Abstract
von Willebrand factor (VWF) is a large multimeric adhesive glycoprotein with complex roles in thrombosis and hemostasis. Abnormalities in VWF give rise to a variety of bleeding complications, known as von Willebrand disease (VWD), the most common inherited bleeding disorder in humans. Current treatment of VWD is based on the replacement of the deficient or dysfunctional protein either by endogenous release from endothelial Weibel-Palade bodies or by administration of plasma-derived VWF concentrates. During the last years, several efforts have been made to optimize existing therapies for VWD, but also to devise new approaches, such as inducing endogenous expression with interleukin-11, administering exogenous recombinant VWF, or introducing the protein via gene delivery. Clearly, the efficacy of any strategy will depend on several factors, including, for example, the quantity, activity, and stability of the delivered VWF. The inherent complexity of VWF biosynthesis, which involves extensive posttranslational processing, may be limiting in terms of producing active VWF outside of its native cellular sources. This review summarizes recent progress in the development of different treatment strategies for VWD, including those that are established and those that are at the experimental stage. Potential pitfalls and benefits of each strategy are discussed.
Introduction
In 1926, Finnish physician Erik von Willebrand described an inherited bleeding disorder that was distinct from hemophilia A.1 It took another 30 years before the plasma protein that is central to the disease was identified, and this was eponymously named von Willebrand factor (VWF).2,3 Since then, much of the structure and function of VWF have been elucidated, and insights into the pathology of von Willebrand disease (VWD) have been continuously gained. This has naturally led to the development of improved treatment strategies for this sometimes life-threatening disorder. In this review, we discuss the different treatment modalities of VWD, focusing on both clinically established regimens and experimental strategies.
VWF
Although not recognized at that time, the bleeding problems originally described by von Willebrand illustrate the pivotal role of VWF in hemostasis. Indeed, this large, multimeric plasma protein is essential for the recruitment of circulating platelets at sites of vascular injury under high shear conditions. Furthermore, apart from sustaining platelet adhesion, VWF fulfills a crucial role in hemostasis by protecting coagulation factor VIII (FVIII) from rapid degradation, cellular uptake, or binding to the surface of activated platelets and endothelial cells. Indeed, when not bound to VWF, the plasma half-life of FVIII is reduced from 12 hours to 1 to 2 hours.
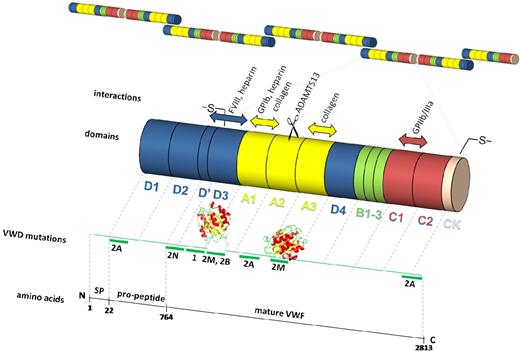
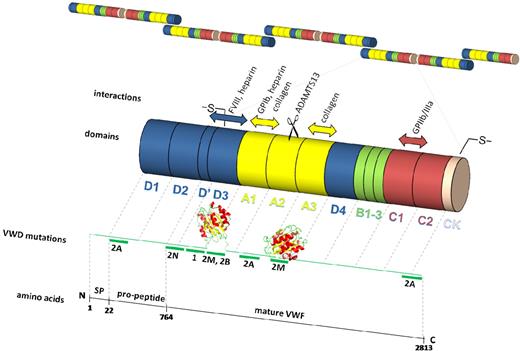
The multidomain structure of VWF (D1-D2-D′-D3-A1-A2-A3-D4-B1-B2-B3-C1-C2-CK)4,5 is fundamental to its function (Figure 1).6,7 At sites of vascular injury, VWF is able to bind to exposed fibrillar collagens via its A3 domain.8,9 This, and/or the high shear stress exerted on immobilized VWF, induces exposure of the VWF A1 domain because of loss of the shielding effect of the A2 and/or D′D3 domain.10-12 These conformational changes allow adhesion of platelets from the circulation via interactions with platelet glycoprotein (GP)Ibα. Because of the fast on- and off-rates of the GPIbα-VWF interaction,13-17 platelets are decelerated, allowing the establishment of more firm interactions between the platelet collagen receptors and the exposed subendothelium. Platelet adhesion is then followed by platelet aggregation, which involves interactions of activated platelet integrin αIIbβ3 with the RGD sequence found in fibrinogen and in the C1 domain of VWF.
Schematic representation of VWF. VWF is synthesized as a pre-pro-VWF that comprises a 22-residue signal peptide, a 741-residue propeptide, and the 2050-residue mature subunit. After removal of the signal peptide (SP), pro-VWF subunits associate in the endoplasmic reticulum in “tail-to-tail” dimers by the formation of disulfide bonds between the cysteine-rich carboxyl-terminal CK domains, after which dimers further multimerize by forming “head-to-head” disulfide bonds between the amino-terminal cysteine-rich D3 domains in the Golgi. The propeptide and the mature subunit form pro-VWF (2791 residues) consisting of 4 types of repeated domains as indicated. Crystal structures for the A16 and A37 domains are depicted. The main binding sites that are important for the hemostatic function of VWF are indicated together with the ADAMTS13 cleavage site. Major regions in which mutations have been found that are associated with VWD types 1 and 2 are also shown.
Schematic representation of VWF. VWF is synthesized as a pre-pro-VWF that comprises a 22-residue signal peptide, a 741-residue propeptide, and the 2050-residue mature subunit. After removal of the signal peptide (SP), pro-VWF subunits associate in the endoplasmic reticulum in “tail-to-tail” dimers by the formation of disulfide bonds between the cysteine-rich carboxyl-terminal CK domains, after which dimers further multimerize by forming “head-to-head” disulfide bonds between the amino-terminal cysteine-rich D3 domains in the Golgi. The propeptide and the mature subunit form pro-VWF (2791 residues) consisting of 4 types of repeated domains as indicated. Crystal structures for the A16 and A37 domains are depicted. The main binding sites that are important for the hemostatic function of VWF are indicated together with the ADAMTS13 cleavage site. Major regions in which mutations have been found that are associated with VWD types 1 and 2 are also shown.
The biosynthesis of VWF is restricted to endothelial cells and megakaryocytes and is complex, involving removal of the signal peptide and the propeptide, glycosylation, sulphatation, and multimerization. Endothelial VWF is secreted constitutively in the blood or in the subendothelial matrix. It may also be stored in Weibel-Palade bodies, from which it is released either on stimulation or via an unstimulated basal pathway.18 After biosynthesis in megakaryocytes, VWF accumulates in platelet α-granules and is only released via a regulated pathway. No matter what the cellular source, VWF activity is dependent on the extent and pattern of multimerization. Local secretion of ultra-large (UL, > 10 × 106 Da) VWF multimers from Weibel-Palade bodies and α-granules at sites of vascular injury strategically localizes highly active VWF to effect hemostasis. Nevertheless, because these UL-VWF multimers in the circulation are thrombogenic, their activity in the circulation must be tightly regulated; thus, they are rapidly digested on release to smaller multimers (≤ 10 × 106 Da or 40 monomers19 ) via cleavage of the Y1605-M1606 bond in the A2 domain by ADAMTS13 (a disintegrin and metalloprotease with thrombospondin type 1 repeats, 13).20-22 Once in the bloodstream, VWF multimers circulate with a half-life of 8 to 12 hours. The mechanisms by which VWF is cleared are not yet fully understood, but recent evidence suggests a role for macrophages in the removal of the VWF/FVIII complex in both the liver and spleen.23
VWD
Inherited quantitative and/or qualitative abnormalities in VWF are responsible for the bleeding disorder VWD. The prevalence of VWD, based on low VWF levels, may be up to 1%.24,25 However, the incidence of those requiring treatment is in the range of 0.002% to 0.01%.26 VWD is most commonly associated with mucosal hemorrhages, such as epistaxis, menorrhagia, and bleeding from the gums and gastrointestinal tract. Prolonged bleeding after trauma to skin or mucous membranes is also characteristic, especially during or after surgery. The most severely affected VWD patients have concomitant low levels of FVIII and are at risk of more severe and spontaneous deep tissue bleeds and hemarthroses.
The identification of more than 250 VWF gene mutations associated with all the types of VWD (database: www.sheffield.ac.uk/VWF) provides useful insights into the mechanisms underlying qualitative and quantitative VWF defects. However, the current clinical classification of VWD27,28 is not based on genetic defects but rather was designed for the purposes of optimizing treatment strategies (Table 1). Thus, a partial or complete quantitative deficiency of VWF results in so-called type 1 and type 3 VWD, respectively, whereas type 2 VWD is caused by qualitative defects.
Type 1 VWD is characterized by mild to severe quantitative defects of VWF (associated mostly with parallel decreases in FVIII levels) and accounts for 60% to 80% of all cases of VWD. Levels of VWF and FVIII are significantly lower in persons with blood group O; thus, the diagnosis of type 1 VWD must be made cautiously. Recent large studies in Europe and Canada have revealed that the majority of type 1 VWD is associated with mutations within VWF.29-31 The more severe forms of VWD with a high penetrance are associated with dominant, mostly single amino acid missense mutations in the D3 domain, that result in reduced intracellular transport of dimeric pro-VWF, or more rapid clearance of the protein from the circulation (for a review, see Nichols et al32 ).
Subtype 2A VWD, the most common qualitative variant, usually with an autosomal dominant inheritance pattern, is characterized by a decreased platelet-dependent function of VWF because of the loss of large and intermediate multimers. This is caused by mutations in either the propeptide or cystein knot domain, leading to defective assembly, and/or by mutations in the A2 domain that increase the susceptibility to proteolysis by ADAMTS13.33
Subtype 2B VWD, usually inherited as an autosomal dominant trait, is associated with increased and often spontaneous binding of VWF to platelet GPIbα. The molecular defect resides within the A1 domain of VWF and is the result of various missense mutations.34 High molecular weight multimers are lost from plasma, as VWF binding to platelets on the one hand facilitates proteolysis by ADAMTS13, and on the other hand results in faster clearance of the platelet-VWF complexes. This gives rise to thrombocytopenia35 and explains the apparently paradoxical bleeding diathesis in these “gain-of-function” mutations.
Subtype 2M VWD is an autosomal dominant variant that displays decreased VWF function in the presence of a (near) normal multimeric distribution. Most of the associated mutations are within the A1 domain, causing impaired binding to GPIbα, without affecting multimer assembly.34 To date, one mutation in the VWF-A3 domain has been reported to result in defective VWF binding to collagen.36
Subtype 2N VWD, an autosomal recessive disorder characterized by a decrease in the affinity of VWF for FVIII, is caused by approximately 20 homozygous or compound heterozygous missense mutations in the D′ or D3 FVIII binding domain. When there is a severe reduction in FVIII levels, type 2N VWD resembles mild or moderate hemophilia A.
Type 3 VWD is the most severe form of the disease, inherited in an autosomal recessive manner, with a prevalence ranging from 0.5 to 5 cases per million. It is caused by defective VWF synthesis, resulting in virtually complete absence of VWF, and a consequent severe reduction in circulating levels of FVIII. Almost 90 distinct mutations,34 associated with the type 3 phenotype, are scattered over the entire VWF gene and include partial or total deletions, small insertions, exon/intron boundary splice site mutations, which result in exon skipping or aberrant splicing, missense mutations, and frameshift mutations.
Acquired VWD is a rare syndrome that mimics the congenital form of VWD but occurs in persons with no personal or family history of bleeding. Several underlying diseases have been associated.37 These are most commonly myeloproliferative and lymphoproliferative disorders, where increased numbers of platelets may bind and clear the highest multimers. Autoimmune and cardiovascular disorders have also been associated. In situations with ultra-high shear stresses, particularly in stenosed areas, high multimer VWF cleavage by ADAMTS13 may be excessive, leading to reduced levels of active VWF.
VWF to the rescue
In VWD patients who require treatment, the main goal is to replace the deficient or dysfunctional VWF protein, thereby restoring the hemostatic balance. At present, 2 primary strategies are used to stop spontaneous acute hemorrhages and to prevent major bleeding during invasive or surgical procedures: administration of desmopressin and infusion of plasma-derived VWF/FVIII concentrates. However, research continues, with the goal of developing safer and more effective preventative and therapeutic strategies. The use of interleukin-11, the introduction of standardized recombinant VWF preparations and advances in gene-based delivery approaches are some of the more promising alternatives undergoing active investigation, which may broaden the panel of future treatment modalities of VWD (Table 2).
Current treatments
Desmopressin
Desmopressin (1-deamino-8-D-arginine vasopressin [DDAVP]) is a synthetic analog of vasopressin that was found to raise VWF levels without the side effects of vasopressin.38,39 DDAVP induces exocytosis of Weibel-Palade bodies by binding to endothelial V2 receptors and activating cyclic adenosine monophosphate-mediated intracellular signaling pathways.40 An intravenous infusion of DDAVP (usually at a dose of 0.3 μg/kg diluted in 50 mL saline over 30 minutes) typically increases plasma levels of VWF 3- to 5-fold over baseline within the first hour after administration.
Concomitantly, DDAVP also increases plasma levels of FVIII. The precise mechanism of this rise is still poorly understood. The uncertainty relates particularly to the fact that the site of release of FVIII remains unclear, although Jacquemin et al suggest that lung microvascular endothelial cells might be an extrahepatic, DDAVP-releasable source.41 Moreover, when FVIII and VWF are expressed together in endothelial cells, VWF targets the FVIII to Weibel-Palade bodies, from which both can be secreted acutely in response to agonists.42
Because high VWF levels are generally maintained for only 6 to 8 hours, DDAVP treatment must be repeated every 12 to 24 hours, depending on the type and the severity of the bleeding. Unfortunately, repeated use of desmopressin frequently results in a refractory response to subsequent doses.43
Desmopressin administration is the treatment of choice for VWD type 1 because functionally intact VWF is present in endothelial storage granules of these patients.44,45 However, it is not effective in VWD type 3 or in severe cases of VWD type 1, yields a variable response in types 2A and 2M, and is contraindicated in patients with VWD type 2B because of the possibility of inducing transient thrombocytopenia. In view of the range in responses to DDAVP, a test infusion is recommended in all VWD patients (except type 2B). For poor responders, alternative treatments, such as plasma concentrates, rhIL-11, or rVWF may be considered. The variability in DDAVP response is not well explained, although several mechanisms have been proposed, including VWF mutations,46,47 causing differences in intracellular transport, secretion, and multimer composition of VWF48 and expression of A-antigen.49
The main advantages of DDAVP are its low cost, ready availability, and suitability for self-administration. It is preferred over plasma concentrates, which carry the risk of transmission of blood-borne infections. Nonetheless, DDAVP may cause mild tachycardia, headache, facial flushing, as well as hyponatremia, particularly in children. Franchini et al also described an episode of deep vein thrombosis after DDAVP administration in a VWD patient undergoing orthopedic surgery,50 and, although not reported in patients with VWD, DDAVP has also been implicated in myocardial infarction and stroke.51,52
VWF/FVIII concentrates
Current treatment of VWD patients who respond unsatisfactorily to DDAVP relies on transfusion therapy using VWF products manufactured from pooled human plasma. This furthermore is the only option for VWD type 3 patients because they lack a releasable pool of VWF. Because patients with VWD type 2 secrete a qualitatively abnormal VWF protein, DDAVP response is often minimal. In addition, patients in whom DDAVP is contraindicated, such as those with VWD type 2B, must be treated with plasma products. A wide variety of plasma concentrates is commercially available, but product composition differs significantly, depending on the purification scheme.53,54 Originally developed for hemophilia A, some products have a high proportion of FVIII (eg, Alphanate [antihemophilic factor]; Alpha Therapeutic, Los Angeles, CA), whereas other, newer formulations are essentially void of FVIII (eg, Wilfactin [VWF]; LFB, Les Ulis, France). Furthermore, the relative content and activity of VWF vary considerably, with many concentrates lacking high-molecular-weight VWF resulting from proteolysis during purification, which probably impacts on their overall effectiveness.53,54
Because preparation of these concentrates requires the pooling of large quantities of human fresh-frozen plasma, untreated preparations that are/were unscreened and/or untreated carry a significant risk of transmitting blood-borne (viral) pathogens. Awareness of this problem became dramatically evident when it was recognized in the mid-late 1980s that up to 90% of severe hemophilia A patients had become seropositive for human immunodeficiency virus and hepatitis virus B and C after being treated with contaminated plasma products.55,56 Fortunately, during the last decades, major improvements have been made in the preparation of contaminant-free products. Using various techniques, including nanofiltration, solvent/detergent, and/or heat treatments, viral transmission has become less of an issue. Nevertheless, even adequately processed blood preparations are deemed to always carry a low but real risk of transmission of pathogens because current screening tests cannot exclude all pathogens. Nor can we fully anticipate what the future will hold, in terms of new blood transfusion-transmitted agents.57 It is therefore probable that plasma concentrates will never be entirely risk-free of transmitting infections, and alternative approaches are well worth pursuing.
Ideally, the concentrate of choice would be viral-inactivated and contain high amounts of clinically active, high-molecular-weight VWF multimers, as well as FVIII. Levels of FVIII will, however, be important to monitor, particularly in patients requiring repeated concentrate injections because sustained high FVIII levels may increase the risk of deep vein thrombosis.58 In that respect, it is important to appreciate also that the pharmacokinetics of FVIII levels after infusion of concentrates varies according to the preparation, and higher FVIII levels will be achieved more rapidly when FVIII is part of the concentrate. Thus, in type 3 VWD, hemostatic FVIII levels are reached only after 6 to 10 hours when concentrates lacking FVIII are used. Hence, this type of concentrate has limited utility in cases of acute, life-threatening bleeding episodes or emergency surgical procedures unless they are used in combination with exogenous recombinant FVIII. On the other hand, although VWF concentrates containing large quantities of FVIII may be preferred in emergency situations, their continued use in other situations is not recommended and maintenance with FVIII-deficient VWF concentrates (or recombinant VWF preparations) may be safer.
Clinical studies obtained over the last 20 years have demonstrated that currently used VWF/FVIII concentrates (most commonly Haemate P [antihemophilic factor]/Humate-P [antihemophilic factor]; ZLB Behring, Marburg, Germany) in patients with VWD are effective at stopping most bleeding episodes and preventing excessive blood loss during surgical procedures. When hemorrhage persists despite high VWF/FVIII levels, administration of platelet concentrates can be helpful, emphasizing the important role of platelet VWF in maintaining primary hemostasis.59-61 Platelet concentrates are effective, particularly in patients with type 3 VWD, probably because of their role in transporting VWF to sites of vascular injury where they secrete actively prothrombotic VWF.
Investigational treatments
Interleukin-11
Originally used to restore platelet counts after chemotherapy, recombinant human interleukin-11 (rhIL-11), a gp-130 signaling cytokine with hematopoietic and anti-inflammatory activity, was found to induce a gradual and sustained increase in VWF and FVIII levels in mice,62 dogs,63 and humans64 for as long as the drug was given. This is in contrast to DDAVP, which yields a rapid but transient increase in VWF/FVIII that becomes refractory to repeated infusions.
Side effects associated with rhIL-11 are generally mild or moderate and are easily managed. During recent phase 2 clinical trials, hypertension, fluid retention, and hypokalemia64,65 were reported as adverse events on infusion of rhIL-11 in patients with mild VWD. In cancer patients, the use of rhIL-11 has been reported to increase the susceptibility to transient atrial arrhythmias.66,67
Interestingly, DDAVP administration during rhIL-11 treatment still results in the release of VWF from the Weibel-Palade bodies, suggesting that the mechanisms for VWF increase differ. These mechanisms have not yet been fully clarified, although IL-11 up-regulates VWF mRNA accumulation in dogs and humans, but not in mice.62 Nonetheless, the different mechanisms indicate that rhIL-11 could be used in combination with DDAVP to treat mild (quantitative) VWD, for example, to overcome DDAVP tachyphylaxis and in cases where prolonged high VWF levels are required. On the other hand, if proven safe in future clinical trials, the use of rhIL-11 will be of particular value for those patients who are refractory or unresponsive to DDAVP and/or who prefer a potentially safer treatment alternative to plasma-derived products.
Future treatments
In vitro–produced VWF
To circumvent the risks related to the use of blood as a source of therapeutic VWF, production of a VWF product by in vitro cell culture is an appealing alternative. Endothelial cell cultures, such as human umbilical vein endothelial cells and blood outgrowth endothelial cells (BOECs),68 appear to be good candidates because they have the natural capacity to correctly synthesize VWF. Yet, these primary human cell lines are not ideally suited for large-scale production of VWF. Interestingly, the cellular machinery responsible for correct assembly of VWF multimers is not unique to endothelial cells and megakaryocytes. VWF multimers can be properly formed in vitro by many cell types in low pH conditions.69 The propeptide itself seems to be the driving force for multimerization, possibly by providing noncovalent, intermolecular interactions between D1-D2 domains of different VWF subunits70 and by acting as an oxido-reductase during multimerization.71,72 As a consequence, efficient VWF biosynthesis has been observed in many different types of heterologous cells, including COS, CHO, 3T3, CV-1, AtT-20, RIN 5F, MDCKII, and HEK293 cells.73
Indeed, a CHO cell–derived standardized recombinant VWF (rVWF) preparation for treatment of VWD is currently under development. This rVWF was initially produced in CHO cells coexpressing furin for proper propeptide removal.74 However, the protocol has been adapted, such that rVWF is coexpressed with recombinant FVIII in the cells. Propeptide cleavage occurs subsequently by exposing rVWF to recombinant CHO cell–derived furin. Preclinical studies showed that furin-processed rVWF has properties comparable with plasma-derived VWF in a variety of in vitro functional assays. One exception is that rVWF contains more intact multimers as it has not been exposed to ADAMTS13 processing.75,76 This apparently does not markedly alter the function of the VWF, at least in vitro. Pharmacokinetic properties of rVWF were investigated in murine and canine models of VWD where a slightly longer half-life for rVWF was observed in VWF knockout mice compared with plasma-derived VWF.75-77 Preliminary data show that the half-life of recombinant VWF can be further increased by PEGylation or by modifying the glycosylation pattern of VWF, although these modifications significantly reduce the functional activity of VWF.78,79 On the other hand, a prolonged half-life of VWF and concomitant increase of the half-life of coadministered FVIII might be beneficial for patients with hemophilia A.
Because pure rVWF preparations contain only VWF, concomitant administration of FVIII for VWD patients will be necessary for the treatment of acute bleeding and for the prevention of excessive bleeding during major surgery. Future clinical studies with rVWF will reveal its efficacy and, thus, its potential as an alternative to plasma VWF concentrates.
Gene therapy
Patients with severe bleeding phenotypes (VWD type 3 and some severe cases of types 1 and 2) not only have the looming threat of a serious hemorrhage but are also confronted with more general quality of life challenges that impact on education, work, social activities, and family life.80 Frequent hemarthroses often lead to arthropathies that limit the patient's mobility and independence.81,82 Recurrent epistaxis can be severe enough to cause anemia in children. Patients with frequent gastrointestinal or other bleeding episodes may require treatments every day or every other day, restricting work and social activities. Menorrhagia also has a negative impact on overall life activities.83,84 The daily management of symptoms, the unpredictable and potential life-threatening nature of bleeding episodes, and concerns about the future are furthermore associated with anxiety and depression.80 Overall, it is clear that treatment strategies that are preventative rather than reactive, with a sustained effectiveness, would be particularly valuable for these persons.
The benefits of long-term treatment of VWD can be deduced from the limited number of prophylaxis studies. Although long-term prophylaxis is not as common for VWD as for hemophilia A (probably because of an underestimation of the number of patients who would benefit85 ), recent data from Swedish surveys are encouraging.86,87 A substantial number of patients who received VWF concentrates over long periods of time exhibited fewer bleeding episodes, and all reported an improved quality of life. Furthermore, in children who began long-term prophylaxis before the age of 5, none developed arthropathy. Finally, in an Italian study, long-term prophylaxis stopped bleeding in VWD patients and reduced days in hospital.88
Gene therapy for VWD offers the potential of a long-term, if not lifelong, correction of VWF deficiency, which would dramatically change the patient's personal comfort and quality of life. Instead of repetitive, on-demand replacement of the deficient/defective protein, a permanent correction of the underlying genetic defect would ideally cure the disorder. Indeed, VWD is a good candidate for gene therapy, as it is a monogenic disease. Moreover, VWF is secreted into the circulation; thus, organ- or tissue-specific targeting is not required. Although several safety and ethical issues remain to be resolved in the field of gene therapy, interest in using this approach for VWD is increasing.68,89-92
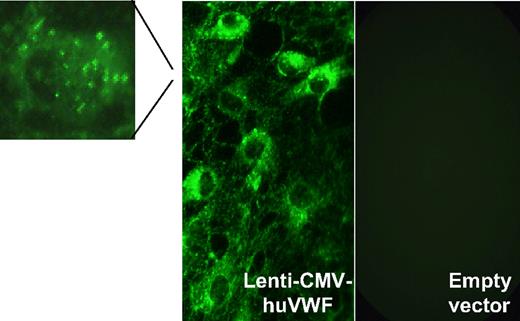
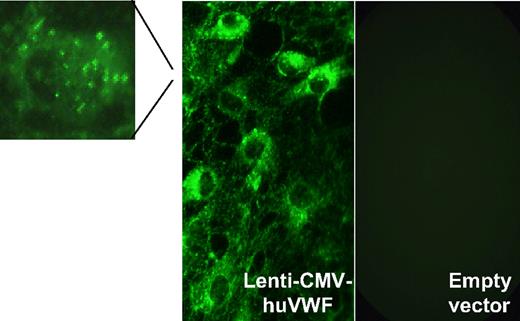
In the past, the development of gene therapy for VWD was viewed as a daunting task, especially because of the large size of the VWF cDNA (8.4 kb), which impeded efficient incorporation into integrating viral vectors. Moreover, as mentioned earlier, the VWF protein undergoes several complex intracellular processing steps, all of which are required to yield a functional protein. Nonetheless, these challenges are being met. We recently demonstrated the feasibility of accommodating full-length VWF into a lentiviral vector (Figure 2).68 With this vector, expression of functional VWF could be completely restored in BOECs that were isolated from dogs with VWD type 3. It remains to be seen whether such genetically engineered autologous BOECs can be engrafted in vivo into VWD donors for long-term delivery of VWF. However, promising proof-of-principle experiments are available for the treatment of hemophilia A in animal models.93,94
Expression of transgene-encoded VWF in VWD BOECs after lentiviral transduction. VWD BOECs were isolated from dogs with VWD type 3 and transduced with lentiviral vectors encoding full-length human VWF. VWF immunostaining revealed high concentrations of VWF present in both the cytoplasm and Weibel-Palade bodies (magnification) of transduced VWD BOECs (Lenti-CMV-huVWF) but not in VWD BOECs transduced with empty lentiviral particles (empty vector). Reprinted from De Meyer et al68 with permission.
Expression of transgene-encoded VWF in VWD BOECs after lentiviral transduction. VWD BOECs were isolated from dogs with VWD type 3 and transduced with lentiviral vectors encoding full-length human VWF. VWF immunostaining revealed high concentrations of VWF present in both the cytoplasm and Weibel-Palade bodies (magnification) of transduced VWD BOECs (Lenti-CMV-huVWF) but not in VWD BOECs transduced with empty lentiviral particles (empty vector). Reprinted from De Meyer et al68 with permission.
With the availability of a lentiviral tool for VWF gene transfer, another interesting gene-based option to correct VWD would involve direct in vivo transduction after systemic vector administration. One drawback might be that lentiviral vectors predominantly target the liver; thus, the transgene expressing VWF would reside in liver cells. However, using the technique of hydrodynamic gene transfer in a murine model of severe VWD, we and others demonstrated that the liver indeed is capable of producing VWF containing the full range of multimers (Figure 3).90,92,95 Transgene-encoded, liver-expressed VWF could restore FVIII levels to normal and, most importantly, reversed the prolongation of the tail bleeding time.90,92,95 Furthermore, in a FeCl3-induced thrombosis model, there was restoration of the platelet plug-forming capacity, which is a major hemostatic function of VWF.92,96
Multimer analysis of transgene encoded VWF expressed in the liver. Multimer analysis was performed on a plasma sample that was isolated from a VWD type 3 mouse 3 days after liver-directed hydrodynamic gene transfer of murine VWF cDNA (liver-expressed VWF). For comparison, the multimer pattern of plasma VWF from wild-type mice is shown (normal murine plasma [NMP]). Adapted from De Meyer et al92 with permission.
Multimer analysis of transgene encoded VWF expressed in the liver. Multimer analysis was performed on a plasma sample that was isolated from a VWD type 3 mouse 3 days after liver-directed hydrodynamic gene transfer of murine VWF cDNA (liver-expressed VWF). For comparison, the multimer pattern of plasma VWF from wild-type mice is shown (normal murine plasma [NMP]). Adapted from De Meyer et al92 with permission.
When VWF is expressed in heterologous cells, one has to consider that proper digestion by ADAMTS13 might be impaired. Independent of the cellular source, circulating VWF will most probably be cleaved normally in the bloodstream. However, on secretion itself, specific VWF-endothelial interactions may facilitate digestion of UL-VWF, such as the anchoring of released VWF to the endothelial surface by αvβ397 and P-selectin.98 Hence, when VWF is expressed in nonendothelial cell types such as liver cells, efficient processing of VWF by ADAMTS13 could be hampered. Interestingly, however, in contrast to endothelial cells, liver cells do not seem to express UL-VWF multimers92 (and S.F.D.M. and K.V., unpublished data, September 2008). This could be related to differences in cellular machinery, such as the absence of a regulated secretory pathway in hepatocytes. Therefore, even in the absence of cleavage by ADAMTS13, liver-expressed VWF would not probably pose a thrombotic risk related to the circulation of UL-VWF multimers.
This is in accordance with the observed normal FeCl3-induced thrombus formation and the absence of spontaneous thrombotic complications in VWF knockout mice after gene transfer, even when liver-expressed VWF levels were 10-fold higher than in wild-type animals.92 Further studies using VWD animal models will provide more insight into the long-term therapeutic value of this liver-targeted approach.
These first steps toward gene therapy for VWD are only the tip of the iceberg. It is clear that, for each target disease, including severe VWD, a careful risk-benefit assessment of gene therapy and other therapeutic options will be required. With the current status of gene therapy, it is common sense that only the most severely affected patients (VWD type 3) would be considered for a gene-based treatment approach. Although VWD is not life-threatening and there are other available treatments, VWD, similar to hemophilia, is indeed an ideal candidate for gene therapy. However, in hemophilia, an increase of 1% to 2% in circulating levels of the deficient clotting factor can significantly modify the bleeding diathesis. Higher levels of VWF will most probably be needed to achieve hemostasis in VWD. Future studies, preferably in larger animal models of severe VWD such as dogs or pigs, will undoubtedly shed more light on this issue and further expand our knowledge on the possibilities and limitations of VWD gene therapy. As the field of gene therapy is making slow but steady progress, with promising results in a range of diseases, the tide of public opinion is shifting. Despite the isolated adverse events related to gene therapy, there is a large number of patients whose quality of life has been dramatically improved by having received gene therapy.99 Once issues on safety and efficiency are resolved, the appeal of treating severe VWD patients via gene therapy approaches will surely lead to its approval and wide use.
Anti-VWF alloantibodies
Alloantibodies directed against the substituted VWF may complicate the treatment of patients with VWD type 3, particularly in those patients with large VWF gene deletions.100 These antibodies may severely reduce the effectiveness of administered VWF, either by interfering with the functional domains of VWF or by reducing its half-life in the circulation. However, compared with FVIII, the development of inhibitory antibodies against VWF is quite rare (10%-15% of patients with VWD type 3), with only a few cases being described. Exceptionally, administration of VWF/FVIII concentrate to patients with VWF antibodies can induce life-threatening anaphylaxis.101 When such patients fail immune tolerization, on-demand treatment with recombinant FVIII or recombinant activated FVII helps to control bleeding. Antibody induction may also be limiting the applicability of gene therapy for VWD. Because VWF also is normally present in platelets, one could consider a gene therapy approach where VWF is only targeted to platelets, thereby minimizing exposure to the immune system. Such an approach has already been used successfully for FVIII in hemophilia A mice.102,103 However, whether platelet VWF alone would be sufficient for normal hemostasis is questionable, based on studies in chimeric pigs where platelet VWF alone did not correct the bleeding time or thrombus formation.104
VWD in developing countries
It is interesting to note that most of the current information on the biology and management of VWD is deduced from studies conducted in developed countries with a predominantly white population. Data on the epidemiology and management of VWD in developing countries are limited,105-107 although approximately 80% of the world's population lives in these countries. Whether the development of new treatments will add to better management of VWD patients in these countries is hard to predict. Efficient use of currently available treatments (DDAVP and plasma concentrates) in developing countries is hampered by budgetary issues and by lack of proper awareness and/or training in the management of bleeding disorders in general. Thus, whereas much less expensive medication for VWD would certainly help where VWD therapy is presently unaffordable, it may only reach patients in an environment of optimal awareness of the disorder. With the cost burden of plasma concentrates already being very high in developing countries, it is doubtful whether new treatments, such as the use of recombinant factors (IL-11 or VWF) or gene therapy, will help to reduce this burden.
Conclusions
In conclusion, more than 80 years have passed since Erik von Willebrand described the bleeding disorder that bears his name. In those early days, treatment strategies were far from adequate, and patients with severe forms of VWD were crippled before adulthood and had shortened life expectancy. Illustratively, Dr von Willebrand's first case, a 5-year-old girl, bled to death during her fourth menses at the age of 13. Over the past 50 years, our understanding of the bleeding disorder has steadily increased, resulting in dramatic improvements in the management of VWD. It will be exciting to unravel more aspects of VWF biology and to use this new knowledge in the optimization and design of treatments for VWD. Current strategies, using DDAVP or plasma concentrates, give satisfactory results, and alternative treatment options can further improve or at least broaden the panel of VWD treatment modalities. Whether the VWF molecule that comes to the rescue is endogenous, exogenous, recombinant, or even transgene encoded, it will always serve the same goal in VWD: to restore the functional deficiency of VWF and to rapidly and effectively correct the associated hemostatic abnormalities.
Acknowledgments
The authors thank Prof P. M. Mannucci (A. Bianchi Bonomi Hemophilia and Thrombosis Center, Milan, Italy) and Dr E. M. Conway (Katholieke Universiteit Leuven, Leuven, Belgium) for careful reading of the manuscript and helpful criticism.
S.F.D.M. and K.V. are postdoctoral fellows of the Fonds voor Wetenschappelijk Onderzoek, Vlaanderen, Belgium.
Authorship
Contribution: S.F.D.M., H.D., and K.V. wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Simon F. De Meyer, Laboratory for Thrombosis Research, Interdisciplinary Research Center, KU Leuven Campus Kortrijk, E Sabbelaan 53, 8500 Kortrijk, Belgium; e-mail: simon.demeyer@kuleuven-kortrijk.be.

![Figure 3. Multimer analysis of transgene encoded VWF expressed in the liver. Multimer analysis was performed on a plasma sample that was isolated from a VWD type 3 mouse 3 days after liver-directed hydrodynamic gene transfer of murine VWF cDNA (liver-expressed VWF). For comparison, the multimer pattern of plasma VWF from wild-type mice is shown (normal murine plasma [NMP]). Adapted from De Meyer et al92 with permission.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/113/21/10.1182_blood-2008-10-165621/6/m_zh89990936220003.jpeg?Expires=1767350958&Signature=j8pcWeuMkuN1UH9CK0dXwBSoieJJKJ6r0tIBy9xbB~4xPAb5KGY-3IlM5qk0U0nwFOIOLpUPuonaN3aJg8-pxo8kOdVBRev3ceSk1PZ-yksZCPfv6dVxZIjrCRKueCtlubH8KYBAHPqzTZgoARlaMf-LnPcaVK7iBHab90hrNhRzvLb6tOrdPUoGVGuxyCBpuUboEF9LbKKxih7P74DuU-BIRuhcYxGt3H9fJ8fYRU8-EksQv18ed0XaIVQaGg11yvaxQoeS-58gtJ7OAFSTZ8d-Hk8vMs9l6IMC9rHU886rr0KdfllNB3qDluUY1vy16~Qj29f6AJoXktRX1sE-UQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Figure 3. Multimer analysis of transgene encoded VWF expressed in the liver. Multimer analysis was performed on a plasma sample that was isolated from a VWD type 3 mouse 3 days after liver-directed hydrodynamic gene transfer of murine VWF cDNA (liver-expressed VWF). For comparison, the multimer pattern of plasma VWF from wild-type mice is shown (normal murine plasma [NMP]). Adapted from De Meyer et al92 with permission.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/113/21/10.1182_blood-2008-10-165621/6/m_zh89990936220003.jpeg?Expires=1767350959&Signature=VeYjNmkAQj3IcdM~FFdcuriJlhEkvaCkcfpPQ8qivs8ZcX56NSEhzJLXogAfn3t7CsA907zJzar~HLbvP4UztMyQGWQzAIKEsjfEUXbpVRs9AKZVEDlw~Kwm9~GXd8pnCsSqoUUdEC3VGy8WWt5Qp9bQkghYGxGa5weP~7Azy-5DljFXNqd3u5ss-A3zZDy~bG8QKl9As-WF5Rkto~fKe-udHN9wTozntfkq5ZDPP5yogHBLTm~6orsmvSkv7avwSZrVPIDTyE4vMP1wk7tmGf8Cr1PeKZP58c2EDWyxjdhvScP1M1FPLTvgcl3Rr~rpGTAK--R3kVKE5~BsHPYnxA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)