Abstract
Abstract 1530
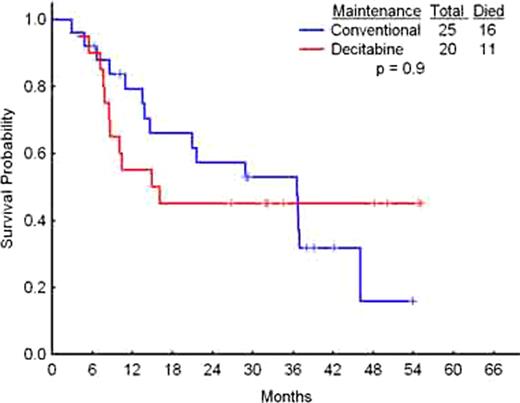
Maintenance therapy in acute myeloid leukemia (AML) is not standard of care. It has been reported that continued therapy with cytotoxic agents similar to those used for induction and consolidation is associated with toxicity but can improve disease free survival (DFS). Methylation status of tumor suppressor genes in clinical remission may predict the relapse in AML, with earlier relapse in patients with methylated genes. Therefore, hypomethylating therapy may be effective in maintaining remission and prolonging survival. Methods: We have conducted a clinical trial comparing decitabine to conventional care (CC, low dose subcutaneous cytarabine, prolonged intensive therapy, or observation) in patients (pts) with AML in their first or subsequent complete remission (CR). Pts with non-favorable risk AML (including intermediate and poor risk) received induction therapy followed by appropriate consolidation. They were then stratified by age (£ 60 vs. > 60) and cytogenetics (intermediate vs. poor risk) and randomized to receive decitabine 20 mg/m2 IV daily × 5 every 4 to 8 weeks for 12 cycles, or CC. Pts in second or subsequent CR were randomized after completion of salvage therapy. Primary endpoint was considered to be no relapse at 1 year. We also monitored minimal residual disease (MRD) by multicolor flow cytometry (MFC) using custom staining panels based on the leukemic phenotypes. Aberrant myeloid blasts were identified by comparison to normal bone marrow CD34+ cells. Serial samples for DNA methylation studies were also collected and methylation analysis was performed. Results: 50 patients have been enrolled. Of those, 45 (19 M, 26 F) pts (including 35 in first CR and 10 in subsequent CR) were evaluable for the primary endpoint. Median age was 57 years (range, 24–77). 27 pts were £ 60 years and 18 > 60. Cytogenetics at diagnosis was intermediate in 34 pts, poor-risk in 10 pts, and favorable [inv(16)] in one patient in second CR. 20 evaluable pts were randomized to decitabine and have received a median of 4.5 cycles (range 1–12). 25 evaluable pts were randomized to CC. With a median duration of follow up for the entire group of 36.3 months (range 6.3–55), 11 pts on the decitabine arm and 10 pts on the CC arm have remained in remission; 9 of 20 (45%) on DAC versus 15 of 25 (60%) on CC have relapsed (p = 0.7). 45 pts including 20 receiving decitabine and 25 receiving CC have been followed for at least 1 year; 9 of 20 (45%) on decitabine versus 9 of 25 (36%) on CC are alive in CR (p=0.9). Toxicity in the decitabine treated pts was limited to 19 episodes of grade 3/4, neutropenia, 14 episodes of grade 3/4 thrombocytopenia, and 1 episode of grade 2 anemia. All were short in duration and reversed without any associated adverse events. Non-hematological grade 3 and 4 adverse events on the decitabine arm include 3 infections, 1 episode each of hypertension and fatigue. There have been no deaths on the study. MFC identified MRD (<5% blasts on smears) in 9 of 19 (47%) patients with subsequent relapse, at levels from 0.04% to 1% of total cells. In 18 pts remaining in CR, no MRD was identified. Relapse occurred from 1.5 to 10 months after the first positive MFC. There was a statistically significant higher LINE methylation at baseline between the pts who relapsed and those who remained in CR (78% vs 73%, P=0.02), whereas no differences were observed for methylation of CDH13 and Mir124a-1 genes. Conclusions: We conclude that administration of decitabine in CR at the above schedule/dose is well tolerated. The study has been terminated early by the data monitoring safety board due to the higher incidence of relapse at 1 year in the decitabine arm. Interestingly, at a median of 36.3 months, decitabine treated patients had lower relapse and higher survival rates than conventionally treated patients, although these differences were not significant. These data suggest the need for larger randomized studies of hypomethylating agents in maintenance therapy in AML.
Off Label Use: Off label use of decitabine in maintenance therapy in AML. Issa:GSK: Consultancy; SYNDAX: Consultancy; Merck: Research Funding; Eisai: Research Funding; Celgene: Research Funding; Celgene: Honoraria; Novartis: Honoraria; J&J: Honoraria. Faderl:Eisai: Research Funding. Borthakur:Eisai: Research Funding. Cortes:Eisai: Research Funding. Kantarjian:Celgene: Research Funding. Ravandi:Eisai: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Johnson & Johnson: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.