Abstract
Hepatitis C virus (HCV) is associated with B-cell lymphoproliferative disorders such as mixed cryoglobulinemia (MC) and B-cell non-Hodgkin lymphoma (B-NHL). The pathogenesis of these disorders remains unclear, and it has been proposed that HCV drives the pro-liferation of B cells. Here we demonstrate that certain HCV+MC+ subjects have clonal expansions of immunoglobulin M (IgM)+κ+IgDlow/−CD21lowCD27+ B cells. Using RT-PCR to amplify Ig from these singly sorted cells, we show that these predominantly rheumatoid factor-encoding VH1-69/JH4 and Vκ3-20 gene segment-restricted cells have low to moderate levels of somatic hypermutations. Ig sequence analysis suggests that antigen selection drives the generation of mutated clones. These findings lend further support to the notion that specific antigenic stimulation leads to B-cell proliferation in HCV MC and that chronic B-cell stimulation may set the stage for malignant transformation and the development of B-NHL. The finding that these hypermutated, marginal zone-like IgM+CD27+ B cells are clonally expanded in certain subjects with MC offers insight into mechanisms of HCV-associated MC and B-cell malignancy. This study was registered at www.clinicaltrials.gov as NCT00219999.
Introduction
Up to 170 million people worldwide are chronically infected with hepatitis C virus (HCV), which is the leading indication for liver transplantation in the United States and Europe.1,2 Although hepatocytes are the primary target for HCV infection, mixed cryoglobulinemia (MC), considered a benign B-cell proliferative disorder, can affect up to 50% of HCV patients.3,4 HCV MC is predominantly characterized by cold-precipitable complexes of monoclonal immunoglobulin (Ig) M kappa (κ) rheumatoid factor (RF), polyreactive IgG, HCV RNA, and HCV structural proteins.3,5,6 MC symptoms range from weakness, arthralgias, and palpable purpura to more severe manifestations, such as neuropathy and membranoproliferative glomerulonephritis.7 HCV infection is also associated with the development of B-cell non-Hodgkin lymphoma (B-NHL).8-14
The mechanisms by which HCV causes B-cell proliferation (reviewed in Dustin and Rice15) remain puzzling. Several studies have demonstrated the presence of abnormal clonal B-cell populations in the liver and blood of HCV–infected persons.16-18 Patients with HCV MC and B-NHL frequently have clonal B cells that use Ig heavy chain variable (VH) 1-69 and Igκ Vκ3 gene segments,19-22 which can encode RF of the WA idiotype.23 Chronic antigenic stimulation by HCV may select a clonally expanded B-cell receptor (BCR) repertoire, which later progresses to B-NHL,24 similar to Helicobacter pylori–induced mucosa-associated lymphoid tissue lymphomas.25 Consistent with this idea, Ig cloned from an HCV+ B-NHL patient was shown to bind to the HCV structural protein, E2. However, this Ig does not cross-react with IgG.26 It has also been suggested that HCV E2 directly activates polyclonal B cells by binding to CD81, a tetraspanin that forms part of the B-cell coreceptor.27 Furthermore, it was reported that the memory B-cell compartment from HCV+ persons is polyclonally activated and that it contains decreased steady-state levels of CD27+ memory cells, which rapidly differentiate independently of the BCR.28 However, these latter 2 studies fail to account for the clonal IgMκ restriction frequently seen in HCV MC and B-NHL. Others have proposed that direct HCV infection of B cells may cause oncogenic transformation, particularly through t(14;18) translocation.29,30 Although t(14;18)-positive cells have been detected in HCV-infected patients, they are also present in up to 50% of healthy persons.31 Moreover, it is controversial whether HCV can infect B cells (Lanford et al32 and L.B.D., unpublished data, 2007), and this hypothesis also fails to explain the clonal B-cell expansions frequently seen in HCV infection.
In support of the polyclonally activated B-cell model, it was recently reported that HCV+ patients have high levels of activated naive B cells in the blood and that levels of total B-cell activation do not significantly differ between MC+ and MC− persons.27 These findings contrasted with our earlier finding that most HCV patients had no evidence of circulating activated B cells.33 This discrepancy led us to analyze peripheral B cells from HCV+MC+ and HCV+MC− patients. We have found that, in most HCV patients, circulating B cells show no evidence of current or prior activation. However, certain HCV+MC+ pa-tients harbor a substantial population of clonally expanded IgM+Igκ+IgDlow/−CD21lowCD27+ B cells in the peripheral circulation. Moreover, these B cells express RF-like Ig that is in most cases hypermutated, indicating specific antigen-driven maturation. Furthermore, phylogenetic analysis suggests that this hypermutation is a result of antigen selection. An association of IgM+ memory-like B cells with MC, which itself is associated with B-NHL, is consistent with a model in which chronic, specific antigenic stimulation of IgM+ B cells predisposes toward neoplastic transformation.
Methods
Patients
The studies were approved by the Institutional Review Boards at the Rockefeller University and New York-Presbyterian Hospitals. Before enrollment, written informed consent was obtained from donors in accordance with the Declaration of Helsinki. We enrolled HCV Ab+, HCV RNA+ subjects whose medical history or physical examination was consistent with arthralgias and/or palpable purpura. We additionally screened for sensorimotor neuropathy by neurologic examination. All HCV RNA+ subjects were HIV Ab−. For controls, we enrolled HCV Ab−, HBV-immunized healthy volunteers at low risk for HIV. We also enrolled HCV RNA−, HCV Ab+ patients who had undergone antiviral treatment with pegylated interferon and ribavirin and who subsequently had 2 separate confirmations of HCV RNA less than 50 IU/mL at least 6 months after cessation of treatment and were sustained virologic responders.
Blood collection and processing
A total of 50 mL of blood was collected into Vacutainer tubes containing acid-citrate-dextrose solution A (BD Biosciences, Franklin Lakes, NJ) and a serum separator tube (prewarmed to 37°C). We obtained serum by allowing blood to clot at 37°C followed by centrifugation at 800g. Plasma was obtained by room-temperature centrifugation and was stored at −80°C. To obtain peripheral blood mononuclear cells (PBMCs), cells were separated on lymphocyte separation medium (ICN, Costa Mesa, CA) by centrifugation at 800g. The mononuclear cell layer was washed 3 times in phosphate-buffered saline (PBS) supplemented with 1% N-2-hydroxyethylpiperazine-N-2-ethanesulfonic acid (HEPES) and 2% fetal bovine serum. Cells were resuspended at a concentration of 107/mL in RPMI 1640 supplemented with 0.5% HEPES, 20% fetal bovine serum, and 7.5% dimethylsulfoxide for cryopreservation. Cells were slowly frozen to −80°C and maintained at −150°C. Viable cell recovery was typically more than 90% as judged by incorporation of an amine-reactive violet dye (LIVE/DEAD Fixable Dead Cell Stain, Invitrogen, Carlsbad, CA).
Clinical tests
To test for MC, we incubated serum at 4°C for 1 week and examined it daily for the presence of a cryoprecipitate.34 To determine MC type, an established protocol was followed.35 Cryoprecipitate was spun in a 4°C microcentrifuge at 650g for 15 minutes, the supernatant was removed, and the pellet was vortexed 6 times with 5 mL of ice-cold PBS, each time spinning out the cryoprecipitate for 15 minutes at 650g. The sample was then resuspended in 100 μL of PBS and was redissolved by incubation at 37°C for 1 hour. Immunofixation was performed for IgM, IgG, IgA, Igκ, and Igλ using an immunofixation kit (Binding Site, Birmingham, United Kingdom), following the manufacturer's instructions. HCV RNA was quantified by the Roche Amplicor assay (version 2.0, Roche Diagnostics, Branchberg, NJ). HCV genotypes were determined by sequencing of the HCV NS5B region. Liver biopsies were evaluated by pathologists according to the Scheuer system.36 These actions, in addition to serum alanine aminotransferase (ALT) measurements, were performed as part of HCV patients' medical care. We measured plasma IgM RF using ELISA (Bethyl Laboratories, Montgomery, TX).
Antibodies
The following mouse mAbs were used: anti-CD19, anti-CD20, anti-CD3, anti-IgM, anti-IgD, anti-CD27, anti-CD69, anti-CD5, anti-CD21, and anti-CD25. FITC, phycoerythrin (PE), PE-Cy7, peridinin chlorophyll protein cyanin 5.5 (PerCP-Cy5.5), allophycocyanin, Alexa Fluor 700, Alexa Fluor 488, and allophycocyanin Cy7 were used as fluorophores. Conjugated mAbs were obtained from BD PharMingen (San Diego, CA). Goat polyclonal F(ab′)2 PE anti-λ and biotin anti-κ were from Southern Biotech (Birmingham, AL), and LIVE/DEAD Fixable Dead Cell Stain was from Invitrogen.
Flow cytometric analysis
Cells (7 × 106/sample) were stained with the indicated Abs at RT in PBS supplemented with 2% (w/v) BSA (Fraction V; Fisher Biotech, Fair Lawn, NJ) and 0.02% NaN3. Cells were incubated with primary and secondary Abs for 30 minutes each, and were washed thrice after each stain with incubation buffer. Cells were fixed in PBS/2% paraformaldehyde and analyzed within 1 hour on an LSRII flow cytometer (BD Immunocytometry Systems, San Jose, CA). Data were analyzed using FlowJo (Tree Star, Ashland, OR). Lymphocytes were identified by forward and side-angle light scatter characteristics. Dead lymphocytes, identified by positive LIVE/DEAD stain, were excluded from further analysis.
CDR3 PCR
DNA was recovered from 3 × 106 PBMCs using a QIAamp DNA Blood Mini Kit (Qiagen, Valencia, CA). PCR amplification was performed on up to 0.5 μg of DNA with a seminested protocol of amplification according to a well-established procedure.37 The upstream primer was complementary to the conserved third framework V region (FR3) of the IgH gene, and the downstream primer annealed to an outer conserved region of the IgH joining (J) region in the first round of amplification and to an inner conserved sequence of the same J region in the second round.38 All samples were tested in 2 separate PCR experiments, and clonal and polyclonal CDR3 DNA controls, as well as a water only control, were included. At the end of amplification, 15 μL of the reaction mixture was analyzed by 12% polyacrylamide gel electro-phoresis, stained with ethidium bromide, and optically analyzed by ultraviolet transillumination. Gels were scanned using an Epson Expression 1600 scanner (Epson America, Torrance, CA) and densitometric analysis was performed with ImageJ software (National Institutes of Health [NIH], Bethesda, MD).39 Clonal expansion was determined by the presence of one or more discrete, dominant bands within an 80- to 120-bp size range, and a polyclonal population was indicated by the presence of a smear with no specific dominant bands.
Single-cell sorting
For single-cell sorting, incubations and washes were performed as for immunophenotyping, except incubations were performed on ice in the absence of added 0.02% NaN3. Moreover, cells were not fixed in paraformaldehyde after staining. Either IgM+κ+CD21lowCD27+, IgM+κ+CD21lowCD27−, IgM+κ+CD5+CD27+, IgM+κ+CD5−CD27+, or IgM+κ+CD27+, single cells were sorted using a MoFlo cell sorter (Dako Cytomaton, Ft. Collins, CO), directly seeded into 96-well plates containing 4 μL lysis solution (0.5× PBS containing 10 mM DTT, 2 U RNase Inhibitor (Invitrogen) and 3 U Prime RNase Inhibitor (Eppendorf)), and immediately frozen on dry ice. Samples were stored at −80°C.
VH and Vκ RT-PCR
We followed an established protocol for cloning VH and Vκ from single B cells.40 Briefly, RNA was reverse transcribed in 14 μL reactions containing random hexamer primers and 50 U Superscript II RT (Invitrogen) for 55 minutes at 40°C. RT-PCR reactions, primer sequences, and cloning strategy were as previously described.40 For VH, we used a pool of family-specific sense primers directed to the 5′ conserved leader and V regions, and a downstream antisense primer directed to the first constant region of IgM (Cμ). Amplification was performed using Taq polymerase (Invitrogen). A second round of PCR was performed on this reaction product with VH- and JH-specific primers. For Vκ, we used pooled family-specific primers directed to the 5′ conserved leader and Vκ regions, and a downstream antisense primer to the conserved Cκ region. We amplified this PCR product with a 5′ pan Vκ primer and a downstream 3′ Cκ primer. IgH and Igκ variable regions were sent for sequencing (Biotic Solutions, New York, NY).
Analysis of somatic hypermutation and phylogeny
The International ImMunoGeneTics information system41 and NIH Joinsolver42 were used to identify the V, D, and J segments and somatic mutations of Ig genes.43 The ratio of replacement (R) and silent (S) mutations was determined and analyzed according to a binomial distribution model,44 using a web-based JAVA applet.45 Nucleotide sequences were aligned using Clustal W.46 Phylogenetic trees were constructed with MacVector (Accelrys, San Diego, CA), using distance-based neighbor-joining analysis performed on Tamura-Nei neighbor estimates. Bootstrap analyses were conducted using 1000 replicates.
Statistics
Values of clinical tests are reported as means (± SD). To test the null hypothesis that clonal Ig was not more prevalent among HCV+MC+ subjects, Fisher exact test was used to compute a P value. All other comparisons used the Kruskal-Wallis test, followed by the Dunn multiple comparison test, as appropriate. We computed all statistics with Prism (GraphPad, San Diego, CA).
Accession numbers
Results
Characteristics of study subjects
Twenty-five patients with signs or symptoms suggestive of cryoglobulinemic vasculitis, such as arthralgia, palpable purpura, peripheral neuropathy, and glomerulonephritis, were enrolled. Subsequent tests revealed that 12 of these patients had demonstrable cryoprecipitates. Characteristics of the groups are presented in Table 1. The HCV Ab− group was completely free of arthralgia, palpable purpura, and neuropathy. Two HCV−, Ab+ subjects had arthralgias. Only HCV+ subjects had laboratory evidence of MC. HCV−, Ab+ subjects had previously been infected with HCV genotype 1 (n = 7), 2b (n = 1), 3b (n = 1), or HCV of unknown genotype (n = 1).
Table 2 describes the characteristics of the HCV-infected group. One HCV+MC+ subject (1308) had a triclonal paraproteinemia on serum immunofixation electrophoresis and underwent bone marrow biopsy, which revealed monotypic B cells with a normal karyotype, consistent with low-grade NHL. Another HCV+MC− patient (1148) had NHL in remission after treatment with cyclophosphamide, doxorubicin, vincristine, and prednisone 1 year before enrollment. Compared with MC− subjects, MC+ subjects tended to have more than one MC related symptom or disease. Consistent with an earlier report,48 monosymptomatic arthralgia was nonspecific for MC. IgM RF was not significantly elevated in HCV+MC+ subjects compared with HCV+MC− subjects. In the 10 subjects in whom MC was typed, the cryoprecipitate was IgMκ, and 8 of 10 subjects had type II MC.
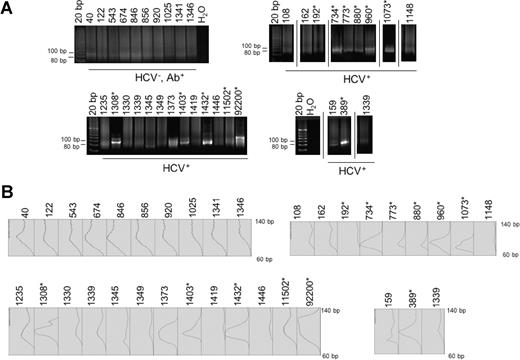
HCV+MC+ patients have clonal B-cell expansions
We performed Ig CDR3 PCR on DNA isolated from PBMCs to assess for clonality (Figure 1). HCV−, Ab+ patient samples yielded DNA smears indicating polyclonality. Similarly, all HCV Ab− volunteers had evidence of polyclonal CDR3 (data not shown). Consistent with previous reports,16,17 clonal CDR3 was highly correlated with the presence of MC. Monoclonal or oligoclonal bands with sizes between 80 to 120 base pairs were found in 10 of 12 HCV+MC+ subjects, and in 1 of 13 HCV+MC− subjects (P < .001, Fisher exact test). These results suggest that the elevated IgM and RF frequently seen in HCV+MC+ patients is the result of clonal B-cell proliferation. Because, in the absence of overt malignancy, B-cell clonal expansion requires activation through a B cell's unique BCR, these data are consistent with the hypothesis that there is an antigenic stimulus that causes MC disease in different HCV-infected patients.
Ig CDR3 PCR. DNA was isolated from PBMCs, amplified following an established protocol (see “CDR3 PCR”) and run on a 12% polyacrylamide gel. Polyclonal CDR3s are indicated by the presence of DNA smears between 80 and 120 bp, the expected size range of CDR3. Monoclonal and oliglonal CDR3s are reflected by the presence of solitary, or 2 to 3 bands, respectively, in the expected size range (A). Densitometric analysis of gel bands (B). *Patients with MC.
Ig CDR3 PCR. DNA was isolated from PBMCs, amplified following an established protocol (see “CDR3 PCR”) and run on a 12% polyacrylamide gel. Polyclonal CDR3s are indicated by the presence of DNA smears between 80 and 120 bp, the expected size range of CDR3. Monoclonal and oliglonal CDR3s are reflected by the presence of solitary, or 2 to 3 bands, respectively, in the expected size range (A). Densitometric analysis of gel bands (B). *Patients with MC.
B cells from certain HCV+MC+ subjects are biased toward a restricted IgM+κ+IgDlow/−CD21lowCD27+ phenotype
We used flow cytometry to identify the expanded B-cell clonal subpopulation in this subset of HCV+MC+ subjects. We tested whether our cell freezing protocol altered the detectable B-cell immunophenotype. We saw no difference in B-cell activation markers between fresh and frozen B-cell samples (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article). We then determined whether HCV+ subjects with clonal Ig had increased percentages of peripheral B cells (Table 3). After gating on lymphocytes, we excluded dead cells, and we selected CD19+, CD20+ B cells (Figure S2A). B-cell percentages (measured as the percentage of lymphocytes expressing CD19 and CD20) were slightly increased in some HCV+ patients compared with HCV Ab− volunteers and HCV−, Ab+ patients. There were no differences in B-cell percentages between HCV+MC+ and HCV+MC− groups. When we calculated the absolute numbers of B cells by multiplying the B-cell percentages by the corresponding total lymphocyte counts, we found no differences among the groups (data not shown). These findings confirmed our earlier study reporting normal B-cell frequencies in most HCV+ subjects.33 We did not detect significantly different percentages of the activation markers CD69 and CD25 among B cells from our patient groups (data not shown), suggesting that B cells are not polyclonally activated during HCV infection.
Consistent with the fact that MC RF is IgMκ, we found that certain HCV+MC+ patients had B cells with a tremendous κ light chain bias, exhibiting κ/λ ratios up to 90:10 (Figure S3A). This ratio was significantly increased among HCV+ subjects with clonal, as opposed to polyclonal, CDR3 (Table 3). Most of the κ+ and IgM+ B cells in these patients expressed CD27 (Figure S3B,C), which is a marker for memory B cells.49 HCV+ subjects with clonal, as opposed to polyclonal, CDR3 had significantly increased percentages of κ+CD27+ and IgM+CD27+ B cells. Most of the expanded IgM+ B cells were IgDlow/− (Figure S3D). Interestingly, CD27+ B cells from 5 of 11 HCV+MC+ subjects, but from none of the HCV+MC− subjects or controls, exhibited markedly diminished CD21 (Figure S3E). HCV+ subjects with clonal, as opposed to polyclonal, CDR3 had significantly increased percentages of CD21lowCD27+ B cells. We thus identified a subset of HCV+ patients with clonal Ig that had an expansion of IgM+κ+IgDlow/−CD21lowCD27+ B cells. We gated on κ+CD27+ and IgM+CD27+ B-cell sub-sets in selected patients (Table 4; Figure S4). In selected HCV+MC+ patients, the expanded IgM+κ+CD27+ subset was pre-dominantly IgDlow/−.
Several groups have reported increased intrahepatic and peripheral CD5+ B cells among HCV+ subjects, and they have suggested that this reflects increased “natural” Ab production in HCV infection.50,51 Although CD5+ B-1a cells seem to be responsible for the production of natural Abs in mice,52 the association between CD5+ B cells and natural Abs in humans is not as clear, and evidence suggests that CD5 expression is inducible.53 Despite these drawbacks, we measured CD5+ B cells by flow cytometry (Figure S2C). Consistent with another group's finding54 and our earlier report,33 the frequency of CD5+ B cells was not significantly increased among HCV+ subjects, nor did frequencies significantly differ between HCV+MC+ and HCV+MC− patients (Table 3). However, 2 HCV+ patients (1446 and 960) had very high levels of CD5+ B cells. Taken together, these data confirm that the majority of HCV+ patients do not have expansions of CD5+ B cells.
HCV+MC+ subjects' expanded IgM+ κ+CD21lowCD27+ B cells bear restricted, clonal Ig
We sorted single IgM+κ+CD21lowCD27+ B cells from subjects LDU 077, LDU 095, 389, 773, 1403, 1308, and 1432. We were unable to singly sort IgM+κ+CD21lowCD27+ B cells from other HCV+MC+ patients either because of a lack of cryopreserved PBMCs (subjects 734, 880, and 92200), or because of the low frequency of these cell subsets. We were able to singly sort IgM+κ+CD27+ B cells from subject 1073. We cloned the entire expressed Ig VH region (and for selected subjects, the entire Ig Vκ region) from individual cells using a 2-stage, unbiased Ig RT-PCR strategy.40 Results for VH and Vκ are summarized in Tables 5, 6. In contrast to HCV Ab− controls, IgM+κ+CD21lowCD27+ B cells from the HCV+MC+ patients exhibited marked VH, JH, and Vκ gene segment usage restriction. Eleven of 12 IgM+κ+CD21lowCD27+ B cells isolated from patient 773, 22 of 22 from subject 1432, and 10 of 18 from patient 1403 used the RF-encoding gene segments VH1-69/JH4. There was a similar pattern of Vκ3-20 restriction in these subjects. All IgM+κ+CD21lowCD27+ B cells isolated from patient 1308 used VH3-7/JH3 and Vκ3-15/Jκ1.
Earlier studies have shown that hepatic lymphoid aggregates from HCV+MC+ subjects consist predominantly of CD5+ B cells.55 As mentioned in “B cells from certain HCV+MC+ subjects are biased toward a restricted IgM+κ+IgDlow/−CD27+ phenotype,” increased intrahepatic and peripheral CD5+ B cells have been reported among HCV+ subjects,50,51 suggesting that the B cells arising in the liver and stimulated by HCV antigens may be CD5+. We therefore decided to clone Ig from IgM+κ+CD27+CD5− and IgM+κ+CD27+CD5+ B cells isolated from subjects 1446 and 960 (who both had increased percentages of CD5+ B cells) and from subject 1403 (to determine whether unmutated clonal Ig was produced by CD5+ cells). We could not recover any IgM+κ+CD27+CD5+ B cells from subject 960. Of IgM+κ+CD27+CD5− B cells, 1 of 7 clones from subject 960, 2 of 6 from subject 1403, and 3 of 13 from the HCV+MC− subject 1446 demonstrated VH1-69/JH4 gene segment usage, whereas no VH1-69/JH4 usage was seen among 10 clones from subject 1446's IgM+κ+CD27+CD5+ B cells, suggesting that this gene segment restriction is not seen in CD5+ cells. Of the 2 VH1-69+/JH4+ clones from 1403, one was unmutated and the other had only 2 mutations, suggesting that the unmutated clonal population may arise from CD5− B cells.
Patients 1308 and 1432 had monoclonal IgM+κ+CD21lowCD27+ B cells, as indicated by the presence of identical CDR3 and palindromic (P) and nontemplated (N) nucleotides at the VHDH, DHJH, and VκJκ joins. We identified 2 clonal populations in subject 773. The largest, represented by 7 of 12 B cells, contained a CDR3 exactly identical to that previously reported from a patient with salivary gland mucosa–associated lymphoid tissue lymphoma.56 That identical CDR3 regions containing N nucleotides have been identified in 2 different patients strongly suggests a common antigenic stimulus in the 2 patients, as it is extremely unlikely that these identical regions could arise by chance. The VH1-69/JH4 clonal population in subject 1446's IgM+κ+CD27+CD5− B cells had a CDR3 that differed by one amino acid from a CDR3 previously recovered by another group from an unrelated HCV+MC+ subject's expanded B cells.57 We identified 2 clonal populations among subject 1403's IgM+κ+CD21lowCD27+ B cells. As mentioned, the predominant clonal VH1-69/JH4 population was also seen in 2 of 6 of 1403's IgM+κ+CD27+CD5− B cells. Clonal Ig was not seen in subject 389's IgM+κ+CD21lowCD27+ B cells nor in subject 1073's IgM+κ+CD27+ B cells. Because clonal Ig was seen in these subjects' unfractionated PBMCs, this suggests that the clonally expanded B cells in these subjects were not CD21lowCD27+.
The expanded IgM+κ+CD21lowCD27+ B cells in certain HCV+MC+ subjects contain somatically hypermutated Igs
The majority of expanded IgM+κ+CD21lowCD27+ B cells exhibited low to moderate levels of somatic hypermutation (SHM; Table 7). An exception was subject 1403 whose clonal VH1-69/JH4 cells were unmutated. Within each clonal IgM+κ+CD21lowCD27+ B-cell population, the mutational frequency varied significantly among individual cells. Except for subject 389, each HCV+MC+ subject from whom Igs were cloned had several Igs with significantly scarce R muta-tions in their FR regions, (pR(FR) < 0.05), indicative of selection based on structural constraint for antigen-Ig binding. However, only 3 of these Igs had a significant excess of R mutations in CDR, (pR(CDR) < 0.05). Despite VH SHM, CDR3 sequences were strikingly conserved among clonal populations, suggestive of a positive selection. Most Vκ were less hypermutated than their corresponding VH, reflective of the lower mutation rate of Igκ seen in the general population.49 In contrast to VH, more Vκ had an excess of R(CDR) than they had a scarcity of R(FR).
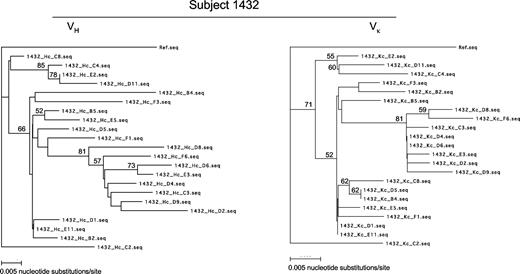
Igs from HCV+MC+ subjects demonstrate features of clonal evolution
We constructed phylogenetic trees for VH and Vκ from subject 1432's IgM+κ+CD21lowCD27+ B cells (Figure 2). When combined with the Ig mutation rates from Table 7, these trees demonstrate that for both VH and Vκ, mutations are shared among different B cells. A pattern of clonal evolution is apparent, as the more hypermutated clones also contain mutations present in the less hypermutated clones. Interestingly, 6 B cells (D2, D4, D6, D9, E3, and F6) that had highly evolved IgH also had significant scarce R(FR), further indication that a structural constraint in FR provides selective pressure for these cells. The VH and Vκ phylogenies correlate well with one another. Cells with relatively large VH mutational frequencies have correspondingly large Vκ mutational frequencies. This fact, combined with similar patterns of shared VH and Vκ mutations among these cells, provides strong evidence that the observed mutations are not PCR artifacts. Similar results were obtained on phylogenetic analysis of Ig clones from subjects 773, 1308, and 1403 (data not shown). Taken together, these data suggest that the expanded IgM+κ+CD21lowCD27+ B cells in certain HCV+MC+ subjects undergo successive rounds of SHM. However, the relatively low mutation rates and the occasional presence of unmutated B-cell clonal expansions suggest that affinity maturation is not an absolute requirement for these cells.
Phylogenetic analysis of VH (left) and Vκ (right) from subject 1432's IgM+κ+ CD27+CD21low B cells. Trees were constructed using neighbor-joining analysis of Tamura-Nei distances calculated from pairwise comparisons of Ig DNA sequences. Percentages of bootstrap support (> 50%) from 1000 replicate samples (analyzed by the neighbor joining method) are indicated to the left of the support node. VH and Vκ from B cell A5 of patient 1403 serve as reference sequences.
Phylogenetic analysis of VH (left) and Vκ (right) from subject 1432's IgM+κ+ CD27+CD21low B cells. Trees were constructed using neighbor-joining analysis of Tamura-Nei distances calculated from pairwise comparisons of Ig DNA sequences. Percentages of bootstrap support (> 50%) from 1000 replicate samples (analyzed by the neighbor joining method) are indicated to the left of the support node. VH and Vκ from B cell A5 of patient 1403 serve as reference sequences.
Discussion
A major finding of our study is the identification of clonally expanded IgM+κ+IgDlow/−CD21lowCD27+ B cells expressing hypermutated RF-like Ig in a subgroup of HCV+MC+ patients. In addition, we describe for the first time cloning of VH and Vκ from single B cells obtained from HCV+MC+ patients. Our cloning strategy was unbiased in its amplification of Ig gene segments; the gene segment usage we observed in our healthy volunteers corresponds to that previously reported in the general population.58 It is also unlikely that we overestimated mutational frequencies because of potential Taq polymerase errors. We performed duplicate VH PCR reactions on reverse-transcribed cDNA from 10 different B cells, and we noted only 2 discordant nucleotides (2 stage VH PCR error rate: 1 of 1860 nucleotides). Moreover, we routinely did not detect mutations in CD27− cells, and mutational frequencies among subjects' VH and Vκ were highly correlated.
The finding that a subset of HCV+MC+ patients have clonally expanded, hypermutated, Ig gene segment–restricted, memory-like B cells suggests that specific antigenic stimulation is responsible for the B-cell proliferation in HCV MC. Our findings contrast with an earlier claim that polyclonal activation of naive B cells occurs during chronic HCV infection.27 Of note, we did not detect any increased CD69 or CD25 expression among any subjects' B cells. However, this latter result is not surprising, given the role of CD69 in retaining activated B cells in lymph nodes.59 It is possible that any recently activated B cells may leave the blood and not be detected. Important, not all HCV+MC+ patients have noticeably expanded B-cell subsets. The finding of clonal VH1-69/JH4 B cells in subject 1446 (HCV+MC− and without a detectable clonal CDR3 band) suggests that these clonal expansions may be occurring subclinically in some patients. That we did not recover clonal Ig in the IgM+κ+CD21lowCD27+ B cells of patient 389 and in the IgM+κ+CD27+ B cells of patient 1073 (both of whom were HCV+MC+ with clonal CDR3, yet without detect-able B-cell expansion) suggests that either clonal Ig is present at low frequencies or is present in different B-cell subsets in these patients. Our results, which are consistent with 2 prior studies, lend support to the hypothesis that chronic, specific antigenic stimulation of IgM+ B cells predisposes toward neoplastic transformation. In one study, regression of WA RF-bearing IgM+κ+IgD−CD5− B cells occurred concomitantly with the decline of HCV RNA during interferon-α treatment.57 The CDR3 of the cells in the cited study57 is highly homologous to that of subject 1446's clonal IgM+κ+CD27+CD5− B cells. In another study, splenic marginal zone lymphoma regressed in patients whose HCV was successfully treated with interferon α-2b.60
IgM+CD27+ cells are important in defending against bacterial pathogens in a T cell–independent manner, and it has been proposed that such cells are the circulating form of splenic marginal zone (MZ) B cells.61,62 MZ B cells are thought to be distinct from GC or post-GC B cells,63 and SHM in these cells does not require accessory molecules such as CD40L or CD40.64 In healthy humans, IgM+ memory B cells have been demonstrated to comprise approximately 10% to 25% of peripheral B cells64,65 and to have lower SHM rates than class-switched memory B cells. We have found that IgM+CD27+ cells comprise up to 75% of circulating B cells in a subset of HCV+MC+ patients and that these cells have low levels of SHM. Moreover, these IgM+ memory B cells are IgDlow/−, which distinguishes them from previously reported hypermutated IgM+IgD+CD27+ B cells in healthy adults.49 Our findings are consistent with the fact that HCV is associated with both splenic66,67 and extrasplenic, nodal MZ lymphomas, the latter of which have been found to be made up of B cells frequently harboring mutated VH1-69 gene segments.68
Our finding that in certain HCV+MC+ subjects, IgM+ memory-like B cells have reduced expression of CD21 contrasts with the characterization of MZ cells as being CD21high.62 Interestingly, reduced CD21 expression was reported on B cells from patients with systemic lupus erythematosis69 and HIV.70 We have previously observed reduced CD21 expression on HCV+ patients' B cells.33 Down-regulation of CD21 may serve to dampen B-cell responsiveness to BCR-mediated activation and proliferation. However, it is also possible that reduced CD21 is a normal feature of B cells that have been stimulated by antigen,71 or it may be emblematic of apoptotic cells.72
Our analysis of CD5−IgM+κ+CD27+ and CD5+IgM+κ+CD27+ B cells, although conducted on only 3 subjects and 1 subject, respectively, suggests that the clonal, VH1-69/JH4-restricted B cells seen in some HCV+MC+ patients are CD5−. This is consistent with prior reports of CD5− MZ-like B-cell lymphoproliferation in some HCV+MC+ patients,57,60 and it suggests that CD5 expression is not a universal feature of the expanded B-cell subsets seen in HCV MC. We are currently in the process of sorting CD5−IgM+κ+CD27+ and CD5+IgM+κ+CD27+ B cells from additional, newly identified HCV+MC+ patients with clonal IgM+κ+IgDlow/−CD21lowCD27+ B-cell expansions.
An interesting finding is that, whereas 3 HCV+MC+ subjects had hypermutated clonal B cells, one patient's clonal B cells were of germ line sequence, despite being CD27+. Our studies are consistent with the findings of Ivanovski et al,19 who found restricted, hypemutated VH and VL genes in PBMCs isolated from HCV patients with immunocytomas. It is unclear if SHM correlates with autoreactivity in HCV MC. We are currently defining the autoreactive profiles of Ig cloned from our HCV+MC+ subjects. Whether autoreactivity is inversely correlated with the presence of SHM is of extreme interest.
It is not known how these Ig-restricted memory-like B cells are stimulated to expand in some HCV+MC+ patients. One possibility is that the Ig on these B cells reacts with an HCV antigen and/or cross-reacts with a self-molecule, such as IgG, which may be bound to HCV. The finding that the clonal B-cell population of one of our HCV+MC+ patients expresses a CDR3 that is exactly identical to the CDR3 from a patient with salivary gland lymphoma is intriguing in light of a report that a particular antigen selects Igs bearing identical CDR3 in different persons.73 Persistent inflammation is a common feature of HCV infection, Sjögren syndrome, and H pylori infection. All of these syndromes are associated with B-NHL. In these diseases, antigen-containing immune complexes may bind to low-affinity autoreactive BCR. Concomitant stimulation of toll-like receptors (TLR), coupled with (or in lieu of) cognate T-cell help, may lead to B-cell activation and proliferation. It has been shown in vitro that IgG-bound Borrelia burgdorferi is capable of breaking RF-expressing B cells' state of immunologic tolerance by binding to both BCR and TLR.74 Moreover, it has been shown that chromatin-IgG complexes can lead to activation of RF+ B cells by engagement of IgM and TLR9.75 We are currently testing the hypothesis that immune complexed HCV induces expansion of RF+ B cells by dual engagement of BCR and TLR7.
In conclusion, we have characterized in detail a subset of HCV+MC+ patients with gene segment-restricted, clonally expanded IgM+κ+IgDlow/−CD21lowCD27+ B cells. We emphasize that our studies are of peripheral B cells. It is unclear how representative these cells are of the B cells in the hepatic microenvironment. Importantly, clonal intrahepatic RF-producing B cells have been shown in HCV+MC+ patients.17 The identification of such highly restricted, potentially autoreactive, Igs in a subset of HCV+MC+ patients gives us hope that elucidation of the precise antigenic stimulus responsible for MC formation will reveal the mechanism of HCV-induced B-cell proliferative disorders.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We are grateful for the generosity of the patient volunteers. We thank the Rockefeller University Hospital Department of Nursing and Patient Care Services, Gertrudis Soto and Queenie Brown for assistance in patient enrollment and sample acquisition. Svetlana Mazel, manager of Rockefeller's Flow Cytometry Research Center, and Peter Lopez, manager of Aaron Diamond AIDS Research Center's Core Facilities, provided expert assistance with flow cytometry. We acknowledge Raymond Peterson for database management and Knut Wittkowski for statistical advice. We also thank Michel Nussenzweig and Sergey Yurasov for helpful discussions.
This study was supported in part by the National Institutes of Health/National Institute of Allergy and Infectious Diseases grant R01AI60561 (L.B.D.), the Irma T. Hirschl/Monique Weill-Caulier Trust (L.B.D.), General Clinical Research Center grant M01-RR00102 (to Rockefeller University Hospital), and Center for Translational Science Award grant 1UL1 RR024143-01 (to Rockefeller University Hospital) from the NIH National Center for Research Resources. E.D.C. is supported in part by the Clinical Scholar Program of Rockefeller University Hospital.
National Institutes of Health
Authorship
Contribution: E.D.C., L.B.D., R.M.G., and S.M. devised and performed experiments; E.D.C., G.V.L.-B., A.H.T., and I.M.J. provided patient referrals; E.D.C., L.B.D., C.M.R., S.M., G.V.L.-B., A.H.T., and I.M.J. interpreted results; and E.D.C. and L.B.D. designed the research and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Lynn B. Dustin, Center for the Study of Hepatitis C, Laboratory of Virology and Infectious Disease, Rockefeller University, Box 64, 1230 York Ave, New York, NY 10021; e-mail: dustinl@rockefeller.edu.