Abstract
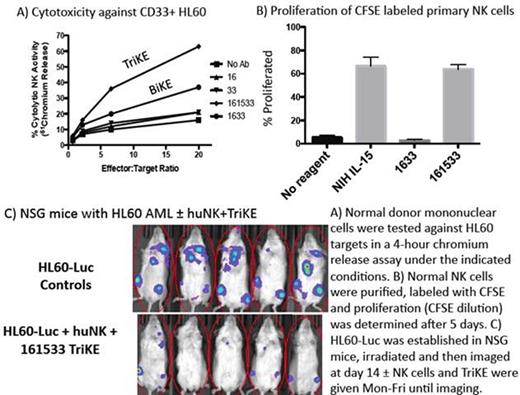
Natural killer (NK) cells are capable of immune surveillance mediated by a balance of activating and inhibitory receptors. We have shown that adoptive transfer of NK cells can induce complete remissions in patients with refractory AML when combined with lymphodepleting chemotherapy and IL-2 to stimulate survival and in vivo expansion of the NK cells. Using this approach, 30-50% of patients with refractory attain clinical remissions. We hypothesize that clinical benefit is limited by the lack of antigen specificity and because IL-2 induces regulatory T cells (Treg) that inhibit NK cell proliferation. We have developed trispecific killer engagers (TriKE) to overcome these limitations. We have previously shown that bispecific killer engagers (BiKEs) are capable of creating immunologic synapses between NK cells and CD33 antigens on AML and MDS targets leading to NK cell signaling through the highly potent CD16 (FcγRIII) receptor. We observed that although CD16 engagement leads to enhanced killing and cytokine production by NK cells, there is no effect on proliferation (designated 1633 in Figure, Panel B). Because IL-15 is the homeostatic factor for NK cell proliferation, survival, activation, and development and because unlike IL-2, it does not stimulate CD4+ CD25+ Treg, we developed a TriKE that includes a modified human IL-15 crosslinker sandwiched between single chain Fv against CD16 and CD33 (designated 161533). The final target gene was spliced into pET21d vector expression plasmid and transformed into the Escherichia coli and compared to a 1633 BiKE with the identical Fv regions as above. TriKEs were recovered from inclusion bodies, refolded, and purified. The addition of the IL-15 crosslinker to the molecule reduced its isoelectric point by two pH units creating more favorable conditions for purification and enhancing yield. Despite identical amounts of starting inclusion bodies, the final yield of 161533 TriKE was twice the yield of 1633 BiKE indicating more favorable purification dynamics. To establish the selectivity of the anti-CD33 binding moiety, BiKEs and TriKEs were analyzed using flow cytometry and both bound to CD16 and CD33 selectively without interference from the IL-15 crosslinker. To determine the capacity of BiKE and TriKE reagents to mediate NK cell killing, activity was compared in a 4-hour chromium release assay (representative of 3 separate experiments) against CD33+ HL60 targets (Figure Panel A) or CD33- HT29 (not shown). The highest specific activity is with the 161533 TriKE containing a modified IL-15 linker as control samples of anti-CD16 and anti-CD33 alone did not augment cytotoxicity while 1633 BiKE mediating killing was intermediate. CD33- HT29 was not killed. We next tested BiKE and TriKE in a proliferation assay using CSFE labeled primary NK cells. NCI produced recombinant human IL-15 was used as a positive control. The TriKE exhibited potent proliferation of primary NK cells compared to BiKE (Figure Panel B). As target cell induced NK cell production of cytokines is an important aspect of the anti-leukemia response, we compared the BiKE and TriKE for their ability to mediate cytokine production with primary NK cells and HL60 targets. TriKE induced greater target cell specific TNFα, INFγ, IL-6, MIP1α, GM-CSF and IL-8 compared to BiKE. We then tested the activity of the TriKE in a xenogeneic model of human NK cell adoptive transfer where NSG mice are given 0.75 million HL60-Luc cells followed by 250 cGy XRT ± 1 million NK cells 3 days later from a CD3 and CD19 depleted clinical product and daily IP injection of 50 mcg/kg TriKE. Significant anti-tumor activity without toxicity was seen in the NK and TriKE treated mice (P<0.002). In addition, the 161533 TriKE had potent in vivo IL-15 activity to support the in vivo persistence and expansion of NK cells while BiKE did not (data not shown). In summary, we have shown that a novel TriKE construct can mediate CD16 directed cytotoxicity against CD33 targets and this is specifically maintained when adding a modified IL-15 linker. The IL-15 activity is fully preserved in vitro and in vivo and unexpectedly enhances the purification product. This will allow us to redirect NK cells to malignant targets while providing cytokine stimulation with an easily exportable off-the-shelf non-gene therapy strategy using a drug that also maintains NK cell persistence, survival and in vivo expansion. Drug production is in progress for clinical testing in 2016.
Miller:Coronado: Speakers Bureau; BioSciences: Speakers Bureau; Celegene: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.