow hematopoiesis,7 although the factors responsible for this profound effect remain to be determined. In addition, in vitro evidence indicates that osteoblastic cells can expand HSC numbers8 and, when cotransplanted with HSCs, can improve engraftment.9 Collectively, these findings suggest that osteoblasts are a key cell type within the HSC niche and that molecules expressed by these cells may have previously unrecognized roles in regulating hematopoiesis.
One molecule that shows high levels of expression in osteoblasts cells lining bone trabeculae is Osteopontin (Opn),10 an observation that is not unexpected given its well-described role as a key regulator of bone homeostasis.11 Opn is a multidomain, phosphorylated glycoprotein synthesized by many cell types and involved in many physiologic and pathologic processes, including cell adhesion,12 angiogenesis,13 apoptosis, inflammatory responses, and tumor metastasis.14 Physiologically, phosphorylation, glycosylation, and cleavage of Opn result in molecular mass variants, ranging from 25 to 75 kDa. The different effects that Opn elicit are attributable to its multiple receptors, binding sites, and its various forms.15 One of the major serine proteases to cleave Opn is thrombin, giving rise to a 24-kDa and a 45-kDa fragment. The 45-kDa fragment has multiple functional advantages in processes such as cell attachment, migration, and spreading through binding to α9β1 and α4β1.16,17
Opn is bound by multiple integrins, including αvβ3,18 α9β1,17 αvβ5,19 αvβ1,19 α4β1,16 α5β1,20 and α4β7.21 In addition, there is evidence that CD44 can also bind Opn22 possibly via the v6 and v7 variants.23 These receptors mediate the adhesion of a broad range of cell types to Opn, which results in distinct cellular functions. For example, αvβ3 and αvβ1 mediate adhesion of smooth muscle cells, but only αvβ3 is involved in cell migration.24 Although several of these integrins, including α4β1,25,26 α4β7,27 and various isoforms of CD44, are expressed on HSCs (reviewed by Simmons et al28 ), to date no studies have investigated the adhesion of primitive hematopoietic cells to Opn.
Herein, we investigate the potential role of Opn in HSC lodgment and hematopoiesis. We demonstrate that Opn exhibits a highly restricted pattern of expression at the endosteal surface and contributes to HSC TMM toward the endosteal region after transplantation. In accord with this, primitive hematopoietic cells demonstrate specific adhesion to Opn in vitro that involves β1 integrins. Experiments using Opn–/– mice demonstrate markedly enhanced cycling of HSCs, consistent with a physiologic role for Opn as a negative regulator of HSC proliferation. In accord with this hypothesis, we demonstrate that exogenous Opn suppresses the proliferation of primitive HPCs in vitro when cultured in a potent combination of early-acting synergistic growth factors, a phenomenon that is not due to the induction of apoptosis. Furthermore, we show that the BM of Opn–/– mice has increased cellularity and an associated significant increase in levels of lineage-negative (Lin–), stem cell antigen-1–positive (Sca-1+), c-kit receptor–positive (Kit+) (LSK) cells in vivo. Collectively, our data provide strong evidence that Opn is an as yet unrecognized component of endosteally located stem cell niches with an important physiologic role in the regulation of HSC location and proliferation.
Materials and methods
Umbilical cord blood (CB)
CB was obtained from the Mercy Hospital for Women (East Melbourne, Victoria, Australia) in accordance with procedures approved by the human ethics committee of the Mercy Hospital. Samples were collected into sodium citrate and held at room temperature until processed.
Mice
Osteopontin-null (Opn–/–)29 and wild-type (wt) mice were bred at Peter MacCallum Cancer Centre. C57Bl/6J mice were purchased from Animal Resources Centre (Perth, Western Australia, Australia) and housed for at least a week prior to experimental use.
Isolation of murine HSCs
Mice were killed by cervical dislocation, and BM was collected from femurs, tibiae, and iliac crests. Low-density cells (< 1.077g/cm3) were isolated by discontinuous density centrifugation using Nycoprep for animals (Accurate Chemical and Scientific, Westbury, NY), and lin– cells were separated as previously described.3 Briefly, cells were labeled with a cocktail of biotinylated rat antimouse antibodies: B220, macrophage antigen-1 (Mac-1), Gr-1, CD4, CD8, CD3, CD5, and Ter119. Lin+ cells were removed by immunomagnetic selection using magnetic-activated cell separation (MACS; Miltenyi Biotec, Bergisch, Gladbach, Germany).
Lin– cells were labeled with Sca-1–fluorescein isothiocyanate (Sca-1–FITC; 1 μg/5 × 106 cells; Pharmingen, San Diego, CA), c-kit–phycoerythrin (PE; 1 μg/5 × 106 cells; Pharmingen), and streptavidin–Red 670 (1/160 final concentration; Gibco, Grand Island, NY). LSK cells were isolated by fluorescence-activated cell sorting (FACS).
Enrichment of human progenitor cells
Low-density BM cells were isolated from CB by discontinuous density centrifugation using Ficoll-Hypaque (1.077 g/mL; Pharmacia Biotech, Uppsala, Sweden). A variation of the Dynal bead method for clinical scale selection of cells using the Isolex 300i (Miltenyi Biotech, Bergisch, Germany) was used for isolation of CD34+ cells.30 CB mononuclear cells were incubated with anti-CD34, washed, and exposed to Dynal anti–mouse immunoglobulin G (IgG) beads to rosette CD34+ cells. CD34+ cells were captured and incubated with peptide release agent to isolate CD34+ cells. Cells were immunolabeled with a cocktail of CD34-FITC and CD38-PE (Becton Dickinson, Franklin Lakes, NJ) for subsequent isolation of CD34+, CD34+CD38–, and CD34+CD38+ cells by FACS.
Adhesion assay
Cell adhesion assays were performed to examine the ability of HSCs to specifically bind to Opn. Microplates were coated overnight at 4°C with a fusion protein comprising full-length human Opn fused at the N-terminus with glutathione S-transferase (GST; Auspep, Parkville, Victoria, Australia), at a concentration of 20 μg/mL in Tris (tris(hydroxymethyl)aminomethane)–buffered saline (TBS; 25 mM Tris-HCl, 150 mM NaCl, pH 7.2). Unbound Opn was removed by washing, and wells were blocked with Iscove modified Dulbecco medium (Gibco BRL) supplemented with 1% heat-denatured bovine serum albumin (BSA). Cells for assay were labeled with 10 μM calcein-AM (Molecular Probes, Eugene, OR). To demonstrate specific interaction of CD34+ cells with Opn via β1 integrins, an aliquot of cells was incubated with the function-blocking monoclonal antibody P5D2.31 Cells were allowed to adhere for 30 minutes at 37°C. Unbound cells were removed by gentle washing. Cell adhesion was quantified by lysing adherent cells with 1% sodium dodecyl sulfate and measuring fluorescence using a Molecular Imager FX (Bio-Rad, Hercules, CA). The number of adherent cells was determined by calculating the percentage of fluorescence under each condition compared with the percentage of fluorescence of input cells.
Cell culture
Sorted human cells were cultured in serum-deprived media32 supplemented with human granulocyte colony-stimulating factor (G-CSF), stem cell factor (SCF), Fms-like tyrosine kinase 3 ligand (FLT3-L), megakaryocyte growth and development factor (MGDF) (all 100 ng/mL), interleukin 6 (IL-6), and IL-3 (both 10 ng/mL). Sorted murine cells were cultured in X Vivo 10 medium (BioWhittaker, Walkersville, MD), 0.5% human serum albumin (Buminate; Baxter, Glendale, CA) supplemented with rat SCF (75 ng/mL) and human IL-11, FLT3-L, and IL-6 (all 100 ng/mL). In addition, various doses of intact bovine Opn (R&D Systems, Minneapolis, MN), or thrombin-cleaved bovine Opn (tcOpn) were added. tcOpn was prepared by incubating 24 μg bovine Opn in 20 mM Tris-HCl (pH 7.6), 80 mM NaCl, 2 mM CaCl2, and 0.1 unit thrombin (CSL, Parkville, Victoria, Australia), for 10 minutes at 37°C. Cleavage of Opn was confirmed by Western blot analysis revealing the 2 expected fragments of approximately 28 and 30 kDa. Control cultures were established in the presence of the equivalent volume of buffer and thrombin. As a positive control for growth inhibition, cells were grown in 10 μg/mL biotinylated hyaluronic acid (HA) binding protein (HABP; Seikagaku, Tokyo, Japan).33 All cells were cultured at 37°C in 5% O2, 10% CO2, and 85% N2, before counting and immunophenotyping.
Immunolabeling and flow cytometry
Immunolabeled cells were sorted on a FACStar (Becton Dickinson) as previously described.3 Human cells from in vitro cultures were labeled with CD34-FITC and CD38-PE or with CD15-FITC (Becton Dickinson). Cells were resuspended at 5 × 106 cells/mL with 2 μg/mL 7-amino-actinomycin D (Sigma, St Louis, MO) and analyzed on a FACScan (Becton Dickinson). Data from at least 10 000 viable cells were collected and analyzed by WinMidi software (Scripps Institute, San Diego, CA).
Analysis of apoptosis
The proportion of apoptotic cells was determined by using the In Situ Cell Death Detection Kit (Roche, Indianapolis, IN) as recommended by the manufacturer. The proportion of apoptotic cells was determined by using the FACScan.
5-(and-6)-carboxyfluorescein diacetate succinimidyl ester (CFSE) labeling
Cells to be transplanted for spatial distribution analysis were labeled with CFSE (Molecular Probes) as previously described.3 Cells were transplanted in 0.2 mL phosphate-buffered saline (PBS) by injection into the lateral tail vein.
5-Fluorouracil (5FU) and busulphan
A single dose of 200 mg/kg 5FU was given intravenously 3 days prior to BM analysis for progenitor cell cloning efficiency. Low- and high-proliferative potential colony-forming cells (LPP-CFCs and HPP-CFCs, respectively) were assayed in a double-layer nutrient agar culture system as previously described,34 except that SCF was added to CSF-1, IL-1, and IL-3 to analyze HPP-CFCs. Two doses of 50 mg/kg busulphan were given subcutaneously 1 and 3 days prior to transplanting limiting numbers of wt LSK cells intravenously (10 000, 3000, 1000, and 300).
Bromodeoxyuridine (BrdU)
Wild-type and Opn–/– mice were given BrdU (500 μg/mL) continuously as previously described.35 After 4 weeks, LSK cells were isolated from individual animals as described under “Isolation of murine HSCs.” The proportion of BrdU was determined according to the BrdU in situ detection kit (Becton Dickinson) as described by the manufacturer's instructions.
Transplantation analysis
The spatial distribution of CFSE-positive cells was analyzed 1 and 15 hours after transplantation, as previously described.3 The location of at least 50 CFSE-labeled cells (positive cells) from at least 6 longitudinal sections per individual transplant recipient was recorded, and their location was designated as either endosteal (previously arbitrarily defined as within 12 cells of the endosteum) or central (> 12 cells from either endosteum) (Figure 1).3
Analysis of long-term transplants into wt and Opn–/– microenvironments was done using male donor LSK cells into female recipients. After 3 months, BM was harvested, DNA was isolated, and the proportion of male donor was determined by using real-time polymerase chain reaction (PCR) targeting the same Y6 amplicon on the Y chromosome as previously described,36 except the primers were forward 5′catcctattcagatttctctctctttatca, reverse 5′caaaaggtccaaattcatctaagagtaa, and a 6-carboxyfluorsecein (6FAM)–gttttccaggtttaagtagattctcatt–6-carboxy-tetramethylrhodamine (TAMRA) probe. The autosomal control used was RNA 18s with primers forward 5′-ttggataactgtggtaattctagagctaata, reverse 5′-ccgggttggttttgatctga, and a VIC-atgccgacgggcgctgacc probe.
Immunohistochemical analysis of Opn in BM
Femoral BM was fixed by perfusion, decalcified, and embedded in paraffin as previously described.2 Longitudinal sections (3.5 μm) were cut, dewaxed, brought to water, and incubated in 50 mM glycine in PBS. Sections were incubated in 0.3% Triton X-100 in PBS, washed, and blocked in 5% skim milk, 5% BSA, 0.05% Triton X-100 in 4 × SSC (0.6 M NaCl and 0.06 M sodium citrate, pH 6.4), before labeling with goat anti–mouse Opn (R&D Systems) or goat IgG (R&D Systems) at 2 μg/mL in 0.5% BSA in PBS, washed, followed by rabbit anti–goat IgG-FITC secondary antibody (1/500; Vector Laboratories, Burlingame, CA). Sections were washed in PBS, PBS 0.05% Triton X-100, then PBS prior to mounting in antifade (Vectashield; Vector Laboratories).
Image acquisition and manipulation
Images were acquired on an Olympus BX51 microscope (Olympus Tokyo, Japan) through a 20 ×/0.70 NA UplanApo objective lens using a cooled monochrome CCD Optronics Magnafire S99802 camera at 40°C below ambient and Magnafire software (Optronics, Goleta, CA). Image brightness was adjusted using Adobe Photoshop (Adobe Systems, San Jose, CA).
Statistical analysis
Differences between means were evaluated by one-way analysis of variance (ANOVA) or Student t test where appropriate.
Results
Distribution of Opn in the BM
The anatomical location of Opn within mouse femoral BM was assessed by immunohistochemically staining. As shown in Figure 1, this revealed a highly localized pattern of Opn expression, restricted to the bone and marrow interface. This high and restricted expression of Opn at the endosteum, the putative location for the HSC niche, prompted us to examine what role Opn plays in TMM, lodgment, and the regulation of HSC proliferation and differentiation.
Opn plays a key role in the lodgment and engraftment of transplanted murine HSCs
To investigate the role of Opn in lodgment, HSCs were transplanted into wt or Opn–/– mice, and their spatial distribution was analyzed at short-term time points after transplantation. In accord with previous observations,3 transplantation of LSK cells into a nonmyeloablated, wt microenvironment resulted in TMM to the endosteal region with more than 60% of donor cells evident within this region 15 hours after transplantation (Figure 2A). In marked contrast, transplantations of LSK cells into Opn–/– mice revealed no evidence of TMM to the endosteal region (Figure 2A). In fact, there was evidence of significant migration away from the endosteum within the first 15 hours after transplantation, with a 34% reduction in the number of donor cells present in this region compared with that after 1 hour (P < .005) (Figure 2A). This resulted in an approximate 43% reduction in the proportion of LSK cells located at the endosteum 15 hours after transplantation compared with that detected following a transplantation into a wt microenvironment (P < .01) (Figure 2A) where Opn is expressed at the endosteum. These data therefore suggest a functional role for Opn in the lodgment of HSCs within the endosteal region. This possibility was investigated in studies in which hematopoietic regeneration and survival of myeloablated wt and Opn–/– mice were compared following transplantation with wt LSK BM cells. As shown in Figure 2B, compared with wt mice, Opn–/– recipient animals exhibited an engraftment defect that is consistent with the impaired ability of wt LSK cells to lodge in a hematopoietic microenvironment (HM) devoid of Opn. Impaired engraftment was most evident in recipient mice that received transplants with limiting numbers of LSK cells. Transplantation of 300 to 10 000 wt LSK cells was similarly effective in reestablishing hematopoiesis and enabling wt mice to survive busulphan myeloablation. However, in contrast, transplantation of 1000 and 300 wt LSK cells into myeloablated Opn–/– mice resulted in significantly fewer animals surviving (79% to 64% and 75% to 47%, wt to Opn–/–, respectively). This finding demonstrates the importance of Opn in the HM in supporting limiting numbers of transplanted HSCs.
Immunohistochemical localization of Opn and correlation with CFSE+ donor cells in a longitudinal section of a murine femur. (A) Opn expression was highly restricted to the endosteum of the marrow cavity (dotted arrows) and correlated with the localization of 2 CFSE+ donor LSK cells (solid arrows). (B) Isotype control for Opn expression with 1 CFSE+ donor LSK cell (arrows). Counterstained with DAPI (4′, 6-diamino-2-phenylindole). Bars = 30 μm.
Immunohistochemical localization of Opn and correlation with CFSE+ donor cells in a longitudinal section of a murine femur. (A) Opn expression was highly restricted to the endosteum of the marrow cavity (dotted arrows) and correlated with the localization of 2 CFSE+ donor LSK cells (solid arrows). (B) Isotype control for Opn expression with 1 CFSE+ donor LSK cell (arrows). Counterstained with DAPI (4′, 6-diamino-2-phenylindole). Bars = 30 μm.
Opn plays a key role in the TMM and lodgment of HSCs in the endosteal marrow region and hematopoietic reconstitution. (A) Compared with transplants of HSCs into a wt microenvironment (▦), there was no evidence of TMM toward the endosteal region in an Opn–/– microenvironment (▪). Conversely, there was evidence of significant TMM toward the central region (P < .005), which resulted in significantly fewer cells lodging in the endosteal region 15 hours after transplantation compared with wt controls (P < .01). Data are the mean ± SEM of between 5 and 6 individual mice. (B) Comparison of hematopoietic regeneration and survival out to 3 weeks following myeloablation in wt and Opn–/– mice that received transplants with limiting numbers of wt LSK BM cells (solid bar and ▪ versus open bar and ▴, respectively). Data are the mean of between 12 and 19 recipients from 3 individual experiments.
Opn plays a key role in the TMM and lodgment of HSCs in the endosteal marrow region and hematopoietic reconstitution. (A) Compared with transplants of HSCs into a wt microenvironment (▦), there was no evidence of TMM toward the endosteal region in an Opn–/– microenvironment (▪). Conversely, there was evidence of significant TMM toward the central region (P < .005), which resulted in significantly fewer cells lodging in the endosteal region 15 hours after transplantation compared with wt controls (P < .01). Data are the mean ± SEM of between 5 and 6 individual mice. (B) Comparison of hematopoietic regeneration and survival out to 3 weeks following myeloablation in wt and Opn–/– mice that received transplants with limiting numbers of wt LSK BM cells (solid bar and ▪ versus open bar and ▴, respectively). Data are the mean of between 12 and 19 recipients from 3 individual experiments.
Analysis of the peripheral blood of surviving animals 6 weeks after transplantation revealed no significant differences in the proportion of donor cells in a wt or Opn–/– microenvironment at any of the cell doses transplanted (data not shown). However, analysis of the BM 3 months after transplantation revealed a long-term engraftment defect, with significantly fewer donor cells detected in an Opn–/– microenvironment compared with a wt environment (94% ± 5.8% versus 22% ± 0.9% and 68% ± 6.6% versus 36% ± 3.9% for 300 and 10 000 cells transplanted into a wt and Opn–/– microenvironment, respectively; n = 5 per group; P < .02).
Opn regulates HSC proliferation in vivo
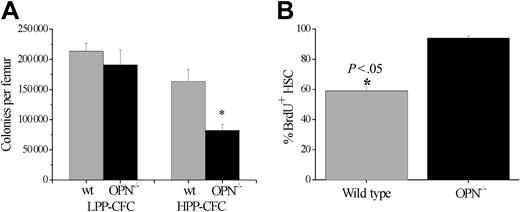
To examine the role of Opn in the regulation of HSC proliferation in vivo, wt and Opn–/– mice were given a single dose of 5FU, and their hematopoietic response was assessed by quantitation of HPCs within the BM after 3 days. There was no difference in the proportion or absolute number of mature, LPP-CFCs in the BM at day 3 after 5FU in Opn–/– mice compared with wt controls (Figure 3A). In contrast, there was a 50% decrease in the number of HPP-CFCs in Opn–/– mice compared with wt controls at the same time point (Figure 3A), suggesting that in the absence of Opn a greater proportion of primitive HPCs are in cycle. To analyze this further, Opn–/– and wt mice were given BrdU continuously for 4 weeks,35 after which LSK cells were isolated and their uptake of BrdU was analyzed by immunohistochemical staining. In wt mice approximately 60% of HSCs were BrdU+, while, in the corresponding LSK population isolated from Opn–/– mice, 100% of cells had incorporated BrdU (Figure 3B). These data confirm that in the absence of Opn essentially all cells within the LSK population divide within 4 weeks, suggesting that Opn inhibits HSC proliferation in vivo. To further investigate the effect of Opn on in vivo hematopoiesis, BM cellularity and primitive HPC content were assessed in Opn–/– and wt mice in the steady state. As shown in Figure 4A, BM cellularity was significantly increased in Opn–/– compared with wt mice (78 ± 2.3 and 96 ± 3.6, respectively; P = .003). Increased BM cellularity of Opn–/– mice was associated with a significant increase in the proportion and total number of LSK cells in these animals compared with wt controls (P < .001) (Figure 4B). Collectively, these data suggest that Opn plays a key role in the physiologic regulation of HSCs. To investigate possible mechanisms underlying the role of Opn on HSC proliferation and lodgment, a series of in vitro studies was performed to analyze the binding of HSCs to Opn and to examine the functional consequences of this interaction.
In vivo Opn is involved in the regulation of HSC proliferation. (A) BM was analyzed for progenitor cell content using an in vitro colony-forming assay 3 days after 5FU cytotoxic challenge. There was a significant reduction in the number of cells with HPP-CFC in the presence of 4 stimulatory growth factors from an Opn–/– microenvironment (▪) compared with wt controls (▦). Data are the mean ± SEM of triplicate plates from 3 individual mice in 2 independent experiments. *P < .05. Furthermore, HSCs (LSK cells) cycle significantly faster in the absence of Opn in the hematopoietic microenvironment (B). Compared with HSCs isolated from a wt microenvironment (▦), significantly more HSCs isolated from an Opn–/– microenvironment (▪) had undergone cell cycle and incorporated BrdU after 4 weeks of continual oral administration. Data are the mean ± SEM of 3 individual mice from 2 independent experiments. *P < .05.
In vivo Opn is involved in the regulation of HSC proliferation. (A) BM was analyzed for progenitor cell content using an in vitro colony-forming assay 3 days after 5FU cytotoxic challenge. There was a significant reduction in the number of cells with HPP-CFC in the presence of 4 stimulatory growth factors from an Opn–/– microenvironment (▪) compared with wt controls (▦). Data are the mean ± SEM of triplicate plates from 3 individual mice in 2 independent experiments. *P < .05. Furthermore, HSCs (LSK cells) cycle significantly faster in the absence of Opn in the hematopoietic microenvironment (B). Compared with HSCs isolated from a wt microenvironment (▦), significantly more HSCs isolated from an Opn–/– microenvironment (▪) had undergone cell cycle and incorporated BrdU after 4 weeks of continual oral administration. Data are the mean ± SEM of 3 individual mice from 2 independent experiments. *P < .05.
HSCs adhere to Opn
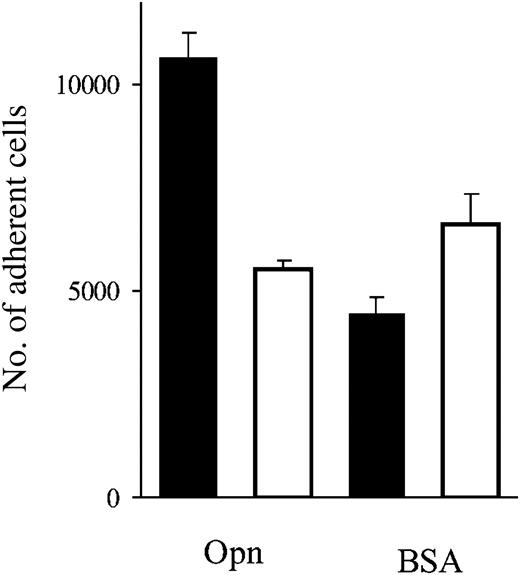
Cell adhesion assays were performed to analyze adhesion of HSCs to full-length recombinant human Opn. Compared with control wells coated with BSA, 25% of CD34+ cells exhibited specific cation-dependent adhesion to Opn (Figure 5). To determine whether β1 integrins are specifically responsible for this adhesion, CD34+ cells were treated with the specific β1 integrin–blocking antibody P5D2. As shown in Figure 5, P5D2 completely blocked adhesion of CD34+ cells to Opn, thereby demonstrating the key role of β1 integrin in mediating HSCs' adhering to Opn.
In vivo, the absence of Opn in the microenvironment results in a significant increase in HSCs and consequently total BM cellularity. (A) Compared with wt controls Opn–/– mice had a significant increase in total marrow cellularity. *P = .003. (B) In addition, there is also a significant increase in the number of LSK cells present in the BM. *P < .001. Data are the mean ± SEM of femurs, tibias, and iliac crests from 5 mice.
In vivo, the absence of Opn in the microenvironment results in a significant increase in HSCs and consequently total BM cellularity. (A) Compared with wt controls Opn–/– mice had a significant increase in total marrow cellularity. *P = .003. (B) In addition, there is also a significant increase in the number of LSK cells present in the BM. *P < .001. Data are the mean ± SEM of femurs, tibias, and iliac crests from 5 mice.
Adhesion of CD34+ cells to immobilized Opn is specifically mediated by β1 integrin. Calcein-AM–labeled BM CD34+ cells were assayed for their ability to attach to GST fusion–tagged full-length human Opn (▪). The ability of β1 integrin to mediate this process was analyzed by preincubating the cells in the specific β1 integrin–blocking antibody P5D2 prior to being deposited in the wells (□). Data are the mean ± SEM of triplicate wells representing 3 independent experiments.
Adhesion of CD34+ cells to immobilized Opn is specifically mediated by β1 integrin. Calcein-AM–labeled BM CD34+ cells were assayed for their ability to attach to GST fusion–tagged full-length human Opn (▪). The ability of β1 integrin to mediate this process was analyzed by preincubating the cells in the specific β1 integrin–blocking antibody P5D2 prior to being deposited in the wells (□). Data are the mean ± SEM of triplicate wells representing 3 independent experiments.
Opn is a negative regulator of HSC proliferation and differentiation in vitro
Earlier in vivo experiments with Opn–/– animals suggested Opn promotes HSC quiescence. Consequently, a series of studies was conducted to investigate potential mechanisms involved in this phenomenon. Initial experiments were performed to determine the functional significance of HSC binding to Opn. Previous studies from this and other laboratories have demonstrated that ligation of cell-surface adhesion molecules on primitive hematopoietic cells, including P-selectin glycoprotein ligand-1 (PSGL-1), CD164, CD43, and HA, results in the in vitro inhibition of HSC proliferation,32,33,37,38 which in part is mediated by induction of apoptosis. Accordingly, the possibility that HSCs' binding to Opn could result in similar growth inhibition was investigated in stroma-free, cytokine-dependent cultures of both primitive murine and human hematopoietic progenitors. Initial experiments using an enriched murine HSC cell population (LSK) demonstrated a 70% and 35% reduction in total cell numbers after 6 days, as compared with growth factors alone, following culture in the presence of tcOpn or HABP, respectively. Subsequent experiments were performed to assess the effects of Opn on hierarchically distinct populations of primitive and committed human hematopoietic progenitor cells. As demonstrated in Figure 6, culture of human CD34+CD38– cells with Opn resulted in a profound suppression of proliferation, despite cells being stimulated by the potent combination of 6 early-acting hematopoietic growth factors, G-CSF, SCF, FLT3-L, MGDF, IL-6, and IL-3. This inhibition of CD34+CD38– cell proliferation was similar to that previously described following the binding of HA expressing human HSCs to a surrogate ligand HABP33 (Figure 6A). Noticeably, this inhibition occurred only when cells were cultured with tcOpn. Incubation of human CD34+CD38+ cells with native Opn did not result in growth inhibition, suggesting that a conformational change in Opn following thrombin-cleavage is critical for this effect. Furthermore, inhibition of cell proliferation by tcOpn was dose dependent and maximal at 15 μg/mL (Figure 6B). In addition to growth inhibition, incubating CD34+CD38– cells in increasing amounts of tcOpn suppressed myeloid differentiation as evidenced by a significant decrease in the number of CD15+ cells generated in the presence of 15 μg/mL tcOpn as compared with SDM alone (16% ± 1.2% and 5% ± 0.8%, respectively) (Figure 6C). A similar series of experiments was conducted simultaneously with committed progenitor cells (CD34+CD38+) isolated from the same CB samples. However, in contrast to the effects observed following culture of CD34+CD38– cells in the presence of tcOpn, growth of CD34+CD38+ cells was not inhibited. When 500 CD34+CD38+ cells were cultured for 6 days under control conditions or in the presence of tcOpn, or intact Opn, 9.5 ± 0.77 × 104, 8.0 ± 0.38 × 104, and 8.9 ± 1.9 × 104 cells were generated, respectively. These data suggested that the inhibitory effect of Opn is restricted to primitive HPCs within the CD34+CD38– subpopulation.
Thrombin-cleaved Opn but not intact Opn significantly inhibits hematopoiesis in the presence of 6-factor stimulation. (A) Sorted CD34+CD38– HSCs (384 per well) were plated in serum-deprived media (SDM) supplemented with 6 factors (▦) and intact bovine Opn (bOPN; ▪), hyaluronic acid binding protein (HABP; ▥), tcOpn (□), or the thrombin control (▤). After 6 days there was significant inhibition of cell proliferation in the presence of HABP and tcOpn. Data are the mean ± SEM of quadruplicate wells and are representative of 6 independent experiments. *P < .05 compared with SDM following analysis by one-way ANOVA and a means comparison using Tukey test. (B) Sorted CD34+CD38– HSCs (384 per well) were plated in the presence of SDM supplemented with 6 factors (▦), HABP (▥), or limiting doses of tcOpn (□) for 6 days. Data demonstrate a significant dose response with a maximal effect with 15μg/mL tcOpn. Data are the mean ± SEM of quadruplicate wells from 3 independent experiments. *P < .05 compared with SDM following analysis by one-way ANOVA and a means comparison using Tukey test. (C) After 6 days of culture, cells in panel B were analyzed for myeloid differentiation by the presence of CD15. In the presence of HABP or tcOpn there was a significant reduction in differentiation into myeloid cells. *P < .05 compared with SDM following analysis by one-way ANOVA and a means comparison using Tukey test.
Thrombin-cleaved Opn but not intact Opn significantly inhibits hematopoiesis in the presence of 6-factor stimulation. (A) Sorted CD34+CD38– HSCs (384 per well) were plated in serum-deprived media (SDM) supplemented with 6 factors (▦) and intact bovine Opn (bOPN; ▪), hyaluronic acid binding protein (HABP; ▥), tcOpn (□), or the thrombin control (▤). After 6 days there was significant inhibition of cell proliferation in the presence of HABP and tcOpn. Data are the mean ± SEM of quadruplicate wells and are representative of 6 independent experiments. *P < .05 compared with SDM following analysis by one-way ANOVA and a means comparison using Tukey test. (B) Sorted CD34+CD38– HSCs (384 per well) were plated in the presence of SDM supplemented with 6 factors (▦), HABP (▥), or limiting doses of tcOpn (□) for 6 days. Data demonstrate a significant dose response with a maximal effect with 15μg/mL tcOpn. Data are the mean ± SEM of quadruplicate wells from 3 independent experiments. *P < .05 compared with SDM following analysis by one-way ANOVA and a means comparison using Tukey test. (C) After 6 days of culture, cells in panel B were analyzed for myeloid differentiation by the presence of CD15. In the presence of HABP or tcOpn there was a significant reduction in differentiation into myeloid cells. *P < .05 compared with SDM following analysis by one-way ANOVA and a means comparison using Tukey test.
Opn does not induce apoptosis in HSCs
To examine the mechanisms responsible for the inhibition of hematopoiesis by Opn, we analyzed cultures of CD34+CD38– CB cells after 4 days under control conditions or in the presence of tcOpn, or intact Opn for the presence of apoptotic cells using a terminal deoxynucleotidyl transferase–mediated dUTP (deoxyuridine triphosphate) nick end labeling (TUNEL) assay. In accord with the data shown in Figure 6, there was significant inhibition of cell growth in the presence of tcOpn, but not intact Opn, compared with control wells (data not shown). However, this inhibition was not associated with induction of apoptosis (16.7% ± 0.3% and 17.3% ± 0.9% apoptotic cells for media and tcOpn, respectively; P > .05).
Discussion
Although it is widely accepted that a unique BM HM or niche is critical for regulating HSC fate, the exact identity of cells and their extracellular biosynthetic products that comprise the niche remain poorly defined. In the present study we provide evidence that Opn expressed within the endosteal region of BM is a key component of the niche that influences HSC location and moreover regulates their function.
In accord with previous studies examining Opn mRNA expression within bone tissue,39 we have now shown that Opn protein is abundantly expressed in a very restricted zone at the endosteal interface of bone and hematopoietic tissue. Osteoblasts within this zone have been proposed as key components of the HSC niche and implicated in regulating HSC numbers, both in vitro and in vivo.4-6,40 This may be mediated in part by direct cell-cell contact, whereby angiopoietin-1 or membrane-bound Jagged1 on osteoblasts elicits signaling of Tie2 or notch1 expressed on HSCs, respectively, resulting in an increased number of HSCs. Notably, cells expressing Jagged1 and angiopoietin-1 display an osteoblastic morphology and express Opn.4,6 Our data suggest that, in addition to both Jagged1 and angiopoietin-1, Opn expressed and secreted by osteoblasts within this location is also involved in hematopoietic regulation, but in contrast promotes HSC quiescence.
Previous studies performed in our laboratory demonstrate that membrane-bound SCF,41 HA,33 and CD44 (S.K.N., unpublished observations, October 2002) promote the directed migration and/or retention of HSCs to the endosteal region where Opn is expressed at high levels. The almost random distribution of HSCs within BM following transplantation into Opn–/– mice provides evidence that Opn is involved in both TMM and lodgment of HSCs. The engraftment defect, observed in Opn–/– mice that received transplants with wt LSK cells, is consistent with an impaired ability of these “normal” donor cells to lodge in an endosteal HM and supports the concept that Opn is a critical component of the stem cell niche. This observed engraftment defect (Figure 2B) is also consistent with a compromised ability of the Opn–/– microenvironment to sustain hematopoiesis as measured by the comparative survival of wt and Opn–/– mice that received transplants with limiting numbers of LSK cells. Whereas there is no significant difference in the survival of myeloablated wt mice that received transplants with 3000 cells and as few as 300 LSK cells, there is a diminished ability of wt LSK cells to reconstitute hematopoiesis in Opn–/– mice as evidenced by decreased survival of myeloablated Opn–/– mice that received transplants with fewer than 3000 LSK cells. Analysis of the relationship between transplanted cell dose and survival of wt and Opn–/– mice allows us to infer that there is at least a 5-fold decrease in the efficiency of lodgment and engraftment of LSK cells in myeloablated Opn–/– versus wt mice. This inference is based on the assumption that the survival of wt mice that received a transplant will be compromised in a way that is similar to that observed in Opn–/– mice at transplanted LSK cell doses below 300 cells per mouse. These data strongly suggest that Opn is not only essential for the TMM and lodgment of HSC but also acts as a potent extrinsic regulator of transplanted HSCs. Furthermore, the lack of a significant difference in the proportion of donor cells detected in the peripheral blood short-term after transplantation (6 weeks) but the emergence of a significant engraftment defect long-term after transplantation (12 weeks) suggests that cells that home to the Opn–/– microenvironment, but have an altered spatial distribution within the marrow, cycle more rapidly, resulting in lower long-term potential. Moreover, the data also suggest that differences in the relative proportion of transplanted cells lodging in the endosteal region predict the quality of engraftment and hematopoietic regeneration.
The question as to whether these affects can be attributed to the secreted and or anchored forms of Opn needs to be addressed. Opn is known to be chemotactic for a variety of cells, including macrophages,42,43 which suggests it may potentially act like the chemokine stromal cell–derived factor-1 (SDF-1) in promoting directed migration of HSCs to the BM. However, we found no evidence of a chemotactic role with HSCs for any form of Opn tested in vitro (data not shown); thus, the exact mechanism for Opn affecting TMM and lodgment remains to be determined. A range of experiments is in progress to investigate whether Opn cooperates with or modulates SDF-1 and/or SCF in HSC chemotaxis.
The most compelling evidence that Opn might directly regulate hematopoiesis is provided by the analysis of hematopoiesis in the Opn–/– mice and in experiments that examine the cell-cycle status of primitive HPCs isolated from Opn–/– mice fed BrdU continuously for 4 weeks. The significant increase in BM cellularity and the proportion and total number of LSK cells observed in Opn–/– mice suggests that under normal steady-state conditions Opn acts as a negative regulator of HSC proliferation by actively maintaining quiescence. The notion that Opn inhibits HSC cell-cycle progression is supported by studies in which wt and Opn–/– mice were fed BrdU continuously for 4 weeks. In contrast to that observed in wt animals, essentially all LSK cells isolated from Opn–/– mice exhibit incorporation of BrdU over this time course. This suggests that Opn contributes to maintenance of HSC quiescence by inhibiting entry into the cell cycle, an effect that is alleviated when Opn is not present within the BM HM. Further evidence that Opn is a potent in vivo negative regulator of HSC proliferation is provided by our 5FU studies. In comparison with wt animals, significantly fewer HPP-CFCs are present in the BM of Opn–/– mice 3 days after 5FU. However, there was no significant difference in the number of LPP-CFCs, suggesting that Opn preferentially inhibits primitive HPCs.
In accord with this concept, exogenous Opn inhibits proliferation of murine LSK cells and primitive human CD34+CD38– but not CD34+CD38+ cells in a dose-dependent manner when cultured in combinations of early-acting synergistic growth factors. In this regard, the extent of growth inhibition is similar to that observed following PSGL-1–mediated adhesion of CD34+ cells to P-selectin32 and cross-linking HA on murine and human HPCs.33 In addition, culturing CD34+CD38– cells in the presence of tcOpn also resulted in reduced myeloid cell differentiation as evidenced by reduced numbers of CD15+ cells.
It is well recognized that Opn is bound by multiple cell types through either RGD (recognition sequence arginine-glycine-aspartic acid)–dependent or -independent adhesive interactions. Osteoclasts interact with Opn within the bone matrix through cell-surface CD44 and αvβ3 integrins to mediate migration, attachment, and resorptive activity.12,44 Our data demonstrate that HSCs directly interact with Opn via β1 integrins and are not consistent with any CD44 isoforms playing a major role. CD44v6, which has been reported to bind Opn,23 is expressed by a very limited number of human HPCs (1.5%-3.6%).45 The expression of other CD44 isoforms such as CD44v7 and CD44v9 remains undetermined. However, as our data demonstrate that 25% of CD34+ cells bind Opn without stimulation and this adhesion is completely abrogated by a specific β1-blocking antibody, it is highly unlikely that CD44 isoforms mediate the adhesion of hematopoietic progenitors to Opn. The β1 integrin–dependent binding of HPCs to Opn could be occurring through either α4 and/or α5, both of which are expressed by HPCs (reviewed by Simmons et al28 ), and both of which have previously been shown to directly interact with Opn.16,20 Furthermore, other αβ1 integrins may also potentially be involved. For example, α9β1 is known to bind to Opn,46 but the expression of this particular integrin by HPCs has not been investigated.
Within the hematopoietic niche the main source of Opn is likely to be osteoblasts lining bone surfaces within the BM cavity. Osteoblasts have previously been shown to stimulate the expansion of HSCs,4 potentially through a parathyroid hormone–dependent mechanism that results in up-regulation of Jagged1 and subsequent increased signaling through its cognate receptor Notch1 on HSCs.47-49 Our data demonstrate that a direct interaction between HSCs and Opn produced by osteoblasts results in β1 integrin–mediated inhibition of cell proliferation. The recent studies of Iwata et al50 suggest that the coculture of CD34+ cells in the presence of the HS-27a stromal cell line plus monocytes in medium containing Opn results in a down-regulation of Notch1 after 4 days, which was inversely correlated to the amount of Opn present. Whether this effect is mediated by a direct interaction between Opn and CD34+ cells or indirectly via the stromal cell line and or monocytes remains unclear. We propose that osteoblasts exert both inhibitory and stimulatory effects on HSC proliferation and differentiation via different and or overlapping mechanisms. In respect to Opn, extensive posttranslational modification, including phosphorylation, sulfation, glycosylation, and cleavage is known to occur, generating molecular mass variants that range in size from 25 to 75 kDa.15,51 It remains unknown which glycoforms and phosphorylation variants are expressed by osteoblasts that line the endosteal region of bone and therefore how these might affect HSCs.
Osteopontin can also be modified through cleavage by matrix metalloproteinases (MMPs) and thrombin, to generate fragments that bind to specific cell-surface integrins to initiate adhesion and migration.52 For example, cleavage of Opn reveals a cryptic site for adhesion to α9β117 that may be used by HSCs to bind to tcOpn. BM stromal cells and hematopoietic cells, including monocytes and developing myeloid cells, express MMP-3 and MMP-7, both of which cleave Opn and therefore may modulate its effect on HSCs. Alternatively, Opn is also known to bind with high affinity to and activate pro–MMP-3,53,54 which is known to stimulate migration of CD34+ cells in vitro.55 Furthermore, MMP-9 cleaves SCF and may also cleave Opn, providing additional means for regulating activity of this molecule within the confines of the HSC niche.56 This concept is supported by our in vitro studies performed with intact or tcOpn. While the intact molecule induces apoptosis, the cleaved form does not and yet still suppresses proliferation of primitive murine and human HPCs.
In summary, our data identify Opn as a key component of the HSC niche. Opn exhibits a highly restricted pattern of expression at the endosteal surface and contributes to HSC transmarrow migration toward the endosteal region after transplantation. HPCs demonstrate specific adhesion to Opn via β1 integrins. In the absence of Opn, there is a marked increase in HSC cycling in vivo, consistent with a physiologic role for Opn as a negative regulator of HSC proliferation. Furthermore, exogenous Opn suppresses the proliferation and differentiation of primitive HPCs in vitro, a phenomenon that is not due to the induction of apoptosis. Collectively, these data identify Opn as-yet unrecognized component of endosteally located stem cell niches that perform an important physiologic role in the regulation of HSC location and proliferation.
Prepublished online as Blood First Edition Paper, April 21, 2005; DOI 10.1182/blood-2004-11-4422.
Supported in part by grants from the National Health and Medical Research Council (NHMRC) of Australia, the Leukemia and Lymphoma Society of America, Association of International Cancer Research, and the Australian Stem Cell Centre.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We acknowledge help from Kate Sells and Kym Stanley with animal work, Brenda Aisbett with histology, and Ralph Rossi and Andrew Fryga with flow cytometry. We also thank the Mercy Hospital for Women, in particular Angie and Val, for coordinating CB collections.