Abstract
Characterization of lymphocytes including B cells during early versus chronic HIV infection is important for understanding the impact of chronic viremia on immune cell function. In this setting, we investigated B cells before and after reduction of HIV plasma viremia by antiretroviral therapy (ART). At baseline, peripheral blood B-cell counts were significantly lower in both early and chronic HIV-infected individuals compared with uninfected controls. Similar to CD4+ but not CD8+ T cells, B-cell numbers in both groups increased significantly after ART. At baseline, B cells of early HIV-infected individuals were composed of a higher percentage of plasmablasts and resting memory B cells compared with chronic HIV-infected individuals whose B cells were composed of a higher percentage of immature/transitional and exhausted B cells compared with their early infection counterparts. At 1 year after ART, the percentage of resting memory B cells remained higher in early compared with chronic HIV-infected individuals. This difference translated into a better functional profile in that memory B-cell responses to HIV and non-HIV antigens were superior in early- compared with chronic-treated HIV infected individuals. These findings provide new insights on B cells in HIV infection and how early initiation of ART may prevent irreversible immune system damage.
Introduction
Numerous perturbations of B-cell phenotype and function have been described in HIV-infected individuals (reviewed in Cagigi et al1 and Moir and Fauci2 ). Phenotypic perturbations of B cells circulating in the peripheral blood include over-representation of activated, exhausted, and terminally differentiated B cells associated with HIV viremia3-5 ; over-representation of immature/transitional B cells associated with HIV-induced CD4+ T-cell lymphopenia6,7 ; and reduced representation of CD27+ memory B cells associated with most stages of HIV infection.8-13 Most of these studies, whether longitudinal or cross-sectional, have been conducted on chronically HIV-infected individuals, whereas only a few studies, generally with small sample sizes, have addressed the effect of duration of infection and initiation of antiretroviral therapy (ART) on perturbations of B-cell subpopulations in HIV-infected individuals.9,14,15
Functional perturbations of B cells in HIV-infected individuals include hypergammaglobulinemia associated with polyclonal and HIV-specific activation of B cells induced by ongoing HIV replication,15,16 as well as decreased B-cell responses to specific immunogens and non-HIV pathogens.11,17,18 The latter is likely a reflection of both CD4+ T-cell dependent and independent defects in B cells that arise in HIV-infected individuals, and especially in individuals with ongoing viral replication. Many of the functional B-cell defects described in HIV-viremic individuals can be improved with ART, although there is 1 important exception that has received relatively little attention. While B-cell responses against non-HIV antigens are either stabilized or increased after initiation of ART,19-22 the reverse is often observed for B-cell responses against HIV antigens,15,23,24 suggesting that the humoral response against HIV is dependent on continuous HIV replication. In the most comprehensive study on B-cell responses after ART, Morris and colleagues described a rapid loss of HIV-specific B cells (actively secreting plasmablasts) during therapy, followed by a more gradual decrease in antibody titers against HIV in chronically infected individuals; the loss was even more rapid in early-treated individuals.15
In a previous study of chronically HIV-infected individuals, we reported a reduction in B-cell numbers and the presence of perturbed B-cell subpopulations before initiation of ART followed by partial normalization 1 year after successful reduction in viremia by ART.25 In a more recent study,5 we identified a subpopulation of CD27− tissue-like memory B cells within an abnormal CD21lo B-cell compartment of the peripheral blood of chronically HIV-viremic individuals; this subpopulation had been included within the activated B-cell compartment that we had previously described.25 These CD27− tissue-like memory B cells bore many features of exhausted cells, arising in the context of chronic immune activation, and with features that include expression of multiple inhibitory receptors, a stunted replication history and immunoglobulin diversification, as well as a reduced capacity to proliferate.25 In addition, there was an enrichment of the HIV-specific response within this compartment of tissue-like memory B cells whereas B-cell responses to the recall antigen influenza were enriched within the classic CD27+ memory B-cell compartment. Similar features have been described for both B cells and T cells in the context of persisting pathogens, including HIV, lymphocytic choriomeningtitis virus, and malaria.26-28
In the present study, we have extended both our previous studies to investigate the phenotypic profile of B cells as well as B-cell function in early and chronic HIV infected individuals and to evaluate the longitudinal effects of ART in such individuals. We identified clear differences in these parameters between individuals during early versus chronic HIV infection, and both before and 1 year after initiation of ART. These findings provide new insight into the pathogenesis of B cell abnormalities in HIV infection and provide further evidence that early initiation of ART may help preserve immune capacity.
Methods
Study participants
Leukapheresis and blood draw products were obtained from HIV-infected and HIV-uninfected individuals after informed consent approved by the Institutional Review Board of the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH) in accordance with the Declaration of Helsinki. Three groups of individuals were recruited as detailed in Table 1. Early HIV-infected individuals were defined as having been infected with HIV within 6 months of donating baseline samples. Chronically HIV-infected individuals were defined as having been infected for at least 6 months and usually for several years. HIV plasma viremia was measured by branched DNA assay (Bayer Diagnostics), with a lower limit of detection of 50 copies per mL. Functional B cell assays were performed on a subset of individuals who received seasonal influenza vaccination on a regular annual basis.
Phenotypic analyses
Multicolor flow cytometry analyses were performed on whole blood to determine lymphocyte counts and the frequency of each B-cell subpopulation. Lymphocyte counts were performed by a core NIAID facility following standard procedures. The following fluorochrome-conjugated monoclonal antibodies were used to stain B cells: allophycocyanin (APC) anti-CD10, APC-H7 anti-CD20, fluorescein isothiocyanate (FITC) anti-IgM, and phycoerythrin (PE) anti-IgG (BD Biosciences); PerCP-Cy5.5 anti-CD19 and PE-Cy7 anti-CD27 (eBioscience); FITC anti-CD21 (Beckman Coulter); and FITC anti-IgA (Dako). Analyses were performed on a Canto flow cytometer (BD Biosciences) with FlowJo Version 8.6 software (TreeStar).
Functional analyses
Peripheral blood mononuclear cells (PBMCs) were obtained by density-gradient centrifugation. Mature (CD10−) B cells were isolated from PBMCs by negative selection using a B-cell enrichment custom cocktail containing an anti-CD10 monoclonal antibody and magnetic bead-based robotic separation (StemCell Technologies). The purity of B cells was typically greater than 95%. Enrichment for CD27+ B cells was performed as previously described,5 with biotinylated anti-CD27 (eBioscience) and anti-biotin Microbeads (Miltenyi Biotec). The CD27+ B cells were placed in culture for 4 days and then used to perform memory B-cell Elispot assays, as previously described,5 with the following modifications. The Elispot assays for influenza were performed as described,29 with the modification that IgA, IgG, and IgM isotypes were measured separately as previously described.5 The source of seasonal influenza vaccine preparation used for coating was matched with the most recent vaccine received by each participant. The ancestral HIV-1 gp120 preparation used for direct coating (immobilized format previously described5 ) was also the same source that was biotinylated for the soluble approach. In this case, wells were coated with 5 μg/mL each of anti–human lambda and kappa antibodies (Rockland Immunochemicals) and detection was made with the biotinylated HIV-1 gp120, followed by standard detection, as previously described.5
Statistical analyses
Three-group comparisons were performed using the Kruskall-Wallis test followed by pair wise comparisons with the Wilcoxon rank sum test, as previously described.5 2-group comparisons were performed using the Wilcoxon rank sum test, and the Wilcoxon signed rank test was used for comparisons within a group. Changes in lymphocyte counts after initiation of ART were analyzed as previously described using mixed models.25 Changes in B-cell subpopulations between baseline and 12 months of ART were analyzed as previously described.25 Briefly, percent differences before and after ART were calculated as a sum distance and a permutation test was used to evaluate whether this sum distance was significant.
Results
Lymphocyte counts before and after ART
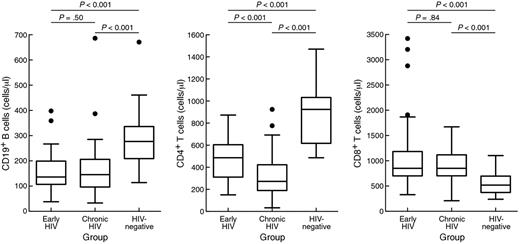
We first measured the absolute number of CD19+ B cells, as well as CD4+ and CD8+ T cells in the peripheral blood of 3 groups of individuals, namely ART-untreated individuals in early and chronic HIV infection, as well as HIV-uninfected control individuals (Table 1). These analyses were restricted to men given the paucity of early HIV-infected women recruited in most North American cohorts, including ours, and strong evidence for sex-related immunologic and virologic differences in HIV infection.30,31 B-cell and CD4+ T-cell counts were significantly higher in HIV-negative individuals compared with both early and chronically HIV-infected individuals whereas CD8+ T-cell counts were lower in HIV-uninfected compared with both HIV-infected groups (Figure 1). There was no significant difference in B-cell and CD8+ T-cell counts between the 2 HIV-infected groups whereas CD4+ T-cell counts were significantly higher in early compared with chronically HIV-infected individuals (P < .001). There was no significant difference in HIV plasma viremia between the 2 HIV-infected groups and no significant difference in age between the 3 groups (Table 1), and differences in Figure 1 remained significant after adjusting for these 2 variables. In the group of early HIV-infected individuals, 23 elected to begin ART shortly after diagnosis and agreed to return for follow-up visits over a period of 78 to 407 days (median 358 days). All early ART-treated individuals achieved undetectable levels of HIV viremia within this period, with 15 of the 23 individuals achieving undetectable viremia within 15 weeks. Similarly, in the group of chronically HIV-infected individuals, 37 elected to begin ART and were monitored for a period of 177 to 409 days (median 353 days). All ART-treated chronically HIV-infected individuals achieved undetectable levels of HIV viremia within this period, with 17 of the 37 individuals achieving undetectable viremia within 15 weeks.
Lymphocyte counts in healthy individuals and early and chronically HIV-infected individuals before ART. Box plots of absolute lymphocyte numbers in the peripheral blood are shown for 3 groups of individuals: early and chronic HIV-infected individuals before initiation of therapy as well as HIV-uninfected individuals. Box plots include median with 25th and 75th percentile boarders and error bars represent 10th and 90th percentiles.
Lymphocyte counts in healthy individuals and early and chronically HIV-infected individuals before ART. Box plots of absolute lymphocyte numbers in the peripheral blood are shown for 3 groups of individuals: early and chronic HIV-infected individuals before initiation of therapy as well as HIV-uninfected individuals. Box plots include median with 25th and 75th percentile boarders and error bars represent 10th and 90th percentiles.
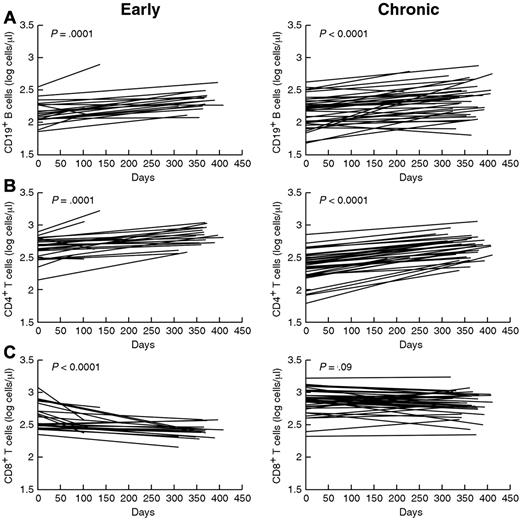
When changes in lymphocyte counts were plotted over time for each HIV-infected group after initiation of ART, there was a significant increase in both CD4+ T cells and B cells whereas the decrease in CD8+ T cells was only significant for early-treated individuals (Figure 2). When changes in lymphocyte counts were compared over time between the 2 groups of HIV-infected individuals using a mixed model analysis, there were no significant differences in slopes associated with treatment between early and chronically HIV-infected individuals for B cells (Figure 2A) and CD4+ T cells (Figure 2B), whereas the slope for CD8+ T cells declined with treatment more sharply for early compared with chronically HIV-infected individuals (Figure 2C, P < .001). Thus, in contrast to previous findings showing a slow normalization of CD8+ T cells after ART in chronically HIV-infected individuals,25 the findings here and elsewhere show a more rapid normalization of CD8+ T cells in early-treated individuals.32,33 These data also confirm the observation made in our previous study, namely that B cells are more similar to CD4+ than to CD8+ T cells with regard to changes after initiation of ART,25 and that B-cell and CD4+ T-cell numbers increase significantly in both early and chronically HIV-infected individuals after ART.
Changes in lymphocyte counts over time after initiation of ART. Absolute numbers of CD19+ B cells (A), CD4+ (B), and CD8+ (C) T cells in the peripheral blood were measured over time after initiation of ART at day 0. Each line represents the trajectory for 1 individual and was generated using regression from a minimum of 3 time points after initiation of ART. Left panels represent individuals treated early after infection and right panels represent individuals treated during the chronic stage of infection.
Changes in lymphocyte counts over time after initiation of ART. Absolute numbers of CD19+ B cells (A), CD4+ (B), and CD8+ (C) T cells in the peripheral blood were measured over time after initiation of ART at day 0. Each line represents the trajectory for 1 individual and was generated using regression from a minimum of 3 time points after initiation of ART. Left panels represent individuals treated early after infection and right panels represent individuals treated during the chronic stage of infection.
B-cell subpopulations before and after initiation of ART
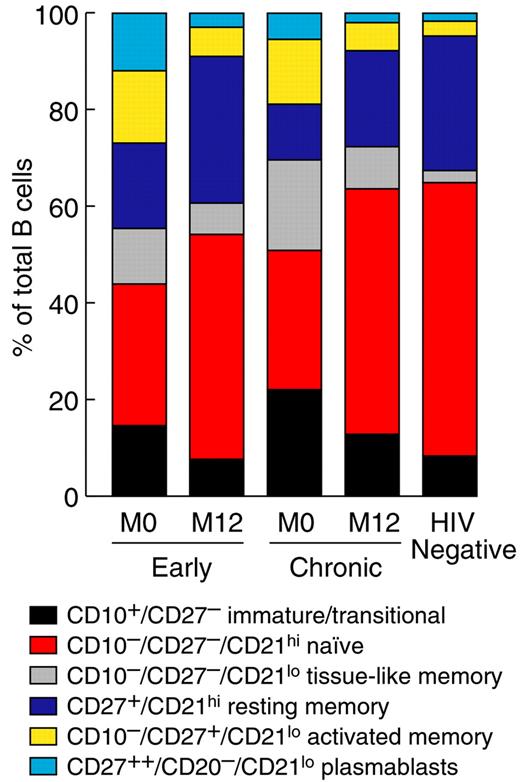
To evaluate the effect of ART on the phenotypic profile in B cells, we evaluated frequencies of various B-cell subpopulations in early and chronically HIV-infected individuals before and 1 year after initiation of ART, and in 20 HIV-negative individuals. Based on previous studies (reviewed in Moir and Fauci2 ), CD19+ B cells in the peripheral blood of HIV-viremic individuals can be divided into the following 6 subpopulations listed in order of increasing level of differentiation: immature/transitional (CD10+/CD27−), naive (CD27−/CD21hi), tissue-like memory (CD27−/CD21lo), resting/memory (CD27+/CD21hi), and activated/memory (CD27+/CD21lo) B cells as well as plasmablasts (CD27++/CD20−/CD21lo). Of note, the resting/memory B-cell compartment also includes germinal-founder B cells (CD10+/CD21hi/CD27+) that represented 1.4%-1.5% of B cells among the 3 groups investigated, consistent with published data on a European cohort34 ; these percentages were unchanged by ART (data not shown). Frequencies for each B-cell subpopulation were available on 27 early and 31 chronically HIV-infected individuals, respectively, before initiation of ART. As shown in Figure 3 and by P values in Table 2, at baseline a significantly higher percentage of B cells were of the immature/transitional subpopulation in chronically infected compared with early HIV-infected individuals. This difference is consistent with past and present findings in that we have previously shown an inverse correlation between immature/transitional B cells and CD4+ T-cell count,6,7 and lower CD4+ T cell-counts were observed here at baseline in the chronically compared with early infected group (Figure 1). The frequency of tissue-like memory B cells was also significantly higher in chronically infected compared with early HIV-infected individuals (Figure 3), consistent with the concept that these are exhausted B cells induced by chronic HIV-induced immune activation.5 In contrast, the frequency of plasmablasts was significantly higher in early compared with chronically HIV-infected individuals (Figure 3), consistent with a previous study showing rapid induction of polyclonal terminal B-cell differentiation shortly after infection.35 The frequency of resting memory B cells was also significantly higher in early compared with chronically HIV-infected individuals (Figure 3), possibly a reflection of the fact that in early HIV infection the immune system remains relatively intact.
Distribution of B-cell subpopulations before and after ART in early and chronic HIV-infected individuals. The percentages of cells in each of the 6 B-cell subpopulations defined in the peripheral blood were measured for HIV-negative individuals and each group of HIV-infected individuals before (M0) and 12 months (M12) after ART.
Distribution of B-cell subpopulations before and after ART in early and chronic HIV-infected individuals. The percentages of cells in each of the 6 B-cell subpopulations defined in the peripheral blood were measured for HIV-negative individuals and each group of HIV-infected individuals before (M0) and 12 months (M12) after ART.
Frequencies for each B-cell subpopulation at 12 months after the initiation of effective ART were available on 16 early and 20 chronically HIV-infected individuals. In this set of analyses we looked for evidence of changes in the representation of B-cell subpopulations within each group of HIV-infected individuals associated with the reduction of HIV plasma viremia induced by ART and we compared the representation of B-cell subpopulations between the 2 groups after 12 months of ART. For the first set of analyses, we used the same approach as previously described,25 namely computing the means of the percentages of each of the 6 B-cell subpopulations before and after initiation of ART and applying a permutation test to assess whether such changes in distribution could reasonably occur by chance. In both those individuals treated with ART early in the course of infection and those treated during the chronic course of infection, this analysis revealed that the changes in B-cell subpopulations shown in Figure 3 as a result of initiation of ART were highly significant (P = .0006 and P < .0001 for early and chronically HIV-infected individuals, respectively). These changes included decreases in the percentages of plasmablasts, as well as of immature/transitional, tissue-like memory, and activated memory B cells, with compensatory increases in both naive and resting/memory B cells. In addition, when the effect of ART on each B-cell subpopulation was compared between early and chronically HIV-infected individuals, the differences in percentage of plasmablasts, and tissue-like memory cells observed before initiation of ART were no longer significant at 12 months after ART. In contrast, the frequency of resting memory B cells remained significantly higher in early-treated compared with chronically-treated HIV-infected individuals, whereas the reverse was observed for immature/transitional B cells (Figure 3 and Table 2). Taken together, these findings indicate that the frequencies of B cells in early and chronically HIV-infected individuals differ before ART; both groups undergo significant shifts in B-cell subpopulations after ART; and some of the differences between the 2 groups observed before initiation of ART persist after 1 year of ART.
Frequencies of each of the 6 B-cell subpopulations were also compared between HIV-negative individuals and HIV-infected individuals both before and at 12 months after ART (Figure 3 and Table 2). Compared with HIV-negative individuals, both HIV-infected groups had significantly higher frequencies of immature/transitional, tissue-like and activated memory B cells, as well as plasmablasts before ART; and significantly lower frequencies of naive, and resting memory B cells. At 12 months after ART there were no significant differences in frequencies of plasmablasts among the groups. However, significant differences between the HIV-negative individuals and the 2 HIV-infected groups persisted for tissue-like and activated-memory B cells, likely due to residual HIV-induced activation. Finally, significant differences in immature-transitional and resting memory B cells persisted between HIV-negative and chronic-treated but not early-treated HIV-infected individuals. Thus, early ART helps normalize resting memory B cells and prevents the expansion of immature/transitional B cells associated with CD4+ T-cell lymphopenia.6,7
Functional analyses of B-cells before and after ART
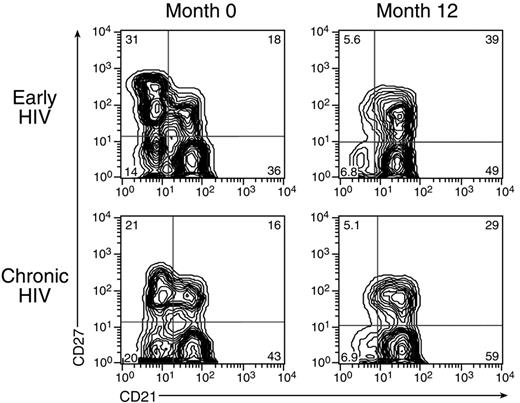
Finally, we considered whether the phenotypic changes in B cells after initiation of ART described in the previous section were associated with alterations in B-cell function. In a previous study, we identified tissue-like memory B cells in the peripheral blood of HIV-infected viremic individuals that were responsible for the majority of the HIV-specific response whereas classic memory B cells (defined as all B cells expressing CD27) were responsible for the majority of responses against recall antigens as represented by influenza virus vaccine. However, as shown in Figure 4, distinctions between these 2 subpopulations of B cells become increasingly difficult to evaluate over time after initiation of ART because tissue-like memory B cells decrease significantly in the peripheral blood after initiation of ART and are also more difficult to assess in early HIV-infected individuals given their lower frequency compared with chronically HIV-infected individuals. Given these limitations and the fact that resting memory B cells constitute the predominant antigen-experienced subpopulation within the peripheral blood after the initiation of ART (see Figures 3 and 4), we restricted our functional analyses of responsiveness to specific antigens to CD27+ B cells.
Depiction of B cells before and after ART in early and chronic HIV-infected individuals. Expression of CD27 and CD21 on mature (CD10−) B cells isolated from the peripheral blood of 1 representative individual in each of the early- and chronic-treated groups before and 12 months after initiation of ART.
Depiction of B cells before and after ART in early and chronic HIV-infected individuals. Expression of CD27 and CD21 on mature (CD10−) B cells isolated from the peripheral blood of 1 representative individual in each of the early- and chronic-treated groups before and 12 months after initiation of ART.
Memory B-cell phenotype and function can be broadly divided according to unswitched (IgM) and switched (IgA and IgG) isotypes. Accordingly, we phenotyped the pre-culture CD27+ memory B cells. Frequencies of unswitched and switched Ig-expressing CD27+ memory B cells were not significantly different before and after 12 months of ART for both groups of HIV-infected individuals, and frequencies between the 2 groups were not significantly different, either before or after ART (supplemental Figure 1A-B, available on the Blood Web site; see the Supplemental Materials link at the top of the online article). Furthermore, there were no differences in total unswitched and switched ASC frequencies, measured as previously described,5 either between groups or between pre- and post-ART (see supplemental Figure 1B for distribution and supplemental Figure 2 for counts).
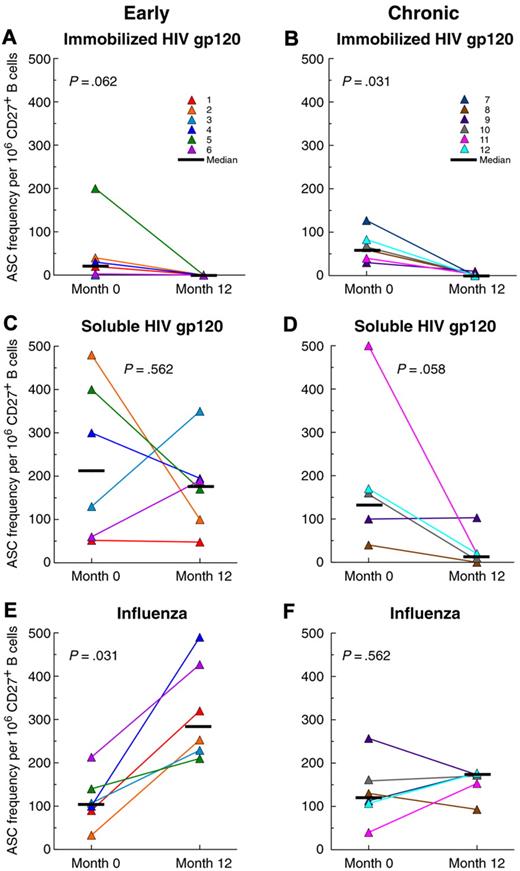
In the majority of previous studies,5,17,23,36 HIV envelope-specific B cells or antibodies were detected after interaction with envelope protein that was directly immobilized on a plastic surface. In our current study, the response to immobilized HIV envelope was low in early HIV-infected individuals before initiation of ART and remained low after 12 months of ART (Figure 5A), whereas in chronically HIV-infected individuals the baseline response was higher and was significantly reduced after the same period of ART (Figure 5B). In contrast, when the reactivity to soluble HIV envelope was assessed using an approach similar to one recently described,37 a different pattern was observed. For early HIV-infected individuals, the response against soluble HIV envelope was substantial before the initiation of ART (Figure 5C), and was significantly higher compared with the response against immobilized HIV envelope before and after ART (P = .03 for responses to the 2 forms of HIV envelope in Figure 5A-C for each individual at months 0 and 12). Furthermore, it did not significantly change after 12 months of ART (Figure 5C). In chronically HIV-infected individuals, responses to soluble HIV envelope were not significantly different compared with responses to the immobilized form either before or after ART (comparing Figure 5B-D by time point), and the response to soluble HIV envelope for this group did not change significantly after 12 months of ART (Figure 5D). Finally, when the 2 groups were compared, the response to soluble HIV envelope was significantly higher in early compared with chronically HIV-infected individuals after 12 months of ART (P = .01 for responses in Figure 5C,D). Differences in Ig isotype among the HIV-specific ASCs could not be assessed due to low responses against immobilized envelope and technical limitations for responses against soluble envelope. Nonetheless, taken together, these data suggest that responses against soluble but not immobilized HIV envelope are induced early after infection and are better maintained after initiation of ART in early-treated compared with chronically-treated HIV-infected individuals.
Memory B-cell responses to HIV and non-HIV antigens in early and chronic HIV-infected individuals. The frequencies of antibody-secreting cells (ASCs) against immobilized (A-B) and soluble (C-D) forms of monomeric HIV-1 gp120 envelope and against seasonal influenza (E-F) were measured by elispot after 4 days of culture. Responses were measured in 6 early (A,C,E) and 6 chronic (B,D,F) HIV-infected individuals before (M0) and 12 months after (M12) initiation of ART. While the majority of ASCs were of the IgG isotype, data represent total IgG, IgA, and IgM ASCs for each antigen. See supplemental Figure 1 for distribution of switched and unswitched isotypes and supplemental Figure 2 for total Ig ASC frequencies.
Memory B-cell responses to HIV and non-HIV antigens in early and chronic HIV-infected individuals. The frequencies of antibody-secreting cells (ASCs) against immobilized (A-B) and soluble (C-D) forms of monomeric HIV-1 gp120 envelope and against seasonal influenza (E-F) were measured by elispot after 4 days of culture. Responses were measured in 6 early (A,C,E) and 6 chronic (B,D,F) HIV-infected individuals before (M0) and 12 months after (M12) initiation of ART. While the majority of ASCs were of the IgG isotype, data represent total IgG, IgA, and IgM ASCs for each antigen. See supplemental Figure 1 for distribution of switched and unswitched isotypes and supplemental Figure 2 for total Ig ASC frequencies.
Finally, we wished to address the broad functional competency of memory B cells in early and chronically HIV-infected individuals by investigating the responsiveness to antigens of influenza virus, a common pathogen that is targeted for routine vaccination in HIV-infected individuals. When memory B-cell responses to the seasonal influenza virus vaccine were measured before and after ART in individuals who were routinely vaccinated, responses were not significantly different between early and chronically HIV-infected individuals before ART (Figure 5E-F at month 0). However, the response to influenza vaccine antigens was significantly increased after 12 months of ART in the individuals treated early in the course of infection (Figure 5E) but not in the individuals treated during the chronic stage of infection (Figure 5F) group. Furthermore, at 12 months after ART the influenza-specific B-cell response was significantly higher in the early-treated compared with the chronic-treated group (P = .005 for responses at month 12 in Figure 5E-F). When the Ig distribution of influenza-specific ASCs was assessed, the majority of responses were of the switched isotype as expected for T-cell-dependent antigens,38 and there was no difference between groups or between pre- and post-ART (supplemental Figure 1C). Thus, HIV-infected individuals treated early in the course of infection have a better capacity to restore immune function than those HIV-infected individuals treated during the chronic stage of infection.
Discussion
Differences in the phenotype and function of B cells among early and chronically HIV-infected viremic individuals remain poorly understood. The longitudinal effects of the reduction in HIV plasma viremia by ART on B-cell phenotype and function are also poorly understood, especially with regard to early versus later initiation of ART. In this study we demonstrate that while increases in total B-cell numbers in the peripheral blood were similar among early and chronically HIV-infected individuals after initiation of ART, the representation of B-cell subpopulations before and after ART were clearly distinct between the 2 groups and HIV-negative individuals. Before ART, B-cell subpopulations associated with immune activation and persistent viral replication (exhausted memory B cells) as well as disease progression (immature/transitional B cells) were clearly expanded in chronically HIV-infected individuals, whereas plasmablasts, which transiently appear in the blood after exposure to high levels of HIV antigen,39 were most prevalent in early HIV-infected individuals. Furthermore, we provide evidence that early initiation of ART is associated with a better recovery of B-cell function against non-HIV and certain HIV antigens compared with the initiation of ART during the chronic stage of HIV infection, adding a compelling argument to other indications that early initiation of ART is beneficial to preserving immune function in HIV-infected individuals.32,33
In a previous study, we reported that the number of total B cells in the peripheral blood of chronically HIV-infected individuals increased significantly after initiation of ART, similar to the increases in CD4+ but not CD8+ T cells after initiation of ART.25 In the present study, we extended these findings by demonstrating that the early phase of HIV infection was distinct from the chronic stage, both in terms of immunologic parameters before the initiation of ART and the dynamics of response after initiation of ART. With regard to the 2 major T-cell populations, CD4+ T-cell numbers were higher in early compared with chronically HIV-infected individuals before ART, whereas the abnormally high CD8+ T cell-numbers observed in both groups before ART were normalized more rapidly after ART in early compared with chronically HIV-infected individuals. These observations are consistent with the concept that the immune system is better able to recover when ART is initiated early in the course of HIV infection as opposed to during the chronic phase of HIV disease.32,33 With regard to B cells, total counts increased significantly in both groups after reduction of HIV plasma viremia as a result of initiation of ART, although there was no significant difference between the 2 groups. However, changes in total lymphocyte counts that occur in the peripheral blood after the reduction of HIV plasma viremia by ART are driven by poorly understood and somewhat controversial mechanisms that are likely to include redistribution of cells between tissues and blood, increased production, and replacement of short-lived activated cells with long-lived cells.40,41 With regard to the latter mechanism, B cells of early and chronically HIV-infected individuals underwent several changes at the subpopulation level that likely had an impact on overall longevity. In both early and chronic HIV infection, the increased frequency of CD27+ activated memory B cells before initiation of ART was significantly reversed after ART (see Figure 3;4 ). These activated B cells have previously been shown to be highly susceptible to cell death by CD95-mediated extrinsic apoptosis.42 Furthermore, plasmablasts, a subpopulation of short-lived Ki-67+ B cells likely to be responsible for increased B-cell turnover in HIV-viremic individuals,4,9,42 were more abundant in early HIV-infected individuals before ART and normalized after ART. Finally, immature/transitional B cells, which have been shown to be highly susceptible to cell death by intrinsic apoptosis,42 were more abundant in chronically HIV-infected individuals before initiation of ART and significantly depleted after ART. Collectively, the replacement of these various short-lived B cells before initiation of ART with longer-lived naive and resting memory B cells after ART in HIV-infected individuals treated during the early and chronic stages of infection may help explain the increases in B-cell numbers observed in both groups, although redistribution from tissues cannot be excluded.
Established humoral immunity is composed of both memory B cells that can respond rapidly upon re-encounter with cognate antigen and long-lived plasma cells responsible for maintaining stable levels of antibodies.39,43 In HIV infection, both components of humoral immunity become perturbed soon after infection,9,14,15,17 likely as a result of both aberrant polyclonal activation and deficiencies in mounting an antigen-specific response. Both the percentage and absolute numbers of unswitched (IgM+) and/or IgG+ switched memory B cells are decreased in the peripheral blood of HIV-infected individuals and this deficiency is not readily corrected by the initiation of ART in chronically infected individuals.8-12 However, most of the data available regarding the paucity of memory B cells in HIV infection have been obtained from chronically infected individuals. The few reports that have been published on early HIV infection have revealed a more complex picture, with most studies reporting that percentages of memory B cells before the initiation of ART are not decreased compared with those of healthy individuals whereas memory B-cell function is decreased.9,14,35 Several factors may account for the apparent contradictions between phenotype and function of B cells, including high variability in the percentage and phenotype of memory B cells among healthy donors. In this regard, several subpopulations of B cells express CD27, especially in HIV-viremic individuals, which can lead to conflicting results. While there is a paucity of CD27+/CD21hi resting memory B cells in HIV-viremic individuals, there is an expansion of CD27+/CD21lo activated memory B cells and CD27++/CD21lo plasmablasts, both of which are short-lived, maintained by HIV viremia, and unlikely to contribute to long-lasting humoral immunity.2,36 In addition, there is at least 1 additional aberrant subpopulation of CD27− memory B cells associated with HIV infection,5,44 which are also maintained at high frequencies by HIV viremia (see Figure 3). Finally, HIV-induced perturbation of IgM-memory B cells has been described,9,11,12 and one,11 but not the other study,12 demonstrated an association with decreased responses to T-cell-independent antigens. However, this subpopulation remains poorly characterized and somewhat controversial.43 Collectively, these observations illustrate the complexity of memory B cells in HIV infection and underscore the need to carefully define populations and combine phenotypic analyses with functional correlates.
In the present study, we investigated several phenotypic and functional attributes of memory B cells before and after reduction of HIV plasma viremia by ART. First, by assessing pre-ART frequencies of various B-cell subpopulations in relatively large cohorts of early and chronically HIV-infected individuals, we found a significantly higher percentage of CD27+ resting memory B cells in the peripheral blood of early compared with chronically HIV-infected individuals. Furthermore, even though the frequency of CD27+ resting memory B cells increased significantly in both groups after 1 year of ART, the level was nonetheless significantly higher in the group treated early in the course of HIV infection compared with the group treated during the chronic stage of infection. This difference was associated with a significant increase in the influenza-specific memory B-cell response in early compared with chronically HIV-infected individuals, both in terms of effects of ART on the response within each group and comparison between the 2 groups after 1 year of ART (see Figure 5F,G). These findings are consistent with similar findings in early-treated HIV-infected children,14 although responses to childhood and T-cell-independent vaccines were not restored in early-treated HIV-infected adults.17 Nonetheless, these data provide an additional argument that early initiation of ART may help restore at least certain aspects of the humoral arm of the immune system in HIV-infected individuals.
The majority of studies on the humoral response against HIV envelope have focused on the serum antibody response with relatively little emphasis on HIV envelope-specific memory B cells.45 However, memory B-cell responses are also important to consider, both for vaccine development and ability of the immune system to control HIV in infected individuals. Several studies have demonstrated that the maintenance of HIV-specific antibodies and memory B cells is dependent on the presence of HIV antigen.15,23,36,46,47 Our findings largely confirm this observation for the majority of chronically HIV-infected individuals studied. However, we did find evidence of a stronger and more sustained memory B-cell response to soluble HIV envelope in early-treated compared with chronically-treated individuals. Given the abundant evidence that the structure and presentation of HIV envelope are important determinants of the type of antibody response generated,48,49 it is not surprising to find differences in responsiveness to immobilized versus soluble forms of the same antigen shown here and reported elsewhere.37 Nonetheless, the significance of our observation needs to be further characterized and investigated in larger cohorts of HIV-infected individuals treated during the early stage of infection as well as those treated during the chronic stage.
In conclusion, our findings shed new light on B cells in the context of early and chronic HIV infection, providing evidence that in both cases B cells respond to initiation of ART more similarly to CD4+ than to CD8+ T cells. However, we also provide evidence for clear distinctions between early and chronic HIV infection relative to the subpopulations of B cells that circulate in the peripheral blood before and after the reduction of HIV plasma viremia by ART. Before ART we found a predominance of plasmablasts and resting memory B cells in early HIV-infected individuals compared with a predominance of immature/transitional and exhausted B cells in chronically HIV-infected individuals. After 1 year of ART, we found a predominance of resting memory B cells in HIV-infected individuals treated early in the course of HIV infection compared with those in whom therapy was initiated during the chronic stage of disease that translated into a better functional profile for the early-treated group. These improved phenotypic and functional attributes of B cells provide further evidence that early initiation of ART is important for preserving overall immune competency in HIV-infected individuals.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank James Arthos for advice and for providing reagents used in this study. The authors are grateful to the patients for their willingness to participate in this study
This work was supported by the Intramural Research Program of NIAID, NIH.
National Institutes of Health
Authorship
Contribution: S.M. designed the study and wrote the paper; C.M.B designed and performed experiments, analyzed data, and revised the paper; J.H. and J.C. designed and performed experiments; W.W., A.J.W., J.G.P., and L.K. performed experiments; M.A.O. recruited and monitored patients; S.K. contributed to study design; T.-W.C. contributed to study design, analyzed data, and revised the paper; M.A.P. performed the statistical analyses and contributed to preparation of the paper; and A.S.F. designed the study and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financials interests.
Correspondence: Susan Moir, NIH, 9000 Rockville Pike, Bldg 10, Rm 6A02, Bethesda, MD 20892-1576; e-mail: smoir@niaid.nih.gov.
References
Author notes
S.M. and C.M.B. contributed equally to this work.