Abstract
Hodgkin lymphoma is a highly curable malignancy, but treatment outcome might be influenced by inherited gene polymorphisms determining anticancer agent metabolism. We prospectively collected peripheral blood lymphocytes from 313 patients with Hodgkin lymphomas to analyze GSTP1, GSTM1, GSTT1, UGT1A1, and CYP3A4 enzyme gene polymorphisms. All patients were treated with chemotherapy, associated with radiotherapy when they had localized disease. There was no difference for GSTP1, GSTM1, and GSTT1 as well as for UGT1A1 and CYP3A4 polymorphism distributions between Hodgkin lymphoma patients and healthy controls. Patients carrying 1 or 2 UGT1A1*28 allele had a significantly (P < .05) better freedom from progression and time to treatment failure than those homozygous for the UGT1A1 TA6/TA6 allele. Multivariate prognostic analyses showed that the UGT1A1 polymorphism was as an independent prognostic parameter for all the studied endpoints, the wild-type homozygous UGT1A1 TA6/TA6 genotype being associated with a significantly worse prognosis than genotypes with at least one UGT1A1*28 allele (overall survival; relative risk [RR] = 2.54, 95% confidence interval [CI], 1.05-6.14; P = .04; freedom from progression, RR = 2.70, 95% CI, 1.37-5.31; P = .004; time to treatment failure, RR = 2.37, 95% CI, 1.28-4.40, P = .006). UGT1A1 polymorphism on TA repeats, which are thought to determine several anticancer drugs metabolism, influence Hodgkin lymphoma patient outcome.
Introduction
Approximately 20 000 new cases of Hodgkin lymphomas are diagnosed each year in North America and Europe, and approximately 80% of the patients are cured.1,2 One treatment strategy for improving cure rate has been to modify the intensity of therapy based on lymphoma and patient characteristics.3 However, in early-stage diseases that represent the majority of patients, this strategy is hampered by an increase of treatment-related toxicities leading eventually to death, which may represent a significant proportion of deaths observed in Hodgkin lymphoma patients. The challenge today is then to optimize the treatment for each individual patient by lowering acute toxicity and increasing efficiency but also to reduce the risk of late and redoubtable therapy-related complications, such as secondary cancers and cardiac complications.1,2
Germline polymorphisms in genes that code for enzymes involved in the pharmacodynamics of anticancer agents are common and may result in altered drug pharmacokinetics.4-7 Cytotoxic drugs and their metabolites are metabolized by enzymatic reactions classically divided into 2 main categories: the phase 1 enzymes, mediating oxidations, essentially represented by the cytochrome P450 family enzymes; and the phase 2 conjugating enzymes, mediating various modifications, such as glucuronidation, sulfo-conjugation, acetylation, and glutathione-conjugation.4,8,9 Intersubject variability of the activity of these enzymes is especially important for anticancer agents that have a narrow therapeutic index, with toxic doses close to active doses. We postulated that a better understanding of interpatient variability in drug-metabolizing enzyme activity, as determined by the polymorphisms of their genes, could help tailor an individual patient's treatment.
Hodgkin lymphoma patients are treated with homogeneous and widely accepted combination chemotherapy regimen, therefore representing an ideal population to assess the potential impact of drug-metabolizing enzyme polymorphisms. We report here our results on a cohort of 313 Hodgkin lymphoma patients in which the polymorphic variations of several drug metabolism enzymes were assessed for potential link with Hodgkin lymphoma patient prognosis. The choice of enzyme gene polymorphisms that were examined was guided by recent data in the literature showing that polymorphisms of both class II (GSTs, UGT1A1) and class I (CYP3A4) enzymes might play a role in hematologic malignancies.5-8 Our data demonstrate that UGT1A1 polymorphism does influence Hodgkin lymphoma outcome.
Methods
Patients
Peripheral blood lymphocytes from patients with Hodgkin lymphoma were collected before therapy between January 15, 1998, and June 6, 2002. Patients were included into ongoing European Organisation for Research and Treatment of Cancer/Groupe d'Etude des Lymphomes agressifs (EORTC/GELA) collaborative clinical trials (159 and 3 patients, respectively, in the H9 and H96 protocols),10-12 or were treated according to GELA recommendations (n = 151). Disease outcome data from patients were prospectively collected, and a panel of hematopathologists conducted a central pathology review (88% of the cases), without knowledge of the patients' outcome, to confirm Hodgkin lymphoma diagnosis.
Staging included complete history, searching for B symptoms, clinical examination, complete blood counts with differential, erythrocyte sedimentation rate, albumin serum level, lactate dehydrogenase serum level, chest radiograph, CT scan of the chest, abdomen, and pelvis, and bone marrow biopsy. Peripheral blood samples were obtained before any therapy at the time of initial diagnosis in all patients. The International Prognostic Score (IPS) validated in advanced Hodgkin lymphoma was used to categorize all patients.13 Written informed consent was obtained from all patients in accordance with the Declaration of Helsinki. The study has been approved by the Dijon University Hospital ethics committee, and was conducted according to institutional guidelines.
Blood samples for controls (n = 184) were obtained both from the Etablissement Français du Sang (Evry, France) (n = 154) and from the Service de Génétique, Institut Gustave Roussy (Villejuif, France; n = 30). Controls were known to be free of cancer (mandatory for collecting blood products in France).
Molecular genetic analyses
Genomic DNA was isolated from peripheral blood leucocytes using saline method with QIAamp DNA Blood Midi or Mini Kit (QIAGEN, Courtaboeuf, France) or High Pure PCR Template Preparation Kit (Roche Diagnostics, Mannheim, Germany). DNA samples were quantified using NanoDrop ND-1000 Spectrophotometer (NanoDrop, Wilmington, DE) and further adjusted to 15 ng/μL in nuclease free water.
CYP3A4 (1B) and GSTP1 (Ile105Val) SNP genotyping.
The CYP3A4 (c.-392A > G, rs2740574 dbSNP) and GSTP1 (c.313A > G, p.Ile105Val, rs947894 dbSNP) genotypes were determined using TaqMan MGB probes (Applied Biosystems, Foster City, CA) as follows: in a final volume of 10 μL, 30 ng DNA was added to a mix containing 1× TaqMan Universal PCR Master Mix without AmpErase uracil-N-glycosylase, and 1 μM both CYP3A4F and CYP3A4R primers (Table 1) together with 0.2 μM both CYP3A4*1B-G and CYP3A4*1B-A MGB probes (Table 1) or 0.25 μL 40× Assay Mix (Assay-by-Design, reference #SO1408679, Applied Biosystems) for CYP3A4*1B or GSTP1 I*B genotyping, respectively. The polymerase chain reaction (PCR) conditions were the following: 10 minutes of initial denaturation (92°C), then 15 seconds of denaturation (92°C) and 1 minute of annealing-extension (60°C) for 40 cycles. The fluorescence emission was recorded using ABI Prism 7700 Sequence Detection System (Applied Biosystems); endpoint plate read measurements were allowed to perform allelic discrimination using Sequence Detection System software (Applied Biosystems).
UGT1A1 TA repeat genotyping.
The number of TA repeats (n = 5-8) located 41 bp upstream of UGT1A1 initiation codon was determined by fragment length analysis of fluorescent PCR products obtained as follows: 30 ng of DNA was added to a mix containing 1× PCR buffer (final MgCl2 concentration, 1.5 mM), 0.2 μM each dNTP, 0.25 U of HotStarTaq DNA Polymerase (QIAGEN), and 0.4 μM both UGT1A1F and UGT1A1R primers (Table 1) in a final volume of 10 μL. Cycling conditions consisted of initial denaturation step (95°C, 15 minutes) followed by 45 cycles (94°C, 30 seconds; 55°C, 30 seconds; 72°C, 30 seconds) and final extension step (72°C, 10 minutes). PCR products were separated on an Applied Biosystems 3730 DNA Analyzer; the collected data were analyzed with the GeneMapper v3.5 software.
GSTM1 and GSTT1 dosage.
Both the GSTM1 and GSTT1 genes were quantified by quantitative multiplex PCR of short fluorescent fragment. In a final volume of 25 μL, 30 ng DNA was added to a mix containing 1 × PCR buffer (final MgCl2 concentration, 1.5 mM), 1 × Q-Solution, 0.2 mM each dNTP, 1.25 U of HotStarTaq DNA Polymerase (QIAGEN), 0.5 μM GSTM1F, GSTM1R, GSTT1F, and GSTT1R primers (Table 1), and 1 μM both GAPDHF and GAPDHR primers (GAPDH gene was used as reference gene). PCR conditions consisted of initial denaturation (95°C, 15 minutes), followed by 31 cycles (95°C, 45 seconds; 58°C, 45 seconds; 72°C, 45 seconds) and final extension step (72°C, 7 minutes). PCR products were separated, and the collected data were analyzed as described in the previous paragraph.
Statistics
The study was designed to have a 90% power to detect an absolute difference of 20% in the proportion of events between 2 groups: one corresponding to the more frequent polymorphism and the second group to the remaining patients, assuming that the overall proportion of events was 20%. The number of patients necessary was estimated for proportions of patients, with the more frequent polymorphism ranging from 50% to 90%. Situations with 90% of the patients in the more frequent polymorphism group were those requiring the highest number of patients. The size of the study was then fixed to 345 patients. This corresponds to a situation in which the most frequent polymorphism is found in 90% of the patients and is associated with a proportion of events of 18%, whereas the proportion of events in the other patients is of 38%.
Overall survival (OS), time to treatment failure (FFTF), and freedom from progression (FFP) were estimated from the first day of therapy to the time of the event. In FFTF relapses, progressions and death were considered as events, whereas in FFP, relapses and progressions were considered as events and deaths as censorship. Univariate survival analyses were performed with the Kaplan-Meier method, and comparisons of survival curves were tested with the log-rank test. Five-year event rates were estimated with 95% confidence intervals estimated with Rothman's method. Multivariate analysis used Cox proportional hazard regression model. Two models were used: one including the prognostic parameters and patient characteristics (13 covariates) and the 5 gene polymorphisms; and the second including the IPS score (coded with 4 dummy covariates (IPS > 1, lPS > 2, IPS > 3, and IPS > 4) and the 5 gene polymorphisms. Missing values were not replaced, and only cases without missing values were included. For each endpoint, all the covariates were entered in the multivariate analysis. Nonindependent prognostic covariates were eliminated through a backward elimination procedure. No adjustments were performed because of multiple testing. Statistical analyses were performed with SAS, version 8.2.
The most frequent genotypes of GSTP1, UGT1A1, and CYP3A4 polymorphism distribution were assessed for compatibility with the Hardy-Weinberg equilibrium rule (genotype could not be assessed with the techniques used for GSTT1 and GSTM gene analysis).
Results
From January 1998 to June 2002, 377 patients were registered in this study. Sixty-four patients were not included in the present analysis for the following reasons: insufficient amount or quality of DNA after extraction (22 patients), histologic diagnosis of Popema Lennert paragranuloma (10 cases) or benign hyperplasia (1 case), non-Hodgkin lymphoma (3 cases), HIV-positive serology (4 cases), and major therapy deviation (including 2 patients receiving radiotherapy alone and 22 patients who received unusual treatment regimens).
The present cohort consisted then of 313 patients with a median age of 32 years (range, 15-93 years), and approximately 75% of the patients had localized Hodgkin lymphomas (Table 2). All patients were treated with an anthracyclin-based chemotherapy (ABVD: doxorubicin, bleomycin, vinblastine and dacarbazine; EBVP: epirubicin, bleomycin, vinblastine, and prednisone; or BEACOPP: bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisone). At the time of analysis, the median follow-up was 4.1 years (range, 0.9-6.5 years), 53 (17%) patients had relapsed or progressed during or after initial chemotherapy, and 28 (9%) patients died. The causes of death were Hodgkin lymphoma (17 patients), treatment-related toxicity (6 patients), secondary malignancies (4 patients), and unknown (1 patient).
Polymorphism distributions
The repartition of GSTP1 (GSTP1 Ile105Val), UGT1A1, and CYP3A4 genotypes was consistent with Hardy-Weinberg equilibrium in the control cohort as well as in the Hodgkin lymphoma patients' cohort. For all the polymorphisms, distributions were not significantly different between patients and controls (Table 3).
UGT1A1 promoter region contains between 5 and 8 TA nucleotide repeats. As usually observed in the white population, a 6-TA allele, noted (TA)6, was the most common TA promoter number of repeats. When 7 TA repeats were present in the promoter region, the allele is noted (TA)7 or UGT1A1*28. Of the 313 patients studied for UGT1A1 polymorphism, 148 had the (TA)6 homozygous number of repeat (UGT1A1 TA6/TA6) and 161 had the presence of at least one 7-TA repeat (UGT1A1*28 allele), including 31 homozygous for UGT1A1*28 allele (or UGT1A1 77). Only 2 patients carried 5 TA repeats, (TA)5, in the UGT1A1 promoter region; none had more than 7 TA repeats. In all cases, the most frequent allele represented less than 90% of the patients, allowing these alleles to be tested for prognosis according to the statistical hypothesis of the study.
Patient outcome according to gene polymorphisms
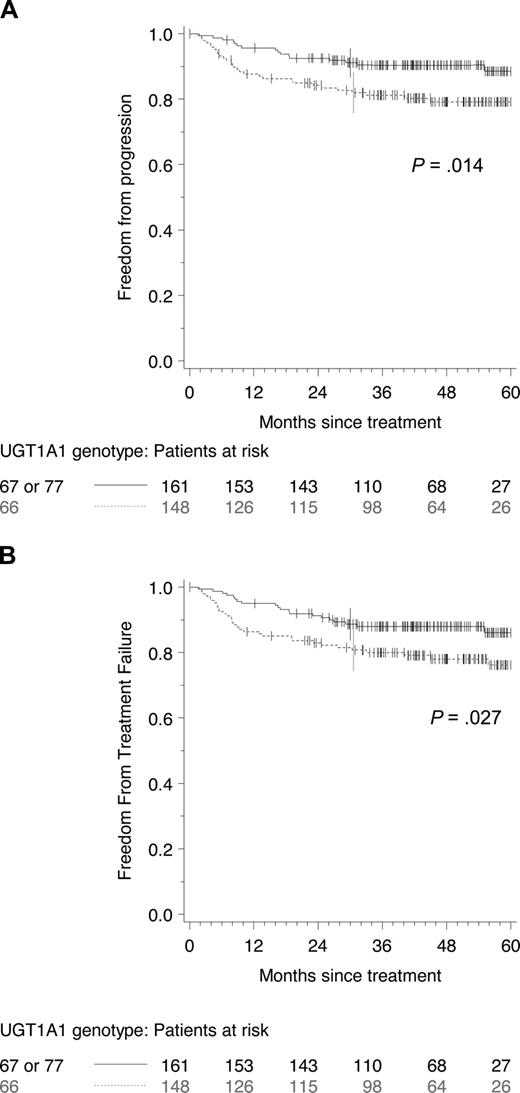
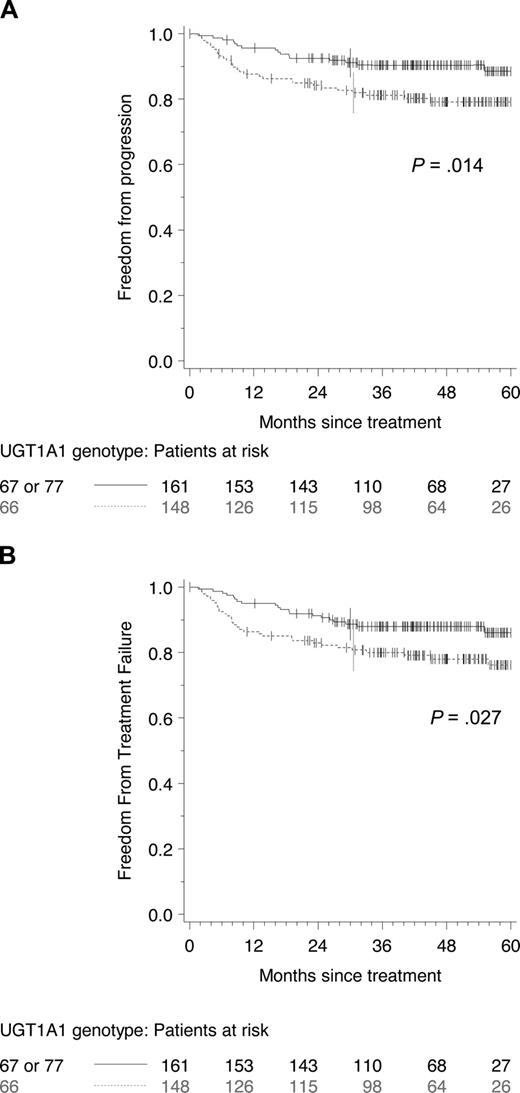
The only gene polymorphism found to influence FFTF and FFP was UGT1A1 (Table 4). The prognosis was similar in patients with one or 2 UGT1A1*28 alleles. However, only 31 patients had 2 UGT1A1*28 alleles, which constitute too small a group to make statistically meaningful separate analyses. Patients with one or2 UGT1A1*28 alleles experienced a significantly better FFP and FFTF survival compared with those with the (TA)6 homozygous genotype (P = .014 and .027, respectively, Figure 1). The association between UGT1A1 genotype and survival was, however, not significant (P = .18). Of note, a borderline relationship was observed between GSTT1 polymorphism and OS (P = .042), but this polymorphism was not associated with significant changes in FFP or FFTF (P = .63 and .41, respectively).
Freedom from progression according to UGT1A1 (TA) repeats, UGT1A1 TA6/TA6 (patients with (TA)6 wild-type phenotype TA6/TA6) and UGT1A1*28 (patients with at least 1 (TA)7 allele: 67 or 77). FFP (A) and FFTF (B) according to UGT1A1 (TA) repeats, UGT1A1 TA6/TA6 (patients with (TA) 6 wild-type phenotype: TA6/TA6) and UGT1A1*28 (patients with at least 1 (TA) 7 allele: 67 or 77).
Freedom from progression according to UGT1A1 (TA) repeats, UGT1A1 TA6/TA6 (patients with (TA)6 wild-type phenotype TA6/TA6) and UGT1A1*28 (patients with at least 1 (TA)7 allele: 67 or 77). FFP (A) and FFTF (B) according to UGT1A1 (TA) repeats, UGT1A1 TA6/TA6 (patients with (TA) 6 wild-type phenotype: TA6/TA6) and UGT1A1*28 (patients with at least 1 (TA) 7 allele: 67 or 77).
The impact of SNP on acute toxicities was assessed on 131 patients who were included in the EORTC/GELA trial H9. Four indicators were examined: interval between 2 consecutive cycles of chemotherapy more than theoretical interval plus 7 days, granulocyte count on day 1 of the next cycle less than 1 × 109/L, leukocyte count on day 1 of the next cycle less than 1.5 × 109/L, and platelet count on day 1 of the next cycle less than 100 × 109/L.
The proportion of patients with granulocyte or platelet toxicities on day 1 of chemotherapy was too small (< 1% and 1.5%, respectively) to perform meaningful analyses, but 13.7% of the patients had an increased interval for at least one cycle and 23.7% a decreased leukocyte count after at least one cycle. The number of patients was too small to reach a sufficient power for toxicity analyses. However, the proportion of toxicities seems to be increased in patients with UGT1A1 67 or 77 compared with UGT1A1 66 patients. Four of 51 (8%) patients with the (TA)6 homozygous genotype had an interval between 2 consecutive cures increased by more than 7 days compared with 14 of 80 (18%) patients with 1 or 2 UGT1A1*28 alleles (P = .12). The same trend was also observed for the leukocyte count on day 1 of the next cycle; less than 1.5 × 109/L with 10 of 51 (20%) patients with the (TA)6 homozygous genotype had interval between 2 consecutive cures increased by more than 7 days and 21 of 80 (26%) with 1 or 2 UGT1A1*28 alleles (P = .39). These data also suggest that patients with 1 or 2 UGT1A1*28 alleles may experience increased toxicity. None of the other SNPs was associated with toxicities with the variables analyzed.
Prognostic factor analysis
The main prognostic factors were analyzed for their influence on patients' outcome: FFP, FFTF, and OS. The prognostic value of the classic prognostic parameters was compatible with what is currently reported in the literature; erythrocyte sedimentation rate, age, B symptoms, and Ann Arbor stage were related to prognosis (Table 5). The IPS score was the most powerful single prognostic parameter.
When usual clinical parameters and polymorphisms were analyzed together in multivariate analysis, UGT1A1 and age were both prognostic and independent for all the endpoints analyzed (Table 6). The other independent parameters selected in the analysis were erythrocyte sedimentation rate for FFP and FFTF and B symptoms for OS.
When IPS and polymorphisms were analyzed together (Table 6), UGT1A1 polymorphisms were retained for FFP and FFTF (P = .01 for both), but not for OS (P = .08).
Discussion
We analyzed the polymorphisms of several drug-metabolizing enzymes involved in anticancer agent metabolism used for Hodgkin lymphoma therapy. Allelic distributions of these genes were similar to those previously reported in Western populations.4-23 We made the hypothesis that relevant polymorphisms previously reported for other studies in humans treated with chemotherapy could have an impact on the outcome of patients treated for Hodgkin lymphoma. This study has several limitations. One is related to a necessary tradeoff between the amounts of data needed to assess anticancer agent interactions with the size of the cohorts of patients who must be large enough to ensure a sufficient statistical power. A second point is the inability to investigate pharmacokinetics parameters separately for each drug in this cohort.
We did not find any association between GSTP1 (Ile105Val), GSTT1, GSTM1, CYP3A4, and UGT1A1 polymorphisms and occurrence of Hodgkin lymphoma. UGT1A1 polymorphism was significantly associated with FFP and FFTF but not GSTP1 (Ile105Val), GSTM1, GSTT1, and CYP3A4 polymorphisms. GSTT1 was marginally associated with OS on univariate analysis but did not remain as an independent prognostic parameter in multivariate analyses.
Two previous studies have explored whether GST germline polymorphisms could be related to Hodgkin lymphoma outcome. Both studies were performed in smaller cohorts (90 and 97 patients, respectively), and patients were treated with alkylating agents (mechlorethamine, vincristine, procarbazine, prednisone) or anthracyclin-based (ABVD) chemotherapies.5,14 A relation between GSTP1 Ile105Val alleles and freedom from treatment failure as well as OS were observed, but no relation was evidenced between GSTP1 Ile105Val alleles and relapse or remission rate.14 The discussion of the second paper14 ended with power considerations. The authors stated: “A cohort of 308 patients will be needed to confirm the prognostic difference between these groups at 80% power level.”14 Our study is compatible with these requirements, but we do not confirm these results. We found that GSTT1 phenotype was related to OS but not to disease-related endpoints (FFP and FFTF). This observation could be explained by an increased mortality unrelated to Hodgkin lymphoma in patients with GSTT1 null phenotype. However, the limited number of treatment-related deaths in the present study precluded any analysis regarding non-Hodgkin lymphoma-related mortality.
The glucuronidation of xenobiotics by UGT enzymes is one of the major metabolic pathways that renders the metabolic glucuronide products more easily excreted from the body via urinary and biliary tracts. Among the UGT1A exons, the exon 1 coding for UGT1A1 is the most extensively studied for genetic variations. UGT1A1 is responsible for the glucuronidation of bilirubin. Gilbert's syndrome is one of the more frequent hyperbilirubinemic syndromes resulting from UGT1A1 polymorphism and is associated with homozygosity for a dinucleotide (TA) insertion in the UGT1A1 promoter region, resulting in a variant allele (TA)7 (UGT1A1*28), which leads to a 70% reduction in UGT1A1 gene expression compared with the more common (TA)6 allele. Anthracyclins, Vinca alkaloids, and antitopo-isomerase agents all appear to be glucuro-conjugated during their metabolism, with differences between the UGT isoenzymes involved in their metabolism as it has been reported for epirubicin and doxorubicin.24-28 In our patient cohort, individual drug representatives of these classes are found in ABVD, BEACOPP, and EBVP regimens. In patients carrying the UGT1A1*28 allele, the glucuronidation of these anticancer agents may be reduced, therefore increasing the patient's exposure to the cytotoxic agents. As a result, the efficacy of the combination regimens appeared to be improved in those patients. Acute toxicity data were not prospectively collected in the patients treated outside the clinical trial. However, when assessing hematologic toxicities encountered in the 131 patients participating to the H9 trial, the proportion of one or 2 UGT1A1*28 carriers experiencing toxicity appeared to be greater, although not significantly. These data suggest that a link may exist between the efficacy and the toxicity of the regimen influenced by UGT1A1 polymorphisms.
In conclusion, our results showed that UGT1A1 polymorphism on the number of TA repeats is a prognostic factor in Hodgkin lymphoma treated with anthracyclin-based chemotherapy. The homozygous (TA)6 repeat in the promoter region of the UGT1A1 gene is associated with lower FFP, FFTF, and OS than genotypes with at least one (TA)7 repeat. This may be related to a slower drug excretion in patients carrying the UGT1A1*28 allele and will need to be confirmed with further pharmacokinetic analyses. Our findings need to be confirmed in an independent validation study incorporating a pharmacokinetic assessment of the impact of UGT1A1 polymorphisms on anticancer agents. However, given the importance of the difference in prognosis and the high frequency of these UGT1A1 polymorphisms, patient genotype at the initiation of treatment could be important to confirm in a prospective trial with an adaptation of anticancer agents to UGT1A1 genotype. The possible need for treatment adaptation according to patients' gene polymorphisms suggests that the concept of a unique standard dose of chemotherapy valid for all patients might be a myth. In a highly curable disease, such as Hodgkin lymphoma, further developments are still needed to optimize therapy to patient characteristics.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Michel Barrois for invaluable technical design, Coralie Briand for technical assistance, and Michel Henry Amar for his help on the H9 trial.
This work was supported by Centre Hospitalier Universitaire de Dijon (AO PHRC 1996) and Hospices Civils de Lyon (PHRC 2002).
Authorship
Contribution: V.R. and G.S. designed and performed research and wrote the manuscript; S.K. designed and performed research, analyzed and interpreted data, performed statistical analysis, and/or wrote the manuscript; O.C. collected data and wrote the manuscript; C.C. performed research and wrote the manuscript; P.B., F.M., J.G., and A.S. collected data; and G.L. designed research.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Vincent Ribrag, Laboratoire de Recherche translationnelle, Institut Gustave Roussy, 29 Rue C Desmoulins, 94805 Villejuif, France; e-mail: ribrag@igr.fr.