Abstract
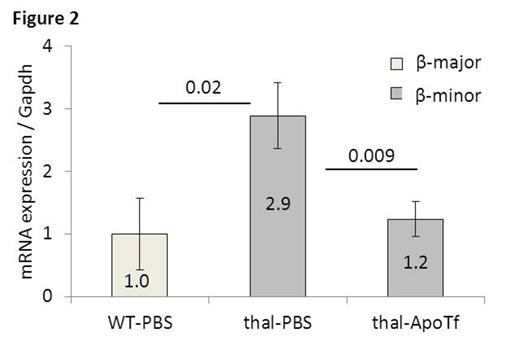
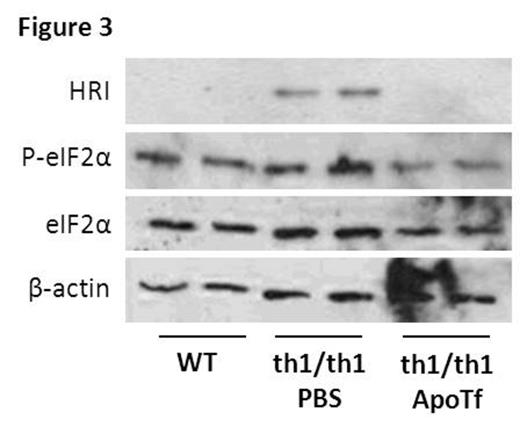
β-thalassemia is an inherited blood disorder caused by reduced or absence of β-globin expression which results in imbalanced globin synthesis, ineffective erythropoiesis, and anemia. How the imbalance between α- and β-globin results in ineffective erythropoiesis, if apoptosis or dysfunctional differentiation of erythroid precursors results in ineffective erythropoiesis, and whether disrupted iron regulation and / or iron overload in β-thalassemia is directly involved in the pathophysiology of ineffective erythropoiesis is incompletely understood. Iron is critical for hemoglobin synthesis and erythropoiesis is dependent on transferrin (Tf) bound iron. Tf functions as the main iron transporter in circulation, where it exists in three forms: as iron-free apo-transferrin (apoTf), monoferric Tf, or diferric Tf (holoTf). Typically, iron is bound to 30% of all Tf binding sites in circulation at which point monoferric Tf is found in the highest concentration relative to holoTf. . We have previously shown that exogenous apoTf ameliorates anemia in a mouse model of β-thalassemia intermedia (th1/th1), resulting in reduced splenomegaly, reticulocytosis, and α-globin precipitation on circulatory red blood cells (RBC). We also observe a decrease in mean corpuscular hemoglobin (MCH) and mean corpuscular volume (MCV), serum iron, Tf saturation, together suggesting that relative iron deficiency improves iron metabolism and ineffective erythropoiesis in apoTf-treated th1/th1 mice. We hypothesize that exogenous apoTf decreases cytosolic iron and heme as a consequence of increased monoferric Tf which results in less iron entering cells via Tf:TfR1 binding. Our current data reveals that in vitro incubation of purified apoTf and holoTf at 37C results in the formation of monoferric Tf, and injection of wild-type (WT) mice with a single intraperitoneal dose of apoTf (10mg) decreases holoTf (P=0.01) and increases monoferric Tf (P=0.02) in the serum 6 hours after injection. Using both calcium mobilization and anti-Tf antibodies in flow cytometry, we demonstrate that apoTf results in no TfR1 binding relative to holoTf in CHO cells (P<0.0001), and an equal concentration apoTf:holoTf mixture results in intermediate binding between apoTf and holoTf (P=0.004). We also demonstrate a dose dependent decrease in cytosolic iron (P<0.001) and heme (P<0.01) in MEL cells treated with escalating concentrations of apoTf, an effect abrogated by the additional of DFO, an iron chelator; urea gel of MEL cell supernatants reveals that monoferric Tf increases with increasing doses of apoTf and decreased in concurrently DFO treated cells (Figure 1 ). These findings together suggest that changes in iron uptake result from increased monoferric Tf (rather than competition of apoTf for TfR1 binding sites). In addition, in vivo experiments demonstrate a decrease in heme concentration (56 vs. 67 uM, P<0.0001) in circulating RBCs as well as α-globin (1.3 vs. 3.3-fold, P=0.009) and β-globin (Figure 2 ) mRNA expression in sorted bone marrow orthochromatophilic erythroblasts from apoTf- vs. PBS-treated th1/th1 mice. As heme is known to regulate globin expression through transcriptional and translational routes, we evaluate bach1, heme oxygenase 1 (HO-1), and heme-regulated eIF2α kinase (HRI). We demonstrate no difference in bach1 and HO-1 mRNA expression but a significant and unexpected decrease in HRI expression (1.0 vs. 2.8-fold, P=0.01) in sorted bone marrow orthochromatophilic erythroblasts from apoTf- vs. PBS-treated th1/th1 mice (similar findings in all stages of terminal erythroid differentiation), suggesting that HRI is regulated by mechanisms independent of cellular iron and heme. Furthermore, western blots of HRI and its target eIF2α (total and phosphorylated) are also normalized in sorted bone marrow erythroid precursors from apoTf- vs. PBS-treated th1/th1 mice (Figure 3 ). Taken together, our data suggests that exogenous apoTf in th1/th1 mice results in decreased cytosolic iron and heme as well as α- and β-globin synthesis as a consequence of increased monoferric Tf in circulation and provides a novel system to explore the regulation of globin in β-thalassemia and how iron deficiency benefits this disease.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.