Abstract
Protamine sulfate is a positively charged polypeptide widely used to reverse heparin-induced anticoagulation. Paradoxically, prospective randomized trials have shown that protamine administration for heparin neutralization is associated with increased bleeding, particularly after cardiothoracic surgery with cardiopulmonary bypass. The molecular mechanism(s) through which protamine mediates this anticoagulant effect has not been defined. In vivo administration of pharmacologic doses of protamine to BALB/c mice significantly reduced plasma thrombin generation and prolonged tail-bleeding time (from 120 to 199 seconds). Similarly, in pooled normal human plasma, protamine caused significant dose-dependent prolongations of both prothrombin time and activated partial thromboplastin time. Protamine also markedly attenuated tissue factor-initiated thrombin generation in human plasma, causing a significant decrease in endogenous thrombin potential (41% ± 7%). As expected, low-dose protamine effectively reversed the anticoagulant activity of unfractionated heparin in plasma. However, elevated protamine concentrations were associated with progressive dose-dependent reduction in thrombin generation. To assess the mechanism by which protamine mediates down-regulation of thrombin generation, the effect of protamine on factor V activation was assessed. Protamine was found to significantly reduce the rate of factor V activation by both thrombin and factor Xa. Protamine mediates its anticoagulant activity in plasma by down-regulation of thrombin generation via a novel mechanism, specifically inhibition of factor V activation.
Introduction
Protamine sulfate is a 5-kDa cationic polypeptide derived from salmon sperm that can bind negatively charged unfractionated heparin (UFH).1 Although the mechanisms of the molecular interaction between protamine and heparin are not well defined, this binding serves to neutralize the antithrombin-mediated anticoagulant properties of heparin. Moreover, the resultant protamine-heparin complex is rapidly cleared by the reticuloendothelial system.2 Consequently, for more than 30 years, protamine has been widely used to reverse the anticoagulant effects of UFH. Protamine is considered the treatment of choice for patients who develop significant bleeding complications while on UFH.3,4 Furthermore, protamine is routinely administered postoperatively to reverse the high concentrations of UFH required for patients undergoing cardiac surgery and cardiopulmonary bypass (CPB).5 As a result, estimates suggest that more than 2 million heparinized patients are managed with protamine each year.2
Clinical use of protamine is, however, associated with several important adverse side effects, including potentially life-threatening systemic arterial hypotension and pulmonary artery hypertension.1 Paradoxically, in vitro studies have also suggested that protamine may possess intrinsic anticoagulant properties.6-8 Administration of excess protamine in the neutralization of UFH has been associated with increased bleeding in clinical settings, particularly after cardiothoracic surgery.9 Due to concerns regarding the inherent anticoagulant potential of protamine, current consensus guidelines recommend that the dose of protamine is limited to 1 mg protamine per 100 IU heparin.3,4 However, pharmacokinetic studies have demonstrated that protamine is cleared rapidly from human plasma (half life 7.4 minutes), so that repeated doses may be necessary to prevent rebound heparin anticoagulant effects.10,11 Animal studies have shown that although protamine fully neutralizes the thrombin-inhibitory activity of low molecular weight heparins (LMWH), it can only partially neutralize their anti–factor Xa (FXa) activities.12,13 Therefore, the clinical efficacy of protamine for reversing LMWH-induced anticoagulation remains unclear.4
Despite the widespread use of protamine in clinical practice, the molecular mechanism(s) underlying its associated intrinsic anticoagulant effect is not clearly defined. Previous studies in which incremental concentrations of protamine (50-300 μg/mL) were added to heparinized patient samples ex vivo demonstrated that heparin anticoagulation was maximally reversed at a protamine to heparin ratio of 1.3:1.8,14 However, addition of higher protamine:heparin ratios (ie, excess free protamine) resulted in significant prolongation of the activated clotting time (ACT) through an unidentified mechanism.8 Similarly, ex vivo addition of protamine to normal pooled plasma markedly attenuated tissue factor (TF)–initiated thromboelastography.15 Protamine significantly increased clot initiation time (R time), decreased the rate of clot propagation (α angle), and diminished clot strength (maximum amplitude) in a concentration-dependent manner. Protamine has also been reported to have a weak inhibitory effect on in vitro platelet aggregation induced by adenosine 5′-diphosphate or collagen.8 In contrast, platelet factor 4, another cationic molecule that has been used therapeutically to reverse UFH anticoagulation, has no apparent endogenous anticoagulant activity in vitro.16
In this study, we sought to characterize the molecular mechanism(s) responsible for the clinically important anticoagulant activity of protamine. We demonstrate that pharmacologic doses of protamine significantly reduce thrombin generation in both murine and human plasma in a concentration-dependent manner. Moreover, although low-dose protamine (< 20 μg/mL) effectively reverses the effects of UFH, increased protamine concentration results in a progressive anticoagulant effect. We further demonstrate that this anticoagulant effect of protamine is mediated via a specific inhibition of factor V (FV) activation by either thrombin or FXa. These new insights into the mechanism of the anticoagulant side effects of protamine will advance the generation of new protamine variants with reduced associated bleeding risk.
Methods
Materials
Protamine sulfate and tinzaparin (Innohep) were obtained from Leo Pharma. Unfractionated heparin, enoxaparin (Clexane), and danaparoid (Orgaran) were from Sigma-Aldrich, Sanofi-Aventis, and Schering-Plough, respectively. BALB/c mice were purchased from Harlan. Animals were housed in a pathogen-free facility using individually ventilated and filtered cages under positive pressure. All animal experiments were performed in compliance with Irish Department of Health and Children regulations and approved by the Trinity College Dublin BioResources ethical review board. Purified human activated protein C (APC), FV, FVa, FXa, and prothrombin were purchased from Haematologic Technologies. Purified human thrombin was obtained from Enzyme Research Laboratories, and phospholipid vesicles were from Avanti Polar Lipids. Synthetic chromogenic substrates BIOPHEN CS-21(66) and BIOPHEN CS-01(38) for APC and thrombin, respectively, were sourced from HYPHEN Biomed. Thrombin generation assay reagents (platelet-poor-plasma reagent, fluorogenic substrate, thrombin calibration standard) were purchased from Thrombinoscope BV. HemosIL FV-deficient plasma was from Instrumentation Laboratory, and factor VIII (FVIII)–deficient plasma from Technoclone. The wild-type FVIII and APC-cleavage–resistant FVIII double-mutant R336Q/R562Q were gifts of Dr Philip Fay (University of Rochester School of Medicine, Rochester, NY).
Measurement of thrombin generation and tail-bleeding time in mice
BALB/c mice, aged 6 to 8 weeks, were weighed and anesthetized with midazolam and etorphine hydrochloride. Protamine sulfate was administered intravenously, followed 90 seconds later by transection of the tail tip. The tail was loosely suspended in PBS at 37°C, and time taken for complete cessation of tail bleeding was recorded. To assess the effect of protamine on in vivo thrombin generation, mice were exsanguinated at specific time points after intravenous protamine administration. Blood was collected into citrate phosphate buffer (Sigma-Aldrich), and plasma was collected by centrifugation at 1500g for 20 minutes. Thrombin generation was initiated by addition of 20 μL HemosIL activated partial thromboplastin time (APTT)–lyophilized silica reagent and 100 mM CaCl2, and was assessed using a Fluoroskan Ascent plate reader in combination with Thrombinoscope software, as described below.
APTT and PT measurement
Human plasma was prepared from a pool of normal healthy volunteers. APTT and prothrombin time (PT) were measured using the fully automated ACL TOP coagulometer (Beckman Coulter) using HemosIL APTT-lyophilized silica reagent and PT-fibrinogen HS plus reagent, respectively (Instrumentation Laboratory).
Effect of protamine on thrombin generation in normal human plasma
The anticoagulant function of protamine in normal, platelet-poor, pooled plasma was assessed using a Fluoroskan Ascent plate reader (Thermo Lab System) in combination with Thrombinoscope software (Thrombinoscope BV), as previously described.17 Briefly, 80 μL of plasma was incubated with 20 μL of platelet-poor-plasma reagent containing 5 pM TF and 4 μM phospholipids (composed of 60% phosphatidylcholine [PC], 20% phosphatidylserine [PS], and 20% phosphatidylethanolamine [PE] in the presence or absence of protamine [3-80 μg/mL; all final concentrations]). Thrombin generation was initiated by automatic dispensation of fluorogenic thrombin substrate (Z-Gly-Gly-Arg-AMC.HCl) and 100 mM CaCl2 into each well (final concentrations, Z-Gly-Gly-Arg-AMC.HCl, 0.42 mM and CaCl2, 16.67 mM). Thrombin generation was determined using a thrombin calibration standard. Measurements were taken at 20-second intervals for 60 minutes, or until thrombin generation was complete. The lag time to start of thrombin generation, peak amount of thrombin generated, time to peak thrombin (TTP), and area under the thrombin generation curve, represented by endogenous thrombin potential (ETP), were measured. Experiments were performed in triplicate, and data were reported as mean plus or minus SEM.
Characterization of APC-mediated FVa proteolysis in the presence of protamine
FVa degradation by APC was assessed, as previously described.16 A total of 8 nM APC was incubated at 37°C with phospholipid vesicles (PC:PS:PE 60%:20%:20%; Avanti Polar Lipids) and 4 nM FVa (Hematologic Technologies) in the presence and absence of protamine sulfate (3 μg/mL final concentration) in 40 mM Tris-HCl, 140 mM NaCl, 3 mM CaCl2, and 0.3% wt/vol bovine serum albumin (2 nM APC, 19 mM phospholipids, and 1 nM FVa, final concentration). Phospholipid vesicles (PC:PS:PE 60%:20%:20%) were prepared, as described previously.17 At specified time points, more than 20 minutes, 2-μL aliquots were removed and added to a prothrombinase mixture (25 μM phospholipids, 1 nM FXa, and 0.5 μM prothrombin [Hematologic Technologies], final concentrations) for 3 minutes. Each reaction was stopped using 5 μL ice-cold 0.5 M EDTA (ethylenediaminetetraacetic acid). A total of 100 μL reaction mixture was removed and incubated with 100 μl of 2 mM thrombin chromogenic substrate BIOPHEN CS-01(38) (HYPHEN Biomed) to assess thrombin generation. The rate of chromogenic substrate cleavage was measured at 405 nm using a VERSAmax microplate reader (Molecular Devices). Residual FVa activity was determined by comparison with FVa activity observed before APC incubation, and plotted values represent the mean of at least 3 individual experiments plus or minus SEM.
Characterization of APC-mediated FVIIIa proteolysis in the presence of protamine
To determine whether protamine enhancement of APC anticoagulant activity was mediated through increased rate of FVIIIa proteolysis, we used a previously characterized APC-resistant FVIII double mutant (R336Q/R562Q; APCR-FVIII).18 FVIII-deficient plasma (Technoclone) was spiked with either B-domainless wild-type FVIII (wt-FVII) or the APCR-FVIII variant (both final concentration 1.0 U/mL [300 ng/mL]). Thrombin generation was then initiated with 5 pM TF, 4 μM phospholipid vesicles (PC:PS:PE 60%:20%:20%), and CaCl2, and ETP was determined. Subsequently, the anticoagulant effect of protamine alone (3 μg/mL), APC alone (10 nM), or protamine in the presence of APC was determined for wt-FVIII and the APCR-FVIII variant, as before.
Determination of rate of FV activation in the presence of protamine
The effect of protamine on FV activation was determined using a method previously described by Safa et al.19 Briefly, purified FV (100 nM final concentration) was incubated with purified α-thrombin (1 nM final concentration) in 100 mM NaCl, 20 mM HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid; pH 7.5), 5 mM CaCl2, and 0.2 mg/mL bovine serum albumin, or with purified FXa (20 nM final concentration) and phospholipid vesicles (80 μM final concentration). At specific time intervals, aliquots were removed and diluted in 100 nM NaCl and 20 nM Tris-HCl (pH 7.5) to stop FV activation. The time course of FV activation was immediately quantified using FV-deficient plasma in a standard prothrombin-based clotting assay.
Results
Protamine prolongs in vivo bleeding time in mice and has a concentration-dependent anticoagulant effect in plasma
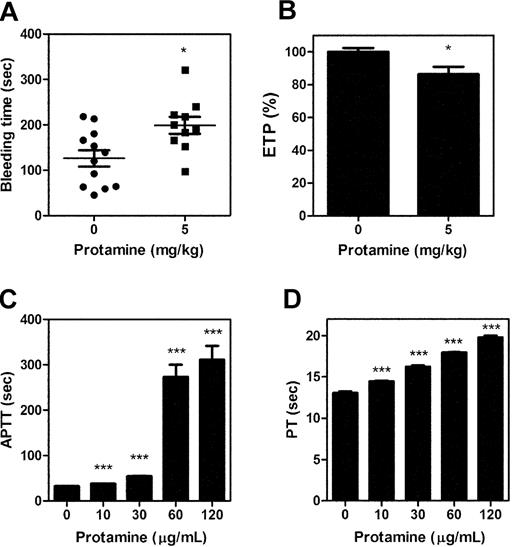
After intravenous administration of a therapeutic protamine dose (50 mg), pharmacokinetic studies have demonstrated typical plasma protamine levels of up to 50 μg/mL.11 However, in practice, doses exceeding 5 mg/kg are frequently administered.20 In BALB/c mice, we observed that parenteral protamine (5 mg/kg) administration significantly prolonged tail-bleeding time and attenuated thrombin generation (Figure 1A-B). These findings, which are in keeping with a previous report in which intravenous protamine (1.5 mg/kg) prolonged the ACT and APTT in a canine model,21 confirm that protamine has in vivo anticoagulant activity. In addition, the presence of protamine in normal pooled human plasma resulted in significant prolongations in the APTT and PT, respectively (Figure 1C-D). Furthermore, again in keeping with previous reports, protamine (5-60 μg/mL) also significantly prolonged human whole blood ACT (data not shown).8 In contrast, although previous studies demonstrated that protamine can bind fibrinogen,22 we observed no effect of protamine (final concentration 5-50 μg/mL) on thrombin-clotting time (data not shown).
Protamine prolongs in vivo bleeding time and clotting time of normal pooled plasma. BALB/c mice were injected with either phosphate-buffered saline or 5 mg/kg protamine. Tail-bleeding time (A) or, in separate mice, plasma endogenous thrombin potential (B) was measured, as described in “Methods.” In addition, the effect of protamine on clotting times of human normal pooled plasma was characterized. Increasing concentrations (10-120 μg/mL) of protamine were titrated into normal pooled plasma, and the effect on plasma APTT (C) and plasma PT (D) was determined. Results described represent the mean ± SEM (*P < .05, ***P < .001, respectively; unpaired 2-tailed t tests performed).
Protamine prolongs in vivo bleeding time and clotting time of normal pooled plasma. BALB/c mice were injected with either phosphate-buffered saline or 5 mg/kg protamine. Tail-bleeding time (A) or, in separate mice, plasma endogenous thrombin potential (B) was measured, as described in “Methods.” In addition, the effect of protamine on clotting times of human normal pooled plasma was characterized. Increasing concentrations (10-120 μg/mL) of protamine were titrated into normal pooled plasma, and the effect on plasma APTT (C) and plasma PT (D) was determined. Results described represent the mean ± SEM (*P < .05, ***P < .001, respectively; unpaired 2-tailed t tests performed).
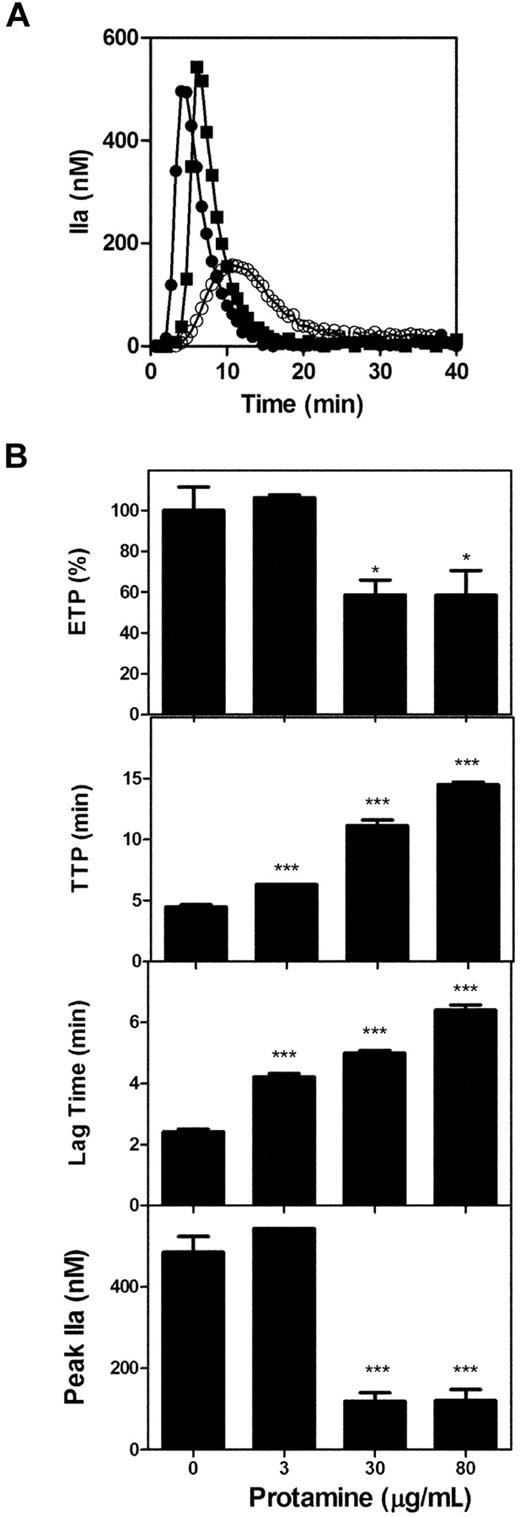
Calibrated automated thrombography was used to assess the impact of protamine on TF-initiated thrombin generation. In normal plasma, protamine significantly reduced thrombin generation (Figure 2A). Calculation of ETP demonstrated that 30 μg/mL protamine reduced thrombin generation to 59% (± 7%; P < .05) of the original ETP before protamine incubation (Figure 2B). Furthermore, at pharmacologic doses, protamine significantly influenced all of the individual parameters assessed during thrombin generation, with significant prolongation of lag time and TTP and a marked decrease in peak thrombin generation (Figure 2B), suggesting that protamine may influence the initiation and propagation phases of coagulation. This inhibition of thrombin generation was not mediated by protamine inhibition of contact activation, as corn trypsin inhibitor, which eliminates the contribution of contact pathway activation to thrombin generation in this system, had no effect on the observed reduction in thrombin generation (data not shown).
Protamine inhibits TF-initiated thrombin generation in normal plasma. Coagulation was initiated in pooled normal plasma with 5 pM TF, 4 μM phospholipid vesicles (PC:PS:PE 60%:20%:20%), and 6.67 mM CaCl2, and thrombin generation was followed using a fluorogenic substrate, as described in “Methods.” (A) Thrombin generation in the absence of protamine (●) was compared with 3 μg/mL (■) and 30 μg/mL (○) of protamine, respectively. (B) The effect of protamine (3-80 μg/mL) on individual thrombin generation curve parameters was determined. Parameters measured (top to bottom) were ETP (% of normal pooled plasma), TTP (minutes), lag time (minutes), and peak thrombin (nM). Unpaired 2-tailed t tests were performed to determine significance (***P < .0001 compared with plasma in the absence of protamine). All experiments were performed in triplicate. Results are expressed as mean ± SEM.
Protamine inhibits TF-initiated thrombin generation in normal plasma. Coagulation was initiated in pooled normal plasma with 5 pM TF, 4 μM phospholipid vesicles (PC:PS:PE 60%:20%:20%), and 6.67 mM CaCl2, and thrombin generation was followed using a fluorogenic substrate, as described in “Methods.” (A) Thrombin generation in the absence of protamine (●) was compared with 3 μg/mL (■) and 30 μg/mL (○) of protamine, respectively. (B) The effect of protamine (3-80 μg/mL) on individual thrombin generation curve parameters was determined. Parameters measured (top to bottom) were ETP (% of normal pooled plasma), TTP (minutes), lag time (minutes), and peak thrombin (nM). Unpaired 2-tailed t tests were performed to determine significance (***P < .0001 compared with plasma in the absence of protamine). All experiments were performed in triplicate. Results are expressed as mean ± SEM.
Anticoagulant effects of protamine in reversal of heparin-induced anticoagulation
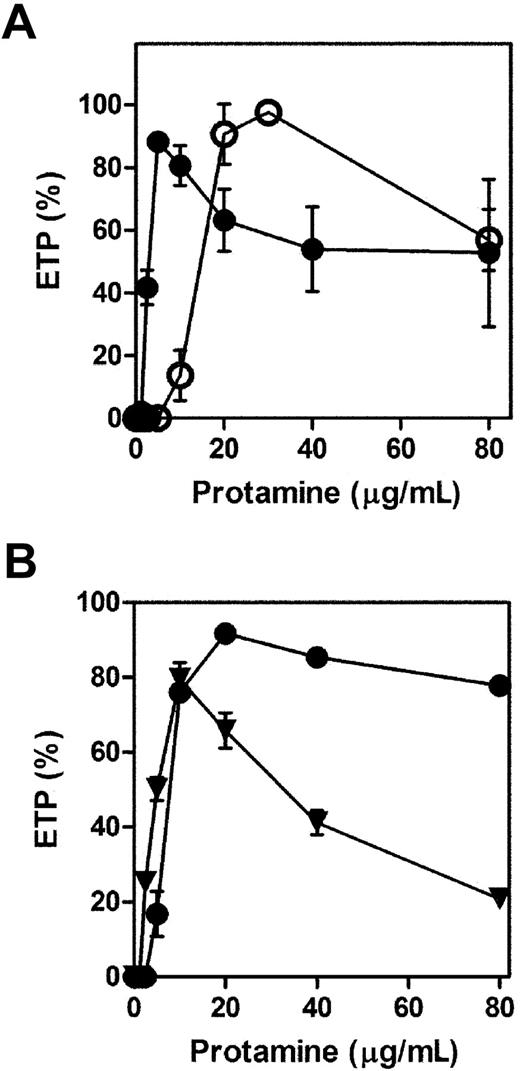
Pharmacologic dose UFH (0.3 U/mL or 1 IU/mL) reduced the ETP such that no thrombin generation was detectable (Figure 3A). Protamine initially reversed the anticoagulant effect of UFH, resulting in a progressive increase in TF-initiated thrombin generation (Figure 3A). However, addition of higher concentrations of protamine to heparinized plasma resulted in a significant progressive reduction in thrombin generation, to a minimum of 54% (± 14%) and 57% (± 10%) of normal plasma ETP for 0.3 and 1.0 IU/mL UFH, respectively (Figure 3A). Similarly, although protamine at low dose (5-20 μg/mL) completely reversed the anticoagulant effect of the LMWH tinzaparin (1.0 U/mL), higher doses of protamine (20-80 μg/mL) were again associated with a significant reduction in ETP (to 78% ± 1%). In contrast, titration of protamine into plasma containing LMWH enoxaparin (1.0 U/mL) failed to fully correct TF-initiated thrombin generation (maximum 80% ± 4%). Moreover, in plasma containing enoxaparin, higher doses of protamine resulted in a more marked anticoagulant effect than that observed with either UFH or tinzaparin, respectively, to 21% (± 2% of normal ETP (Figure 3B).
Anticoagulant activity of excess protamine administration during reversal of heparin-induced anticoagulation. (A) Protamine (10-80 μg/mL) was titrated into normal pooled plasma containing 0.3 U/mL (●) or 1.0 U/mL (○) UFH, and TF-initiated thrombin generation was determined as before. (B) The ability of protamine (10-80 μg/mL) to reverse different LMWH preparations of 1.0 U/mL tinzaparin (●) or 1.0 U/mL enoxaparin (▼) was also characterized.
Anticoagulant activity of excess protamine administration during reversal of heparin-induced anticoagulation. (A) Protamine (10-80 μg/mL) was titrated into normal pooled plasma containing 0.3 U/mL (●) or 1.0 U/mL (○) UFH, and TF-initiated thrombin generation was determined as before. (B) The ability of protamine (10-80 μg/mL) to reverse different LMWH preparations of 1.0 U/mL tinzaparin (●) or 1.0 U/mL enoxaparin (▼) was also characterized.
Anticoagulant effects of APC in plasma are enhanced by protamine
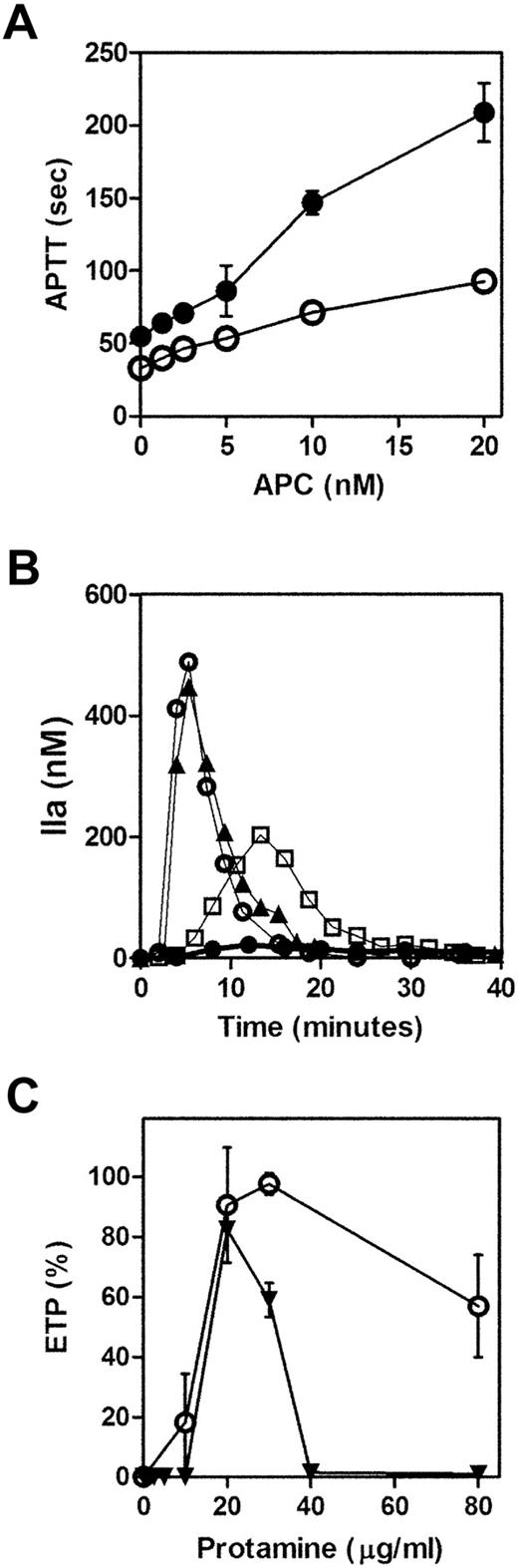
APC down-regulates thrombin generation by inactivation of procoagulant cofactors FVa and FVIIIa. Moreover, we have recently demonstrated that FVa proteolysis by APC can be specifically modulated by another cationic polypeptide, platelet factor 4.16 Consequently, we hypothesized that the anticoagulant effects of cationic protamine might be mediated through a similar mechanism. As expected, APC (1.25-20 nM) alone caused a concentration-dependent prolongation in APTT (maximum 2.8 ± 0.1-fold prolongation) in normal plasma (Figure 4A). However, the anticoagulant activity of APC on the APTT was markedly enhanced at all concentrations in the presence of protamine (30 μg/mL; Figure 4A). Furthermore, in keeping with the observed APTT findings, pharmacologic doses of protamine also significantly enhanced APC attenuation of TF-initiated thrombin generation. For example, although 1 nM APC alone had minimal effect on thrombin generation, coincubation of the same APC concentration with protamine (30 μg/mL) entirely ablated thrombin generation in normal plasma (Figure 4B). A synergistic anticoagulant interaction between APC and protamine was also observed in heparinized plasma. In the presence of 1 nM APC, the ability of high protamine concentrations to inhibit thrombin generation was markedly enhanced, such that thrombin generation was entirely ablated at 40 μg/mL protamine (Figure 4C).
Anticoagulant effects of APC in normal plasma are enhanced by protamine. (A) Increasing concentrations of APC (1.25-20 nM) were added to normal pooled plasma in the presence (●) and absence (○) of 30 μg/mL protamine, and plasma APTT was measured. (B) Thrombin generation in normal pooled plasma (○) was compared with plasma spiked with 1 nM APC (▲) alone, 30 μg/mL protamine (□) alone, or 1 nM APC plus 30 μg/mL protamine (●) in combination. (C) ETP (% of normal pooled plasma) was calculated after titration of protamine (0.2-80 μg/mL) into normal plasma containing 1.0 U/mL UFH and either in the absence (○) or presence (▼) of 1 nM APC.
Anticoagulant effects of APC in normal plasma are enhanced by protamine. (A) Increasing concentrations of APC (1.25-20 nM) were added to normal pooled plasma in the presence (●) and absence (○) of 30 μg/mL protamine, and plasma APTT was measured. (B) Thrombin generation in normal pooled plasma (○) was compared with plasma spiked with 1 nM APC (▲) alone, 30 μg/mL protamine (□) alone, or 1 nM APC plus 30 μg/mL protamine (●) in combination. (C) ETP (% of normal pooled plasma) was calculated after titration of protamine (0.2-80 μg/mL) into normal plasma containing 1.0 U/mL UFH and either in the absence (○) or presence (▼) of 1 nM APC.
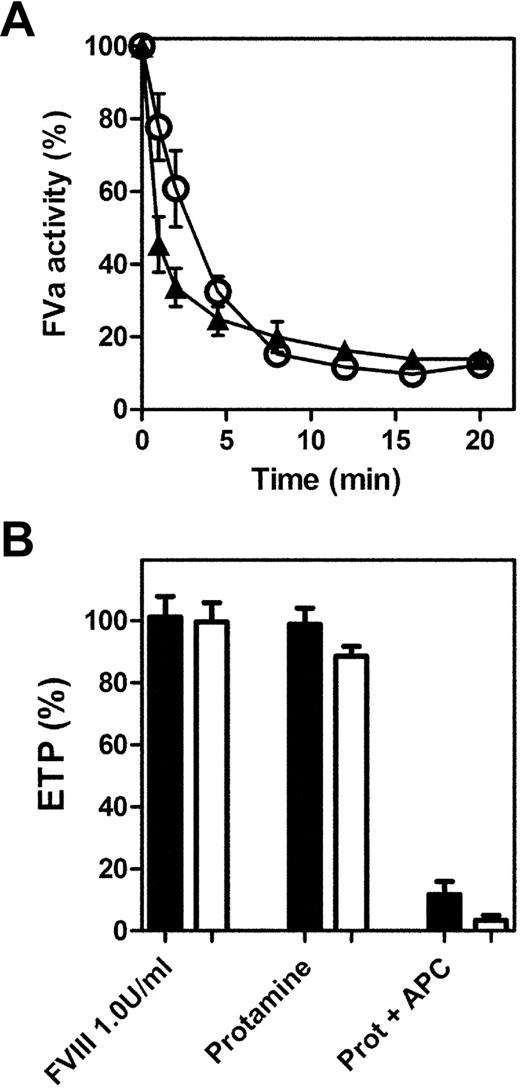
Protamine does not enhance FVa or FVIIIa proteolysis by APC
To further elucidate the mechanism(s) through which protamine enhances APC anticoagulant activity, the rate of FVa proteolysis in the presence or absence of protamine was determined using a phospholipid-dependent FVa proteolysis time course assay (Figure 5A). In this purified system, the ability of APC to cleave and inactivate procoagulant FVa was not significantly enhanced in the presence of pharmacologic concentrations of protamine. Therefore, to determine whether the anticoagulant activity of protamine was due to enhanced FVIIIa proteolysis by APC, we assessed thrombin generation in FVIII-deficient plasma in the presence of an APC-resistant FVIII variant (R336Q/R562Q).18 Wild-type or variant FVIII in FVIII-deficient plasma entirely restored ETP to normal plasma levels (Figure 5B). Although low-dose protamine (3 μg/mL) did not significantly reduce ETP, a marked anticoagulant interaction was again observed when protamine was combined with APC (10 nM). Moreover, the synergistic anticoagulant effects of APC in combination with protamine were comparable for wild-type FVIII and for APC-resistant FVIII, suggesting that accelerated FVIIIa proteolysis is not responsible for the enhanced anticoagulant effects of APC in the presence of protamine.
APC-protamine anticoagulant synergy is not mediated by enhanced substrate proteolysis. (A) FVa proteolysis by APC was assessed in both the absence (▲) and presence (○) of 3 μg/mL protamine. Purified FVa (1 nM final concentration) was incubated with phospholipid vesicles (PC:PS:PE, 60%:20%:20%, 20 μM final concentration) in a buffer containing 175 mM NaCl, 3 mM CaCl2, and 25 mM HEPES (pH 7.4) at 37°C. APC (2 nM final concentration) was added to initiate FVa inactivation. At specific time points, aliquots of the reaction mix were added to a separate prothrombinase mixture and thrombin generated was measured, as described in “Methods.” (B) To assess FVIIIa proteolysis by APC, thrombin generation was initiated with TF, phospholipid vesicles, and CaCl2 in FVIII-deficient plasma to which 1.0 U/mL wild-type (□) or APC-resistant FVIII R336Q/R562Q (■), respectively, had been added. ETP was determined for each FVIII variant in the presence and absence of protamine (3 μg/mL) and also in the presence of APC (10 nM).
APC-protamine anticoagulant synergy is not mediated by enhanced substrate proteolysis. (A) FVa proteolysis by APC was assessed in both the absence (▲) and presence (○) of 3 μg/mL protamine. Purified FVa (1 nM final concentration) was incubated with phospholipid vesicles (PC:PS:PE, 60%:20%:20%, 20 μM final concentration) in a buffer containing 175 mM NaCl, 3 mM CaCl2, and 25 mM HEPES (pH 7.4) at 37°C. APC (2 nM final concentration) was added to initiate FVa inactivation. At specific time points, aliquots of the reaction mix were added to a separate prothrombinase mixture and thrombin generated was measured, as described in “Methods.” (B) To assess FVIIIa proteolysis by APC, thrombin generation was initiated with TF, phospholipid vesicles, and CaCl2 in FVIII-deficient plasma to which 1.0 U/mL wild-type (□) or APC-resistant FVIII R336Q/R562Q (■), respectively, had been added. ETP was determined for each FVIII variant in the presence and absence of protamine (3 μg/mL) and also in the presence of APC (10 nM).
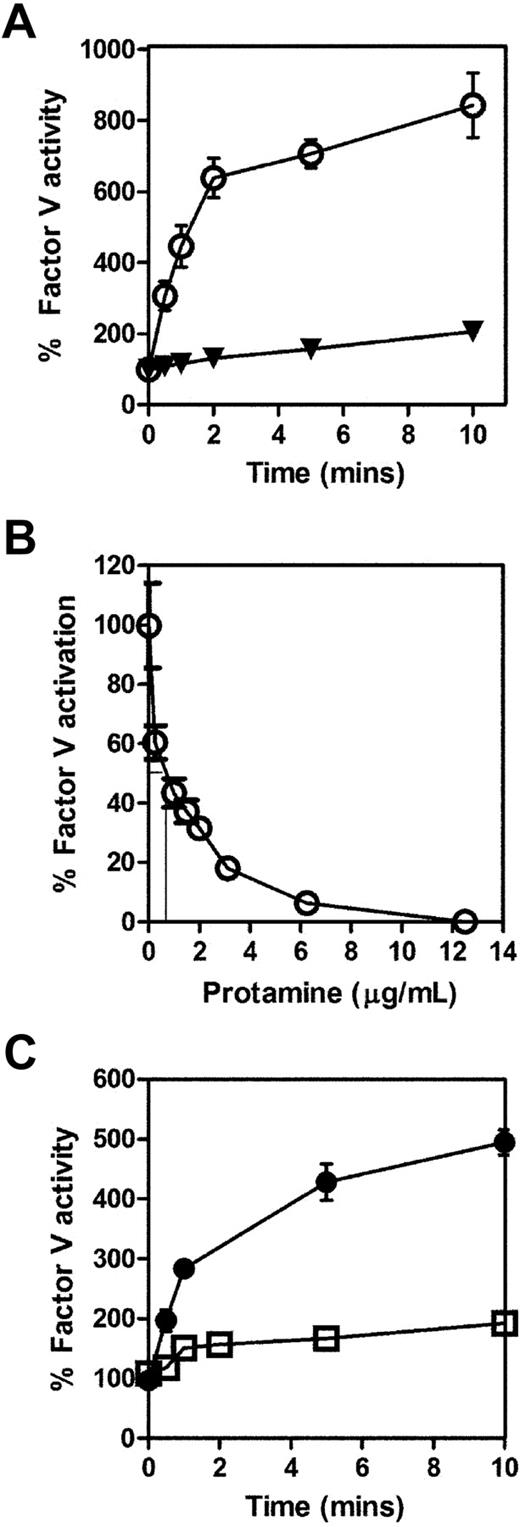
Protamine inhibits activation of FV by α-thrombin and FXa
We further investigated whether protamine enhancement of APC in plasma was due to inhibition of FVa generation. In the presence of pharmacologic concentrations of protamine (50 μg/mL), activation of FV by thrombin (1 nM) was entirely ablated (Figure 6A). Moreover, low concentrations of protamine (0.25-12.5 μg/mL) significantly attenuated FV activation in a dose-dependent manner (Figure 6B). The 50% inhibitory concentration for protamine inhibition of FV activation by thrombin was only 0.8 μg/mL. Consequently, this effect is of clear clinical importance, given that peak protamine plasma concentrations can potentially reach 50 μg/mL after a single 50-mg bolus administration.11 Although physiologic activation of FV is predominantly mediated by thrombin, FXa can also activate FV.23 Interestingly, however, in the presence of protamine (50 μg/mL), FV activation by FXa (20 nM) was also significantly reduced (Figure 6C).
Protamine inhibits activation of intact FV by thrombin and by FXa. (A) The rate of activation of 100 nM purified FV by 1 nM thrombin was measured in a PT-based clotting assay using FV-deficient plasma (as described in “Methods”) in the absence (○) and presence (▼) of 50 μg/mL protamine. (B) To determine the 50% inhibitory concentration for the observed effect, the activity of FV was measured after incubation with thrombin and increasing (0.25-12.5 μg/mL) concentrations of protamine for 60 seconds. Activity was expressed as a percentage of activity in the absence of protamine. (C) To assess whether FXa-mediated FV activation was affected by protamine, the rate of activation of 100 nM purified FV by 20 nM FXa in the presence of phospholipid vesicles (PC:PS:PE 60%:20%:20%, 80 μM final concentration) was assessed in the absence (●) and presence (□) of 50 μg/mL protamine in a PT-based clotting assay.
Protamine inhibits activation of intact FV by thrombin and by FXa. (A) The rate of activation of 100 nM purified FV by 1 nM thrombin was measured in a PT-based clotting assay using FV-deficient plasma (as described in “Methods”) in the absence (○) and presence (▼) of 50 μg/mL protamine. (B) To determine the 50% inhibitory concentration for the observed effect, the activity of FV was measured after incubation with thrombin and increasing (0.25-12.5 μg/mL) concentrations of protamine for 60 seconds. Activity was expressed as a percentage of activity in the absence of protamine. (C) To assess whether FXa-mediated FV activation was affected by protamine, the rate of activation of 100 nM purified FV by 20 nM FXa in the presence of phospholipid vesicles (PC:PS:PE 60%:20%:20%, 80 μM final concentration) was assessed in the absence (●) and presence (□) of 50 μg/mL protamine in a PT-based clotting assay.
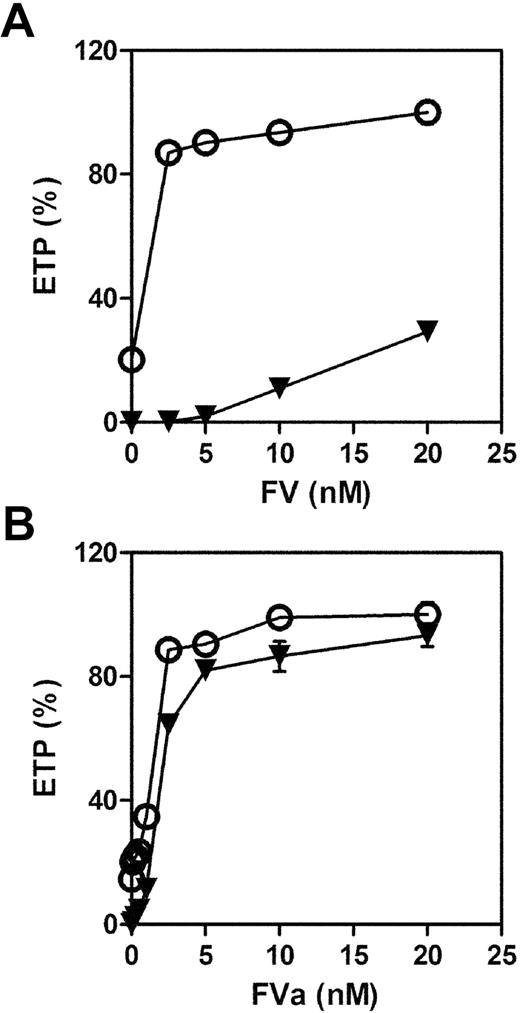
Preactivation of FV eliminates protamine anticoagulant effect in plasma
Previous studies have suggested that protamine may influence several different procoagulant and anticoagulant reactions in plasma.6,7,24,25 To determine the relative importance of protamine inhibition of FV activation in mediating the anticoagulant effect of protamine in plasma, increasing concentrations of either FV or FVa (0-20 nM) were titrated into FV-deficient plasma in the presence or absence of protamine (30 μg/mL; Figure 7). In a TF-initiated thrombin generation assay, addition of FV or FVa resulted in a significant increase in thrombin generation (Figure 7A-B). In keeping with our previous findings, protamine (30 μg/mL) significantly inhibited thrombin generation at all concentrations of FV (Figure 7A). However, in the presence of preactivated FVa, the ability of protamine to significantly inhibit thrombin generation was no longer evident (Figure 7B). Cumulatively, these data support the hypothesis that protamine-mediated inhibition of FV activation plays a critical role in mediating its anticoagulant activity in human plasma.
The anticoagulant effect of protamine is greatly reduced by preactivation of FV to FVa. (A) FV (2.5-20 nM) or (B) FVa (1-20 nM) was titrated into FV-deficient plasma in the absence (○) and presence (▼) of protamine (30 μg/mL). Thrombin generation was initiated with TF, phospholipid vesicles, and CaCl2 (see “Methods”), and ETP was calculated as before.
The anticoagulant effect of protamine is greatly reduced by preactivation of FV to FVa. (A) FV (2.5-20 nM) or (B) FVa (1-20 nM) was titrated into FV-deficient plasma in the absence (○) and presence (▼) of protamine (30 μg/mL). Thrombin generation was initiated with TF, phospholipid vesicles, and CaCl2 (see “Methods”), and ETP was calculated as before.
Discussion
Protamine sulfate is widely regarded as the treatment of choice for reversing UFH-induced anticoagulation. However, excessive protamine administration has been associated with anticoagulant activity, and has been implicated in the etiology of perioperative bleeding for many years.6-8,26 In particular, previous trials have demonstrated that the use of lower doses of protamine for heparin neutralization in patients after CPB resulted in reduced postoperative blood loss.26-30 In a prospective study, Despotis et al randomized 254 patients requiring CPB to heparin neutralization with either a fixed dose of protamine (0.8 mg of protamine per mg total UFH), or a titrated protamine dosing based upon residual plasma heparin concentration.28 Although patients in the titrated protamine dosing arm of the study received lower doses of protamine, they developed fewer bleeding complications and required significantly less hemostatic support (platelets, fresh frozen plasma, and cryoprecipitate transfusions) during the perioperative period. Similarly, another prospective randomized trial of adult patients undergoing CPB also demonstrated that reduction in protamine dose was associated with significantly decreased mediastinal blood loss (∼ 50%).29
In this study, we investigated the molecular mechanisms responsible for these clinically important protamine-mediated anticoagulant effects. We demonstrate that in vivo administration of protamine significantly reduces thrombin generation in murine plasma, and significantly prolongs tail-bleeding time. Moreover, protamine also has anticoagulant activity in normal human plasma. At pharmacologic doses (> 10 μg/mL), protamine prolonged both the PT and APTT, suggesting an effect on the common pathway. Furthermore, protamine also significantly attenuated TF-initiated thrombin generation in human plasma.
Conversion of pro-cofactor FV to active FVa occurs early in the process of TF-initiated coagulation.31 Initial activation of FV by thrombin involves limited proteolytic cleavage of peptide bonds at Arg709, Arg1018, and Arg1545. FVa then associates with FXa on negatively charged phospholipid membrane surfaces to form the prothrombinase complex. In this complex, FVa acts as a critical cofactor, enhancing the ability of FXa to convert prothrombin to thrombin by 300 000-fold.32 In addition, FVa binding also makes FXa refractory to inhibition by anticoagulant tissue factor pathway inhibitor.33 Using purified protein assays to study the anticoagulant activity of protamine, we demonstrate that FV activation by α-thrombin is reduced in a dose-dependent manner by protamine. Moreover, this novel specific inhibitory effect upon FV activation is responsible for the bulk of the anticoagulant effect of protamine on TF-initiated thrombin generation in human plasma. Indeed, protamine had only a minor inhibitory effect on thrombin generation in plasma containing preformed FVa rather than pro-cofactor FV. Further studies will be required to unravel the precise mechanism(s) through which protamine attenuates activation of FV. Nevertheless, the observation that FV activation by both thrombin and FXa is inhibited indicates protamine may form an inhibitory complex with FV.
Because arginine residues account for approximately 60% of its primary amino acid sequence, protamine is highly cationic. Interestingly, several recent studies have shown that specific anionic molecules have the opposite effect to protamine on FV activation.34-36 In particular, polyphosphate, a linear polymer of inorganic phosphate present in the dense granules of human platelets, significantly enhanced the rate of FV activation by both thrombin and FXa.34,37 Similarly, AV513, a sulfated proteoglycan of plant origin, has been shown to accelerate thrombin generation by significantly enhancing FV activation.36 Finally, in antithrombin-deficient plasma, negatively charged UFH also had significant procoagulant activity due to increased FV activation.35 The molecular interactions through which these different anionic polymers function to enhance FV activation have not been defined. Nevertheless, these reports combined with our novel findings cumulatively support the hypothesis that charge-mediated interactions may be critical in regulating FV activation.
Previous studies have reported that protamine can also down-regulate coagulation by directly inhibiting thrombin activity.24 However, high protamine concentrations (> 100 μg/mL) were only associated with relatively minor reductions in thrombin function.24 Moreover, at pharmacologic concentrations (≤ 50 μg/mL), we observed no significant protamine effect on thrombin-clotting time, or thrombin amidolytic activity (data not shown). In contrast, the presence of 10 μg/mL protamine in pooled normal plasma was sufficient to prolong both the PT and APTT. In addition, the lag time and TTP of TF-initiated thrombin generation were significantly prolonged by 3 μg/mL protamine. Consequently, our findings clearly indicate that direct thrombin inhibition plays a relatively minor role in mediating the anticoagulant function of protamine. More recently, Nielsen demonstrated that clinically encountered protamine concentrations also resulted in enhanced fibrinolysis.15 Although the mechanism(s) responsible for this effect was not defined, these data would be consistent with a down-regulation in thrombin generation, and consequent reduction in thrombin-activatable fibrinolysis inhibitor activation.
The ability of pharmacologic doses of protamine to markedly inhibit FV activation has several direct important translational implications. First, the ACT assay is routinely used to monitor UFH-induced anticoagulation during cardicac surgery, and to evaluate the efficacy of protamine reversal during the immediate postoperative period.5,9 In other patients, including those presenting with life-threatening bleeding complications, heparin reversal after protamine administration is typically assessed using an APTT assay.4 However, as we have shown, administration of excess protamine significantly inhibits FV activation, thereby prolonging both the ACT and APTT, respectively. Consequently, an increased ACT or APTT after protamine administration cannot be regarded as pathognomonic of inadequate heparin reversal, but rather may reflect excess free protamine. Interestingly, we observed that TF-initiated thrombin generation curves could rapidly and reliably differentiate between residual heparin and excess protamine, suggesting a potential new diagnostic application for calibrated automated thrombography in this setting.
Second, our findings have important clinical implications in relation to the use of protamine for reversing LMWH-induced anticoagulation. Although protamine reverses the antithrombin activity of LMWH, it only partially neutralizes FXa inhibition. Consequently, as we demonstrate in this study, protamine is more effective in reversing the anticoagulant activity of LMWH with lower anti-FXa:antithrombin ratios (eg, tinzaparin 2:1 compared with enoxaparin 3:1). However, we further demonstrate that rather than reversing LMWH-induced anticoagulant properties, administration of high protamine concentrations actually serves to further enhance the anticoagulant status. Furthermore, this phenomenon is more apparent in the presence of enoxaparin rather than tinzaparin, and presumably reflects residual LMWH anti-FXa activity, coupled with the inhibitory activity of excess free protamine on FV activation. Interestingly, an even more marked combined anticoagulant response was observed when protamine was titrated into plasma containing the low molecular weight heparinoid danaparoid (anti-FXa:antithrombin ratio 28:1; data not shown). Further adequately powered clinical studies will be required to define the clinical utility of protamine in reversing the anticoagulant effects of LMWH. Finally, although protamine does not directly enhance the proteolytic activity of APC, nevertheless, the combination of protamine and APC does result in a potent synergistic anticoagulant effect. Consequently, our data suggest that protamine administration should be used with caution in patients with severe sepsis receiving recombinant APC by continuous infusion.
Presented in abstract form as an oral presentation at the 50th annual meeting of the American Society of Hematology, San Francisco, CA, December 7, 2009.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by Molecular Medicine Ireland Clinician Scientist Award G04005 (to F.N.A.); Health Research Board Ireland Project Grant Award RP/2006/44 (to J.S.O.); Health Research Board Ireland Postdoctoral Fellowship PD/2006/24 (to R.J.S.P.); an Irish Heart Foundation grant (to J.S.O.); and Science Foundation Ireland President of Ireland Young Researcher Award 06/Y12/0925 (to J.S.O.).
Authorship
Contribution: F.N.A. designed the research, performed experiments, analyzed results, made the figures, and wrote the paper; R.J.S.P. designed and supervised the research, analyzed results, and wrote the paper; P.V.J. and H.J.N. performed experiments and analyzed results; J.A.J. performed experiments; O.P.S. and B.W., supervised the research; P.G.F. designed and supervised the research; and J.S.O. designed and supervised the research and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: James S. O'Donnell, Hemostasis Research Group, Trinity Health Center, St James's Hospital, James's St, Trinity College, Dublin, Ireland; e-mail: jodonne@tcd.ie.