Abstract
The first edition of the European LeukemiaNet (ELN) recommendations for diagnosis and management of acute myeloid leukemia (AML) in adults, published in 2010, has found broad acceptance by physicians and investigators caring for patients with AML. Recent advances, for example, in the discovery of the genomic landscape of the disease, in the development of assays for genetic testing and for detecting minimal residual disease (MRD), as well as in the development of novel antileukemic agents, prompted an international panel to provide updated evidence- and expert opinion-based recommendations. The recommendations include a revised version of the ELN genetic categories, a proposal for a response category based on MRD status, and criteria for progressive disease.
Introduction
In 2010, an international expert panel, on behalf of the European LeukemiaNet (ELN), published recommendations for diagnosis and management of acute myeloid leukemia (AML).1 These recommendations have been widely adopted in general practice, within clinical trials, and by regulatory agencies. During recent years, considerable progress has been made in understanding disease pathogenesis, and in development of diagnostic assays and novel therapies.2 This article provides updated recommendations that parallel the current update to the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia.3,4 For diagnosis and management of acute promyelocytic leukemia, readers are referred to the respective recommendations.5
Methods
The panel included 22 international members with recognized clinical and research expertise in AML. The panel met 3 times. Literature searches, categorization of evidence, and arrival at consensus were done as previously.1 Relevant abstracts presented at the 2013 to 2015 meetings of the American Society of Hematology, and the 2013 to 2016 meetings of the American Association for Cancer Research, the European Hematology Association, and the American Society of Clinical Oncology were reviewed.
WHO classification
AML with recurrent genetic abnormalities
The molecular basis of AML with inv(3)(q21.3q26.2) or t(3;3)(q21.3;q26.2) was revisited showing that repositioning of a GATA2 enhancer element leads to overexpression of the MECOM (EVI1) gene and to haploinsufficiency of GATA2.7,8 A new provisional entity “AML with BCR-ABL1” was introduced to recognize that patients with this abnormality should receive therapy with a tyrosine kinase inhibitor. Distinction from blast phase of chronic myeloid leukemia may be difficult; preliminary data suggest that deletion of antigen receptor genes (immunoglobulin heavy chain and T-cell receptor), IKZF1, and/or CDKN2A may support a diagnosis of AML rather than chronic myeloid leukemia blast phase.9 AML with mutated NPM1 and AML with biallelic mutations of CEBPA have become full entities; the latter category was restricted to cases with biallelic mutations because recent studies have shown that only those cases define the entity and portend a favorable outcome.10-16 Both entities now subsume cases with multilineage dysplasia because presence of dysplasia lacks prognostic significance.17-19 Finally, a new provisional entity “AML with mutated RUNX1” (excluding cases with myelodysplasia-related changes) was added; it has been associated with distinct clinicopathologic features and inferior outcome.20-24
AML with myelodysplasia-related changes
Presence of multilineage dysplasia, preexisting myeloid disorder, and/or myelodysplasia-related cytogenetic changes remain diagnostic criteria for this disease category. Deletion 9q was removed from the list of myelodysplasia-related cytogenetic changes because, in addition to its association with t(8;21), it also frequently occurs in AML with NPM1 and biallelic CEBPA mutations.16,25
AML, not otherwise specified
The former subgroup acute erythroid leukemia, erythroid/myeloid type (≥50% bone marrow erythroid precursors and ≥20% myeloblasts among nonerythroid cells) was removed; myeloblasts are now always counted as percentage of total marrow cells. The remaining subcategory AML, not otherwise specified (NOS), pure erythroid leukemia requires >80% immature erythroid precursors with ≥30% proerythroblasts. French-American-British (FAB) subclassification does not seem to provide prognostic information for “AML, NOS” cases if data on NPM1 and CEBPA mutations are available.26
Myeloid neoplasms with germ line predisposition (synonyms: familial myeloid neoplasms; familial myelodysplastic syndromes/acute leukemias)
Inclusion of this new category reflects the increasing recognition that some cases of myeloid neoplasms, including myelodysplastic syndrome (MDS) and AML, arise in association with inherited or de novo germ line mutations (Table 2).6,27-30 Recognition of familial cases requires that physicians take a thorough patient and family history, including information on malignancies and previous bleeding episodes. Awareness of these cases is of clinical relevance because patients may need special clinical care.27 Affected patients, including their families, should be offered genetic counseling with a counselor familiar with these disorders.
Molecular landscape
The advent of high-throughput sequencing techniques has allowed new insights into the molecular basis of myeloid neoplasms.31-37 Similar to most sporadic human malignancies, AML is a complex, dynamic disease, characterized by multiple somatically acquired driver mutations, coexisting competing clones, and disease evolution over time.
The Cancer Genome Atlas AML substudy profiled 200 clinically annotated cases of de novo AML by whole-genome (n = 50) or whole-exome (n = 150) sequencing, along with RNA and microRNA sequencing and DNA-methylation analysis.31 Twenty-three genes were found to be commonly mutated, and another 237 were mutated in 2 or more cases, in nonrandom patterns of co-occurrence and mutual exclusivity. Mutated genes were classified into 1 of 9 functional categories: transcription factor fusions, the NPM1 gene, tumor suppressor genes, DNA methylation-related genes, signaling genes, chromatin-modifying genes, myeloid transcription factor genes, cohesin complex genes, and spliceosome complex genes.
The use of genetic data to inform disease classification and clinical practice is an active field of research. Recently, 1540 patients, intensively treated in prospective trials, were analyzed using targeted resequencing of 111 myeloid cancer genes, along with cytogenetic profiles.37 Patterns of comutations segregated AML cases into 11 nonoverlapping classes, each with a distinct clinical phenotype and outcome. Beyond known disease classes, 3 additional, heterogeneous classes emerged: AML with mutations in chromatin and RNA-splicing regulators; AML with TP53 mutations and/or chromosomal aneuploidies; and, provisionally, AML with IDH2R172 mutations.
Mutant allele fractions can be used to infer the phylogenetic tree leading to development of overt leukemia. Clonal evolution studies in patients and patient-derived xenograft models indicate that mutations in genes involved in regulation of DNA modification and of chromatin state, most commonly DNMT3A, TET2, and ASXL1, are often present in preleukemic stem or progenitor cells and occur early in leukemogenesis.38-41 Such mutations are present in ancestral cells capable of multilineage engraftment, may persist after therapy, lead to clonal expansion during remission, and cause recurrent disease.
Recent studies in large, population-based cohorts have identified recurrent mutations in epigenetic regulators (DNMT3A, ASXL1, TET2), and less frequently in splicing factor genes (SF3B1, SRSF2), to be associated with clonal hematopoietic expansion in elderly seemingly healthy subjects.42-46 The term “clonal hematopoiesis of indeterminate potential”47 has been proposed to describe this phenomenon which seems associated with increased risks of hematologic neoplasms. Preliminary data indicate that the rate of progression of clonal hematopoiesis of indeterminate potential to hematologic disease may be similar to the rate of progression of other premalignant states, such as monoclonal gammopathy of undetermined significance to multiple myeloma.
Diagnostic procedures
Morphology
At least 200 leukocytes on blood smears and 500 nucleated cells on spiculated marrow smears should be counted. A marrow or blood blast count of ≥20% is required, except for AML with t(15;17), t(8;21), inv(16), or t(16;16). Myeloblasts, monoblasts, and megakaryoblasts are included in the blast count. In AML with monocytic or myelomonocytic differentiation, monoblasts and promonocytes, but not abnormal monocytes, are counted as blast equivalents.
Immunophenotyping
Cytogenetics and molecular cytogenetics
Conventional cytogenetic analysis remains mandatory in the evaluation of suspected AML. Eight balanced translocations and inversions, and their variants, are included in the WHO category “AML with recurrent genetic abnormalities”.3,4 Nine balanced rearrangements and multiple unbalanced abnormalities are sufficient to establish the WHO diagnosis of “AML with myelodysplasia-related changes” when ≥20% blood or marrow blasts are present (Table 1).
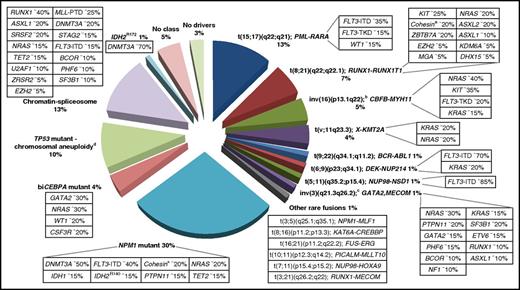
Other rare balanced rearrangements are recognized.49,50 Although considered disease-initiating events, they do not formally define disease categories. They involve genes, for example, encoding epigenetic regulators (eg, KMT2A [MLL], CREBBP, NSD1) or components of the nuclear pore complex (NUP98, NUP214) (Figure 1). Some rearrangements are cytogenetically cryptic, such as t(5;11)(q35.2;p15.4); NUP98-NSD1, which occurs in ∼1% of AML in younger adults and predicts a poor prognosis.51-53 Recent studies have highlighted the potential of novel sequencing technologies to discover additional AML-associated fusion genes.54-56
Molecular classes of AML and concurrent gene mutations in adult patients up to the age of ∼65 years. Class definition is based on the study by Papaemmanuil et al.37 For each AML class denoted in the pie chart, frequent co-occurring mutations are shown in the respective boxes. Data on the frequency of genetic lesions are compiled from the databases of the British Medical Research Council (MRC), the German-Austrian AML Study Group (AMLSG), and from selected studies.37,87,88,299 a indicates cohesin genes including RAD21 (∼10%), SMC1A (∼5%), and SMC3 (∼5%); b, inv(16)(p13.1q22) or t(16;16)(p13.1;q22); CBFB-MYH11; c, inv(3)(q21.3q26.2) or t(3;3)(q21.3;q26.2); GATA2,MECOM(EVI1); and d, TP53 mutations are found in ∼45%, and complex karyotypes in ∼70% of this class. The structure of the pie chart is adapted from Grimwade et al,50 generated by Adam Ivey (King’s College London, London, United Kingdom).
Molecular classes of AML and concurrent gene mutations in adult patients up to the age of ∼65 years. Class definition is based on the study by Papaemmanuil et al.37 For each AML class denoted in the pie chart, frequent co-occurring mutations are shown in the respective boxes. Data on the frequency of genetic lesions are compiled from the databases of the British Medical Research Council (MRC), the German-Austrian AML Study Group (AMLSG), and from selected studies.37,87,88,299 a indicates cohesin genes including RAD21 (∼10%), SMC1A (∼5%), and SMC3 (∼5%); b, inv(16)(p13.1q22) or t(16;16)(p13.1;q22); CBFB-MYH11; c, inv(3)(q21.3q26.2) or t(3;3)(q21.3;q26.2); GATA2,MECOM(EVI1); and d, TP53 mutations are found in ∼45%, and complex karyotypes in ∼70% of this class. The structure of the pie chart is adapted from Grimwade et al,50 generated by Adam Ivey (King’s College London, London, United Kingdom).
If cytogenetic analysis fails, fluorescence in situ hybridization is an option to detect gene rearrangements, such as RUNX1-RUNX1T1, CBFB-MYH11, KMT2A (MLL), and MECOM (EVI1) gene fusions, or loss of chromosome 5q, 7q, or 17p material.
Molecular genetic testing
Diagnostic workup should include screening for (a) mutations in NPM1, CEBPA, and RUNX1 genes because they define disease categories (provisionally for RUNX1); (b) mutations in FLT3 (both for internal tandem duplications [ITDs] together with data on the mutant–to–wild-type allelic ratio,57-60 and tyrosine kinase domain mutations at codons D835 and I836); activating mutations of FLT3 are not only prognostic, but may beneficially be affected by tyrosine kinase inhibition61 ; and (c) mutations in TP53 and ASXL1 because they consistently have been associated with poor prognosis (Table 4).62-70
Molecular testing by reverse transcriptase–polymerase chain reaction (RT-PCR) for recurring rearrangements can be useful (Table 4).
Although only a few of the recently identified molecular markers inform current clinical practice, the list (from the previous paragraph) will likely be expanded with testing for single genes replaced by gene panel diagnostics, or diagnostic platforms that simultaneously test for gene mutations and gene rearrangements.55,56
Biobanking
If possible, pretreatment leukemic marrow and blood should be stored within a biobank. Informed consent preferably should allow a broad array of correlative laboratory studies including analysis of germ line DNA. Pretreatment samples should include nucleic acid (DNA and RNA, stored at −80°C) and viable cells (stored at −196°C). Optimally, a plasma sample, a methanol/acetic acid-fixed cell pellet (from cytogenetic analysis), and frozen cell pellets from various time points during and after treatment (eg, at time of complete remission [CR], relapse, and for minimal residual disease [MRD] monitoring at defined time points during remission) should be obtained and stored under appropriate conditions.
Buccal swabs and sputum have been previously recommended for the analysis of germ line DNA; samples should preferably be obtained during remission to reduce the risk of contaminating DNA from leukemic cells. Skin fibroblasts may be the preferred tissue source. A skin biopsy can be performed using a punch biopsy or by taking a small biopsy at the site of skin incision during bone marrow aspiration or biopsy. When obtained at diagnosis, skin cells should be grown from the biopsy to avoid contamination of the specimen with leukemic cells; alternatively, the biopsy can be taken during remission without growing of fibroblasts. Other sources include finger nails and hair follicles, although the amount of DNA that can be extracted may be limited. Finally, bone marrow fibroblasts can be grown from viably frozen mononuclear cells.72
Other diagnostic tests
Tests and procedures for a patient with AML are described in Table 4.
Prognostic factors
Pretreatment factors
Recent studies have explored the relative contribution of genetic and clinical variables to prediction of event-free survival (EFS) and overall survival (OS).36,37,73,74 Genomic lesions account for about two-thirds of explained variation, with the other third contributed by demographic, clinical, and treatment variables. However, models incorporating all of these factors and aimed at predicting whether a patient with a given set of covariates will have a longer remission or life expectancy than another patient with a different set of covariates are correct in only 75% to 80% of cases. This emphasizes the need not only to identify other pretreatment prognostic factors but also to focus on posttreatment events, in particular the presence of MRD (see “Factors after diagnosis”).
Patient-related factors.
Increasing age is independently associated with poorer outcomes. Performance status, general health, and specific comorbidities modulate the effect of age on tolerance of chemotherapy (see also “Current therapy” and “Older patients not considered candidates for intensive chemotherapy”), whereas specific age-related AML-associated genetic abnormalities increase the likelihood of resistance, as do previous MDS, chronic myelomonocytic leukemia, myeloproliferative neoplasm (MPN), or prior exposure to cytotoxic therapy for other disorders. Hence, age should not be the sole determinant of treatment decisions.
AML-related genetic factors.
Genetic abnormalities are powerful prognostic factors.36,37,50,73,75,76 Results from conventional cytogenetics and from NPM1, FLT3, and CEBPA mutational screening are currently being used in routine practice following 2010 ELN recommendations.1
Recent data have led to several changes in these recommendations (see “2017 ELN genetic risk stratification” and Table 5). RUNX1 mutations although occurring with unfavorable features, such as older age, antecedent myeloid disorder, and concurrent gene mutations (eg, SRSF2, ASXL1), identify patients with poor prognosis.20-23,37,70,73 Likewise, ASXL1 mutations are more common in older patients and associated with inferior survival.36,37,62-65,69,70 TP53 mutations are associated with complex karyotype, monosomal karyotype, and specific chromosomal aneuploidies (eg, −5/5q−, −7/7q−), and predict for very poor outcome.37,66-70,73 TP53 mutation and complex karyotype provide independent prognostic information, with the combination of both having the worst outcome.37
The prognostic impact of many markers is context-dependent with the effect of a given abnormality dependent on the presence/absence of another.37 Simple examples of such gene-gene interactions are that a NPM1 mutation conveys a “favorable” prognosis only in the absence of a FLT3-ITD (or FLT3-ITD with a low allelic ratio),57-59,77 whereas mutations in both ASXL1 and RUNX1 confer a particularly poor prognosis.37,65 Furthermore, tightly correlated clusters of mutated genes, that is, mutations in RNA splicing (SRSF2, SF3B1, U2AF1, ZRSR2), chromatin (ASXL1, STAG2, BCOR, KMT2APTD, EZH2), or transcription (RUNX1) regulators are found in high-risk MDS, high-risk MPN as well as secondary AML, indicating gene signatures identify high-risk myeloid disorders that cross-conventional diagnostic boundaries.37,78-82
In core-binding factor (CBF) AML, in particular in AML with t(8;21), the presence of KIT mutations, especially if higher mutant KIT levels are present, appear to be associated with poorer prognosis.83-87 Nevertheless, presence of a KIT mutation should not assign a patient to a different genetic risk category; rather, patients should be monitored for MRD, whose absence abrogates the effect of KIT.85 Although both types of CBF-AML are associated with mutations in signaling genes (NRAS, KIT, NF1, FLT3, KRAS), recent comprehensive mutation profiling studies have revealed a different spectrum of cooperating mutations (Figure 1).87,88 AML with RUNX1-RUNX1T1 is significantly enriched for mutations in chromatin-modifying genes (42%-44%), including ASXL2, and for mutations in cohesin complex genes (18%-20%), whereas they are nearly absent in AML with CBFB-MYH11.87-89
Although a genetic marker may currently not be prognostic, its presence may provide a target for new therapies as with IDH1, IDH2, and KMT2A (MLL).2 Likewise, a recent study in primary human samples identified co-occurrence of biallelic CEBPA mutations and mutations in the granulocyte colony-stimulating factor receptor gene CSF3R (signaling through the JAK-STAT pathway) as uniformly responsive to JAK inhibitors.90
Factors after diagnosis
Monitoring of MRD.
Two approaches can be used to detect MRD, that is, multiparameter flow cytometry (MFC) and molecular techniques, including real-time quantitative PCR (RT-qPCR), digital PCR, and next-generation sequencing–based technologies. Standardized RT-qPCR assays are now available to detect AML-associated genetic lesions (Table 4). Each methodology differs in the proportion of patients to whom it can be applied and in its sensitivity to detect MRD.91,92 It is expected that integrated evaluation of baseline factors and assessment of MRD will improve risk assessment and inform postremission therapy.91-93
MRD can be assessed (1) at early time points, for example, following induction and consolidation courses to assess remission status and determine kinetics of disease response, and (2) sequentially beyond consolidation to detect impending morphologic relapse. Remission status as assessed by MFC (which is informative in ∼90% of AML patients) provides a more reliable predictor of outcome than conventional morphology-based CR assessment.92-99 MFC can be used to assess “CR without MRD” (CRMRD−) (see “Response criteria and outcome measures” and Table 6). The depth of response assessed by MFC has been consistently shown to provide independent prognostic information and thus may inform risk stratification. Currently, analyses should be performed in experienced laboratories, until MFC techniques have been further standardized.
In ∼60% of younger adults, the leukemia cells are informative for a molecular marker that can be tracked by RNA-based RT-qPCR assays. Assay sensitivity depends upon the relative expression of the target in leukemic blasts compared with standard housekeeping genes (eg, ABL1) and varies according to the target, as well as between patients with the same target.91 Assays for MLLT3-KMT2A are typically associated with the lowest sensitivity (∼1 in 103) due to relatively low-level fusion gene expression,100 whereas assays for NPM1 mutations achieve sensitivities of up to 1 in 106-7 due to the high-level mutant allele expression.101-106 Many studies have shown that kinetics of MRD response to frontline therapy differs by molecular marker analyzed.85,101-109 For example, reduction in RUNX1-RUNX1T1 is slower than in NPM1 transcript levels. Importantly, MRD status has been found to be a better predictor of relapse risk than presence of cooperating mutations involving KIT and FLT3-ITD in CBF-AML,85 or FLT3-ITD, DNMT3A, and WT1 in NPM1-mutated AML.106 These data support inclusion of molecular MRD assessment into routine care to help inform transplant decisions in first remission.
Sequential MRD-monitoring studies have shown that persistent high-level PCR positivity, or a rising level of leukemic transcripts after an initial molecular response, invariably predict relapse.91 Whether the opportunity thus provided for early intervention to prevent overt relapse will be useful is under investigation. Preemptive therapy may be particularly relevant with allogeneic hematopoietic cell transplantation (HCT) where MRD status may inform conditioning strategy, or post-HCT measures aiming to avoid frank relapse.
Molecular markers can now be identified in virtually all cases. This has opened the way to detection of MRD using next-generation sequencing or digital PCR.91 Although currently investigational, studies have already shown that mutational assessment at early time points can distinguish patients at differing probability of relapse.110,111 Studies are needed to define which mutations are reliable indicators of leukemic clones associated with clinical relapse from mutations that are associated with preleukemic clones (eg, DNMT3A, IDH1/2) poorly predictive of relapse, although persistent at high levels after chemotherapy and during remission.106,112,113
2017 ELN genetic risk stratification
The original intention of the ELN genetic categories was to standardize reporting of genetic abnormalities particularly for correlations with clinical characteristics and outcome. The distinction between the intermediate I and intermediate II categories was based on genetic characteristics, rather than on prognostic stratification. Although a subsequent study demonstrated longer OS in the intermediate I group than the intermediate II group, the 2 groups were prognostically indistinguishable in older patients, who constitute the majority of cases of AML.114
Given these findings, the panel decided to simplify the ELN system by using a 3-group classification (favorable, intermediate, adverse) rather than the previous 4-group system (Table 5). A few other changes have been made. Recent studies have shown that in AML with NPM1 or biallelic CEBPA mutations, the presence of coexisting chromosomal abnormalities does not appear to modify the prognostic effect of the mutations16,25,115 ; prognosis may be more influenced by concurrent gene mutations.37 Accordingly, and as in CBF-AML, the categorization of these cases is now based on the primary leukemia-defining genetic subsets irrespective of the karyotype. The higher relapse rate and poorer OS associated with FLT3-ITD largely depends on the ITD allelic ratio. Most recent studies suggest that patients with NPM1 mutation and FLT3-ITD with a low (<0.5) allelic ratio (FLT3-ITDlow) have a similar (favorable) outcome as patients with a NPM1 mutation but no FLT3-ITD; thus, both groups are now considered favorable.57-60 In contrast, AML with wild-type NPM1 and FLT3-ITD with a high (≥0.5) allelic ratio (FLT3-ITDhigh) has a poor prognosis and is placed in the adverse-risk group,57 although the panel acknowledges that the natural course of AML with FLT3 mutation may change by use of FLT3 inhibitors.
RUNX1, ASXL1, and TP53 mutations (see “Pretreatment factors”), and monosomal karyotype116-120 have also been added to the adverse-risk group in recognition of their independent association with adverse risk. Although numerous studies have dealt with mutations in other genes, for example, DNMT3A, IDH1, IDH2, or genes in the chromatin/spliceosome group other than ASXL1 and RUNX1, the panel did not feel enough evidence has as yet accumulated to warrant their assignment to an ELN prognostic group.
Response criteria and outcome measures
CRMRD−
The category CRMRD− is proposed because relapse is more likely in patients in CR or CR with incomplete hematologic recovery (CRi) with detectable residual disease.91,92 The best time to test for MRD in patients in CR by conventional criteria is not settled. Assessment of MRD after cycle 2 or even cycle 1 of induction allows earlier identification of poor responders.91,92,97,106 However, MRD can disappear after consolidation therapy. The frequency with which this occurs may differ in different molecular subsets and future assessment of these frequencies will likely inform therapeutic decisions.
Primary refractory AML
The panel proposes criteria for “primary refractory disease” (also commonly termed “induction failure”) because the definition of refractory disease currently differs in clinical practice and clinical trials. Failure to attain CR following exposure to at least 2 courses of intensive induction therapy defines patients to be “primary refractory.” Although possibly influenced by selection bias, CR rates from a second course of 7+3 can be 40% to 45%, which is often higher than the rate targeted by newer therapies.121 Regimens containing higher doses of cytarabine are generally considered as the best option for patients not responding to a first cycle of 7+3. The likelihood of CR with a second course of a higher dose cytarabine-based regimen after failure of a first of the 2 cycles may be relatively lower than is the case with a second 7+3 after failure of a first.122,123
Progressive disease
This proposed new category primarily applies to patients given less intense or single-agent targeted therapies. A uniformly accepted definition of progressive disease (PD) should facilitate a standardized interpretation of new drug trials. Because criteria for PD are arbitrary, it is unknown whether PD augurs a poorer prognosis than stable disease and warrants investigation. In the interim, observation of PD does not necessarily imply a patient should be removed from a given therapy.
MDS-AML overlap/secondary AML
Genetic basis
The related and partially overlapping clinical phenotypes of MDS and AML are reflected in the genetic bases of the 2 diseases.31,37,78-80,124 A subset of mutations are highly specific for de novo AML, whereas another set of mutations is specific for secondary AML and are found commonly in MDS. Genetic analyses of a panel of genes mutated in myeloid malignancies, and perhaps the addition of gene expression and DNA-methylation profiling, have the potential to inform the distinction between MDS and AML, and to determine which cases of AML arose from an antecedent MDS.37,80,81 The prognoses of patients with clinically diagnosed de novo AML whose gene mutation profile resembles those of patients with clinically diagnosed secondary AML is more like secondary than de novo AML.81
Mutations associated with secondary AML occur in genes encoding SRSF2, SF3B1, U2AF1, and ZRSR2 (splicing factors); ASXL1, EZH2, and BCOR (epigenetic regulators); and STAG2 (a member of the cohesin complex).81 In such cases, these mutations likely occur during an MDS phase, remain in the clone that progresses to acute leukemia, and often persist in clonal remission following chemotherapy. Similarly, mutations in ASXL1, EZH2, and SRSF2 genes have been shown to identify patients with primary myelofibrosis who are at risk for leukemic transformation and who have particularly poor outcomes.82,125 In contrast, NPM1 mutations, and CBF and KMT2A rearrangements are highly specific for de novo AML.81
Blast count
Given the biologic overlap between secondary AML and MDS any minimum blast percentage used to distinguish AML from MDS with higher blast counts (ie, MDS with excess blasts-2 [MDS-EB2]) must be arbitrary. Thus, this minimum has decreased from 30% in the FAB system to 20% in the WHO system with many AML clinical trial groups allowing entry of patients with >10% blasts. Bone marrow failure is the usual cause of death in both AML and MDS-EB2, and most of the latter die without “progression to AML,” with data suggesting the natural history of MDS-EB2 is more similar to AML than to lower risk MDS.128,129
These observations suggest that it is best to determine eligibility for an “AML” or “MDS” study based on disease- and patient-specific factors rather than on a fixed blast percentage. Integration of data from molecular genetics into future classification systems will be useful to refine current diagnostic algorithms and support a more biologically precise disease classification.
Current therapy
The general approach to current therapy has not changed substantially in recent years. Initial assessment evaluates whether a patient is considered a candidate for intensive induction chemotherapy. Although assessment of risk of treatment-related mortality (TRM) after intensive therapy is usually most relevant in older patients (commonly above the age of 65 years), age is merely one, and not the most important, predictor of TRM.130-135 Furthermore, TRM rates are declining due to improved supportive care and to better health status in older patients.136,137
Therefore, age alone should not be the decisive determinant to guide therapy. Although few randomized trials have addressed the question and these trials have been small, there are suggestions that older, medically fit patients may benefit more from “intensive” than “nonintensive” induction therapy, subject to the constraints of selection bias.137 Hence, although recognizing that firm criteria to consider older patients (or any patients) unfit for intensive induction therapy cannot be provided, the panel feels these should include only factors such as poor performance status and significant comorbidities and, in the case of conventional regimens such as 7+3, adverse ELN cytogenetics/molecular genetics (Table 5) because in these instances the benefit may not outweigh the risk. Results from cytogenetics should be obtained preferably within 5 to 7 days. Results from NPM1 and FLT3 mutational screening should be available within 48 to 72 hours (at least in patients eligible for intensive chemotherapy), and results from additional molecular genetics within the first treatment cycle. Abnormal renal or liver function should not be considered solely but in the context of other comorbidities and, although dose reduction may be called for, should not per se exclude patients from administration of intensive therapy. Several systems to quantify comorbidities and/or risk of TRM after intensive induction therapy have been proposed (see “Older patients not considered candidates for intensive chemotherapy”).
Intensive induction therapy
Anthracycline dose level.
Randomized studies have indicated that daunorubicin at 45 mg/m2 daily ×3 is associated with a lower CR rate and a higher relapse rate than 90 mg/m2 daily ×3 when daunorubicin is used in a single induction cycle.139-141 This clear dose-effect relation seems much less prominent in patients >65 years of age. However, another comparison found that 90 mg/m2 daunorubicin daily ×3 in a first induction cycle was not superior to daunorubicin at 60 mg/m2 daily ×3.142 In this study, both groups received additional daunorubicin at 50 mg/m2 for 3 days once in CR which added significant toxicities to the high-dose schedule and may have obscured or counteracted the benefit of the 90 mg/m2 during the first cycle. A recent exploratory analysis from this study suggests the potential for improved outcomes among patients with FLT3-ITD with anthracycline intensification, although this finding requires further validation.143 Current evidence suggests that the dose of daunorubicin should not be <60 mg/m2.
In patients 50 to 70 years of age, daunorubicin (80 mg/m2 for 3 days) or idarubicin (12 mg/m2 for 4 days) were compared with the usual idarubicin schedule (12 mg/m2 for 3 days). Although the CR rate was slightly higher with 4 days of idarubicin, there were no differences between the 3 arms in rates of relapse, EFS, or OS.144
Cytarabine dose.
Recent studies123,145 confirm earlier ones demonstrating increased toxicity without improvement in efficacy with higher dose cytarabine (2000-3000 mg/m2). A randomized trial found that fludarabine + high-dose cytarabine + granulocyte colony-stimulating factor (G-CSF; FLAG) + idarubicin (FLAG-IDA) not only produced a lower relapse rate than daunorubicin-cytarabine with or without etoposide, but was also associated with more deaths in remission resulting in similar OS.123 Only 1 randomized study has shown prolonged OS (52% vs 43% at 6 years) with cytarabine at 3000 mg/m2 (every 12 hours, days 1, 3, 5, 7) compared with 100 mg/m2 (daily ×7) in cycle I, but only in patients <46 and not 46 to 60 years of age.146 The bulk of evidence indicates that cytarabine at doses >1000 mg/m2 should not be included in induction regimens.147 Furthermore, neither this study nor any others have shown that particular cytogenetic subsets benefit from such high cytarabine doses (see also “Conventional postremission therapy”).
Role of other drugs.
FLT3 inhibitors.
The RATIFY trial evaluated intensive induction and consolidation chemotherapy plus midostaurin or placebo followed by a 1-year midostaurin/placebo maintenance phase in 717 patients aged 18 to 60 years with FLT3-mutated AML.61 Use of midostaurin increased the CR rate when all CRs reported within 30 days of ending protocol therapy were considered (68% vs 59%; P = .04). The trial met its primary end point in improving OS (hazard ratio 0.78; P = .009), regardless of whether patients received allogeneic HCT. Thus, patients with FLT3-mutated AML may be considered to receive intensive chemotherapy in combination with midostaurin.
Gemtuzumab ozogamicin.
The role of gemtuzumab ozogamicin (GO), an antibody-toxin (calicheamicin) conjugate that targets CD33+ AML, is complicated. Two randomized studies using a single GO dose during chemotherapy in patients primarily age <60 years failed to show a survival advantage,148,149 although the first used a suboptimal daunorubicin dose (45 mg/m2) in the GO arm vs 60 mg/m2 in the control arm.148 Both studies suggested the addition of GO was associated with longer relapse-free survival (RFS) in the favorable-risk subset of CBF-AML. The second study149 extended this finding to survival in some patients with intermediate-risk cytogenetics. Two studies in older patients (median age, 61 and 67 years), 1 using a single 3 mg/m2 GO dose and the other using 3 mg/m2 GO on days 1, 4, and 7 of induction found survival benefit with GO, largely attributable to fewer relapses in patients with favorable- or intermediate-risk cytogenetics.150,151 An individual patient data meta-analysis of these 4 studies and a fifth published in abstract form reinforced these conclusions.152 In contrast, 1 large study in patients age 61 to 75 years found shorter survival (P = .071) in the GO arm largely reflecting higher early mortality in patients age 70 to 75 years.153 The dose and schedule of GO may be critical for the benefit-toxicity ratio. GO is currently only available in clinical trials and through a compassionate use program sponsored by the US Food and Drug Administration (FDA).
CPX-351.
CPX-351 is an encapsulation in nanoscale liposomes of cytarabine and daunorubicin at a synergistic 5:1 molar ratio.154-157 Phase 2 studies suggested a beneficial effect of the agent in first-line treatment of secondary and therapy-related AML,155 and in the poor-risk stratum (by the European Prognostic Index [EPI])158 of relapsed AML.156 A subsequent phase 3 trial randomized 309 patients age 60 to 75 years with high-risk AML, defined as AML with myelodysplasia-related changes or therapy-related AML, to CPX-351 or “7+3”.157 CPX-351 produced a higher response rate (CR/CRi, 47.7% vs 33.3%; P = .016), and longer OS (hazard ratio, 0.69; P = .005 with medians of 9.6 vs 6 months and 2-year survival rates of 31% and 12%). Results were similar after accounting for allogeneic HCT. Thus, CPX-351 may improve therapy of older patients with high-risk features.
Purine analogs.
In 1 study, cladribine (at 5 mg/m2 days 1-5) added to “7+3” in adults up to age 60 years produced a higher CR rate and better OS than 7+3, particularly in patients age 50 to 60 years and in those with adverse-risk cytogenetics.159 However, the relatively low CR rate (56%) and median OS (14 months) in the control arm have raised questions, and we await independent confirmation. In the intensive arm of their AML16 trial in older patients (median age, 67 years), the National Cancer Research Institute (NCRI) Cooperative Group randomized 806 patients between daunorubicin (50 mg/m2 days 1-3) and either cytarabine (100 mg/m2 days 1-10) or clofarabine (20 mg/m2 days 1-5). Rates of CR (66%-71%), relapse (68%-74% at 3 years) and OS (22%-23% at 3 years) were essentially identical.160
Intensive postremission therapy
Conventional postremission therapy.
Postremission strategies comprise intensive chemotherapy and high-dose therapy followed by autologous or allogeneic HCT (Table 8). Assessment of residual disease by RT-qPCR or MFC is critical in monitoring patients in morphological remission to inform further therapy (see “Factors after diagnosis”).
Conventional intensive consolidation.
Consolidation regimens include single-agent cytarabine at high doses and multiagent chemotherapy which lead to similar outcomes. Administration of up to 4 cycles of high-dose cytarabine (2000-3000 mg/m2, commonly 6 doses per cycle) has been widely used. Recent trials have questioned the need for such high doses. One study randomized 933 patients, 15 to 60 years of age, between consolidation with mitoxantrone and cytarabine at 3000 mg/m2 (every 12 hours for 6 days) vs a similar chemotherapy program, but with intermediate-dose cytarabine (IDAC) at 1000 mg/m2 for consolidation with no differences in outcome.161 Similarly, in a study with multiple randomizations in induction, the postremission comparison between cytarabine 3000 mg/m2 and 1500 mg/m2 (n = 657) showed no difference in survival.123 A third study in 781 complete responders (15-64 years of age) failed to show a benefit for 3 cycles of cytarabine at 2000 mg/m2 (every 12 hours for 5 days) compared with 4 cycles of a multiagent chemotherapy consolidation that contained 200 mg/m2 cytarabine by 24-hour continuous infusion for 5 days.162 None of these studies have identified a benefit of the high-dose cytarabine regimens in cytogenetically favorable-risk AML. In a smaller study in patients 15 to 50 years of age, no difference in survival was noted between 4 cycles of cytarabine at 3000 mg/m2 and a combination of multiple cytotoxic agents.163
Altogether, there is no convincing evidence that cytarabine regimens at 3000 mg/m2 are more effective than regimens at intermediate-dose levels at 1000 to 1500 mg/m2, with or without the addition of an anthracycline.147 Open questions remain regarding the optimal number of cycles of consolidation therapy. In most studies, 2 to 4 cycles have been given after attainment of CR. In 1 randomized study, 2 cycles of postremission treatment following 2 induction cycles was not inferior to 3 postremission cycles.123 Intensified postremission chemotherapy in high-risk patients, especially older patients is without clear benefit.164
Intensive chemotherapy followed by autologous HCT.
One cycle of intensive chemotherapy followed by autologous HCT using peripheral blood CD34+ cells offers condensed treatment. In 1 randomized study, autologous HCT provided better RFS and similar OS as conventional consolidation chemotherapy.165 Recent data addressing the value of autologous HCT come from retrospective analyses accounting for the “lead time bias” consequent to the need for transplanted patients to live a minimum amount of time in order to receive a transplant. In these studies, autologous HCT leads to better EFS and RFS than chemotherapy.16,166,167 This effect is mainly apparent in favorable- and intermediate-risk disease (mainly by 2010 ELN criteria) where outcome after autologous HCT approaches results after allogeneic HCT if OS is the end point. Limiting autologous HCT to patients who are MRD− might improve results.
Maintenance therapy.
Allogeneic HCT.
AML is the most frequent indication for allogeneic HCT with a 10% annual increase in transplants performed worldwide.170-172 Expanded use of mismatched and unrelated donors as well as cord blood means a donor can be found for most patients. Furthermore, nonmyeloablative or reduced-intensity conditioning (RIC) regimens allow allogeneic HCT in patients aged up to 75 years. Nonetheless, in reality, only a minority of AML patients undergo transplantation because of older age, comorbidities, toxicity of prior therapy, inability to achieve a remission, and early relapse or refractory leukemia.173
Indications.
The decision to perform allogeneic HCT depends on the assessment of the risk-benefit ratio (ie, nonrelapse mortality [NRM]/morbidity vs reduction of relapse risk) based on cytogenetic and molecular genetic features as well as patient, donor, and transplant factors.174-177 AML with favorable-risk genetics are not a priori assigned to allogeneic HCT in first CR.57-59,77,174,177 Allogeneic HCT is generally recommended when the relapse incidence without the procedure is expected to be >35% to 40%. The higher the expected relapse risk, the more risk of NRM may be accepted. Especially in the adverse genetic group, it is generally assumed, although not unambiguously demonstrated, that the transplant should be performed as soon as CR has been achieved. Allogeneic HCT is the only curative option for patients with primary refractory disease.
Sequential MRD monitoring by RT-qPCR or MFC provides a reliable guide to management. Patients with persistent MRD or with early MRD reoccurrence can receive salvage therapy and proceed to transplant before hematologic relapse, or may proceed directly to transplant depending on the likelihood of success with salvage therapy. Although allogeneic HCT often produces superior outcomes to chemotherapy it does not abrogate the negative effect of unfavorable genetics or pretransplant MRD.99,119 Patients without MRD or adverse genetics but with high risk of NRM could receive chemotherapy only or autologous transplantation in CR1.167,178
Myeloablative conditioning vs RIC.
RIC potentially extends the curative graft-versus-leukemia effect to patients of older age or to young patients with significant comorbidities.179-182 Conditioning intensity varies. For instance, busulfan/fludarabine is more dose-intense than fludarabine/low-dose total-body irradiation.183 Currently, >30% of allogeneic transplants are performed using RIC and have yielded encouraging results.184 Although RIC and ablative conditioning have produced similar survival in patients aged 40 to 60 years in first CR,167 a trial of the Blood and Marrow Transplant Clinical Trials Network (BMT CTN 0901) randomizing 218 patients (+54 with MDS) aged 18 to 65 years and with HCT comorbidity index (HCT-CI) scores associated with <20% to 30% NRM between RIC (typically fludarabine/busulfan) and more ablative (typically busulfan/cyclophosphamide) regimens suggests an advantage for more ablative regimens.185 This emphasizes the importance of randomized trials in transplantion with broad eligibility criteria to avoid selection bias. Currently, myeloablative regimens are generally recommended for healthy younger patients and RIC in elderly patients or in younger patients with severe comorbidities. Outcomes after myeloablative conditioning using busulfan/cyclophosphamide appear to be equivalent, if not superior, to outcomes after cyclophosphamide/total-body irradiation.186-188
Comorbidities and risk scores.
Several transplant-related models have been developed to optimize decision-making about suitable candidates for allogeneic HCT.189 The HCT-CI is a validated tool that sums a patient’s comorbidities into a single score that predicts the likelihood of NRM given a myeloablative or RIC regimen.190 A Disease Risk Index based on disease stage and cytogenetics has been developed that predicts the likelihood of disease recurrence following myeloablative or RIC regimens, independent of age, conditioning intensity, graft source, and donor type.191 The modified European Society for Blood and Marrow Transplantation (EBMT) risk score was designed to predict OS rather than just NRM or relapse, and includes age, disease stage, donor source, gender mismatch, and time from diagnosis.192 Recent reports suggest that a combination of the HCT-CI and the EBMT score may provide improved prediction of NRM and OS.193,194
New modalities.
Partial or complete T-cell depletion and posttransplant cyclophosphamide may reduce the risks of acute and chronic graft-versus-host disease (GVHD).195-198 The biggest challenge remains prevention of posttransplant relapse.199 Preparative regimens including novel agents or radiolabeled monoclonal antibodies,200 or therapy during the early posttransplant period with tyrosine kinase inhibitors or hypomethylating agents (HMAs) are being tested.201-203 Furthermore, cell-based therapies are being developed to enhance the graft-versus-leukemia effect, such as natural killer cell enrichment or adoptive transfer, and the use of genetically engineered antigen-specific T cells that target AML-specific antigens.204-209
Older patients not considered candidates for intensive chemotherapy
Some AML patients will not tolerate intensive chemotherapy. Several risk scoring systems are available that use patient-specific and disease-specific factors to make the choice of intensive or alternative treatment.74,132,133,210 The relevance of systems193,194 originally designed to forecast NRM after allogeneic HCT is under investigation.211
Treatment alternatives for unfit patients are limited to best supportive care, low-intensity treatment, or clinical trials with investigational drugs. Low-intensity options are either low-dose cytarabine (LDAC) or therapy with HMA (Table 8). LDAC is generally well-tolerated and produces CR rates in the order of 15% to 25%; however, OS (median, 5-6 months) is unsatisfactory.212
Therapy with HMA has been evaluated in randomized trials. An increase in median OS with decitabine vs mostly LDAC (7.7 vs 5.0 months) was observed.213 The AZA-AML-001 trial compared azacitidine with 3 conventional care regimens in patients aged ≥65 years with >30% blasts: LDAC (158 patients), 7+3 (44 patients), or best supportive care only (45 patients)214 ; azacitidine increased the median survival (10.4 vs 6.5 months). Azacitidine may be particularly advantageous in AML with adverse cytogenetics.215 Superiority of azacitidine over conventional care regimens was previously shown in AML with 20% to 30% blasts.216 Up to 6 courses may be needed to observe maximal response with azacitidine or decitabine, although patients without response after 3 courses are unlikely to respond with further therapy.217 HMA seem to alter the natural course of AML in some patients who do not achieve CR. Thus, hematologic improvement can also yield clinical benefit, that is, a reduction in transfusions and improved quality of life (QoL).
Treatment of unfit and most older patients with AML is currently unsatisfactory. We strongly recommend enrolling these patients in clinical trials.
Relapsed disease and primary refractory disease
Treatment of patients with relapsed or primary refractory disease requires a balanced assessment of the likely benefit of further therapy vs the potential complications associated with salvage chemotherapy.218
Prognostic markers
Factors influencing survival were incorporated in the EPI score applicable to adults between 15 and 60 years of age.158 Poor outcome is associated with shorter CR1 duration, increasing age at the time of relapse, nonfavorable karyotype at initial diagnosis, or history of prior allogeneic HCT.
Salvage treatment
No specific salvage regimen has emerged as the standard for treating primary refractory or relapsed AML.122,219-226 Enrollment in a clinical trial should therefore be the priority for such patients whenever possible. Table 8 provides recommendations for salvage regimens in patients considered fit for intensive therapy.
In younger adults (16-49 years), a second CR can be achieved with intensive salvage therapy in about 55% in the absence of prior allogeneic HCT.227 Two-thirds are able to proceed to allogeneic HCT in CR2, resulting in a 40% 5-year OS. Response rates are lower (∼20%-30%) in more unselected adult patients with relapsed/refractory disease.222 Benefit may also be derived from allogeneic HCT in the presence of active disease, with CR2 achieved in 42% and long-term survival observed in 9% to 22%.228-231
Another approach for patients with refractory or active disease is to use a short course of chemotherapy such as fludarabine, cytarabine, and amsacrine immediately prior to RIC and allogeneic HCT. With this approach, CR rates after allogeneic HCT of 70% to 90% are achieved, with expected 4-year survival ranging between 32% and 45%.231,232 The possible constraint of selection bias should again be noted; nonetheless, at least 20% of patients with primary refractory disease can still be cured with allogeneic HCT.233
Outcome for patients relapsing after allogeneic HCT during first or second CR is particularly poor.234,235 The Center for International Blood and Marrow Transplant Research (CIBMTR) recently found234 3-year OS was 4%, 12%, 26%, and 38% for relapses within 1 to 6 months, 6 months to 2 years, 2 to 3 years, and ≥3 years after allogeneic HCT, respectively. Lower mortality was independently associated with longer time from HCT to relapse and a first HCT using RIC; and inferior outcome associated with age >40 years, active GVHD, adverse cytogenetics, mismatched unrelated donor, and use of cord blood for first HCT.234 Outcomes may be better if patients receive chemotherapy to reduce disease burden followed by donor lymphocyte infusion, rather than chemotherapy alone.236,237 Use of HMA has modest efficacy in AML relapsing post-HCT, producing CR rates of ∼15%238 ; responses may be higher when combining donor lymphocyte infusion and azacitidine.239 Responses have been observed in relapses after HCT, including extramedullary manifestations, using CTLA-4 blockade with ipilimumab.240 The value of using a different donor for the second transplant remains unproven.235
In patients not fit for intensive salvage chemotherapy, effective treatment options are lacking. Azacitidine and decitabine induce CR rates of 16% to 21% and median survival times of 6 to 9 months in older patients with relapsed/refractory AML223-225 ; median postrelapse survival after therapy with LDAC is 5 to 6 months.226 For patients in second or third relapse, various therapeutic options are associated with CR rates of ∼20% and median OS outcomes of ∼3 months,221 stressing the need for enrollment into clinical trials.
Therapy-related AML
Biology of t-AML
Therapy-related myeloid neoplasms (t-MNs) are a distinct category within the WHO classification including cases of t-MDS and t-AML. t-AML is a well recognized clinical syndrome occurring as a late complication following cytotoxic therapy for a primary neoplasm or a nonneoplastic disorder.241,242 Currently comprising ∼7% of all newly diagnosed AML, the incidence of t-AML is rising due to increasing numbers of cancer survivors at risk and changes in treatment.125,243,244
These neoplasms have been thought to be the direct consequence of mutational events induced by cytotoxic therapy. Association between type of prior exposure and phenotype of t-AML support a direct role of prior cytotoxic therapy. The more common subtype, seen in ∼75% of patients, typically occurs 5 to 7 years after first exposure to alkylating agents or radiation, is often preceded by MDS, and is frequently accompanied by chromosomes 5 and/or 7 abnormalities, complex karyotype, and TP53 mutation. In general, t-AML is associated with more adverse genetic lesions.245-248 In a study analyzing mutation hotspots of 53 genes in 70 t-MNs (28 t-MDS, 42 t-AML), TP53 was the most commonly mutated gene in t-MDS (35.7%) and t-AML (33.3%).248 Some individuals develop t-AML after treatment with topoisomerase II inhibitors; their latency period is often only 1 to 3 years, antecedent MDS is rare, and balanced rearrangements involving KMT2A (MLL) at 11q23, RUNX1 at 21q22, or PML/RARA are common. The distinction between these 2 subtypes has become less evident due to the use of multiagent chemotherapy, often in combination with radiotherapy.
An alternative mechanism is suggested by cases with a preexisting myeloid clone that is resistant to chemotherapy.249 Cases of t-AML were identified in which the exact TP53 mutation found at diagnosis was already present at low frequency in blood or bone marrow many years before t-AML development.249 Similarly, somatic mutations in PPM1D, a serine/threonine phosphatase that negatively regulates p53,250 have been found in blood of patients with breast, ovarian, and lung cancer.251-254 In ovarian cancer, the frequency of PPM1D mutations in blood was significantly associated with prior chemotherapy, and the variant allele frequency increased during chemotherapy.251 These data suggest a model in which hematopoietic progenitor cells carrying mutations in the TP53 pathway undergo selective pressure by cytotoxic therapy, ultimately leading to t-AML.
Some cases of t-MNs have been shown to be associated with germ line mutations in cancer susceptibility genes.255,256 In a recent study of survivors of breast cancer developing t-AML, many patients had personal or family histories suggestive of inherited cancer susceptibility; 10 of 41 patients studied (21%) carried germ line mutations in BRCA1, BRCA2, TP53, or CHEK2 genes.256 The identification of such preexisting conditions will facilitate screening and counseling of patients prior to treatment of their primary disease.
Treatment of t-AML
The survival of patients with t-MNs has remained poor mainly due to sequelae of prior therapy, and to adverse disease-related features.257-261 Therapy may be compromised by a higher treatment-related morbidity and mortality.259 There is still little prospective treatment data because these patients have often been excluded from frontline clinical trials. Clinical trials should allow enrollment of patients with t-MN. Allogeneic HCT should be considered, due to the poor results with conventional chemotherapy.
Clinical trials
Necessity for biobanking
We strongly recommend storage of biosamples (see “Biobanking”) be done in all clinical trials. Such biobanking can be performed as part of an interventional trial, or within a noninterventional biobanking or registry study.
Trial design
Trials of new therapies have traditionally been disease-specific, proceeding through phase 1 (determination of maximum tolerated dose [MTD]), phase 2 (determination of efficacy), and phase 3 (randomized comparison of new and standard therapies). Recent challenges to this paradigm have arisen.
Early drug development.
“Basket trials.”
MTD vs “optimal biologic dose.”
When a drug’s ability to modulate its target appears fundamental to its clinical activity, phase 1 studies might seek to identify the optimal biologic dose (OBD) rather than the MTD. Randomization between OBD and MTD might be considered in phase 2 to shed light on which approach is preferable.262
Combined phase 1-2 designs.
To accelerate drug development, many phase 1 protocols now include an expansion phase which focuses on efficacy.264 On the assumption of a relation between efficacy and toxicity, multiple outcome designs simultaneously base dose finding on toxicity and efficacy, with a dose declared admissible for further study if associated with relatively low probabilities of toxicity and high probabilities of efficacy.265
“Pick-a-winner designs” to accelerate drug development.
The conventional distinction between the single-arm phase 2 trial and the larger (randomized) phase 3 study has been questioned. The frequent failure of therapies found “promising” in single-arm phase 2 trials to translate into truly successful treatments because of various biases in phase 2 is well known.266 Because these biases can only be addressed by randomization, there has been increasing interest in randomized phase 2 designs, also known as “selection” or “pick-a-winner” designs.267,268 Here, randomization between a standard and a new treatment begins sooner than currently. A first stage enrolls a relatively small number of patients, thus allowing more agents to be investigated in a given time. Treatments that meet a particular efficacy criterion are carried forward against the standard into a larger second stage, analogous to standard phase 3 studies, whereas treatments not meeting these criteria drop out. One limitation of the design is that small sample sizes may preclude the identification of patients with biologically defined subsets of the disease that may benefit from a particular new agent.
Adaptive designs.
Adaptive designs use incoming information from the early stages of a trial to affect conduct of later stages.269,270 Although designs such as the 3+3 and the Simon 2-stage are technically “adaptive,” newer designs make more frequent use of incoming information. An example is “adaptive randomization” in which patients are initially randomized 1:1 after which randomization probabilities change at various intervals, to reflect incoming results.269 An advantage is that fewer patients may receive an ultimately unsatisfactory therapy, whereas a disadvantage is a loss of power. Another example is the continuous reassessment method, which in phase 1 trials permits more account to be made of covariates other than dose than does the standard 3+3 design.271
End points
OS and EFS.
Table 7 lists outcome measures, and Table 9 recommended reporting criteria for phase 3 clinical trials. OS is the end point most commonly used for approval of new therapies. However, OS may be an imperfect indicator of a new drug’s efficacy because advances in rescue therapies and supportive care have made it possible to keep patients alive after AML has relapsed or failed to enter CR.262,272 In contrast, EFS includes relapse and failure to enter CR as well as death and thus may better reflect a single treatment’s efficacy.272-275 Furthermore, less time is required to assess EFS, and use of EFS facilitates crossover designs, that is, patients are randomly assigned to a sequence of treatments.
Incorporation of MRD.
The utility of CR as a surrogate for OS has been questioned.276,277 Likewise, if CRs are short-lived, a higher CR rate may not result in meaningful improvements in EFS. Considerable evidence indicates that patients in CR by conventional criteria who have MRD as assessed by RT-qPCR or MFC are at higher risk of relapse and death than patients without MRD (see “Monitoring of minimal residual disease”). This suggests the potential utility of CRMRD− as a rapidly assessable end point that may serve as a surrogate for EFS or long-term survival provided these relationships can be confirmed and means to measure MRD can be harmonized.91,92
QoL.
Regulatory drug approval agencies accept improvement in QoL as well as in quantity of life as a criterion for new drug approval. Although QoL has received little attention, clinical observation suggests that patients who achieve CR may have improved QoL, for example, due to receipt of fewer transfusions and spending less time in medical facilities than patients who do not achieve CR, even if survival is not improved; the same may apply with CRi.278
Novel therapies
AML is an important field for new drug investigation.2,262,279 Novel therapies are usually first evaluated in patients with relapsed/refractory disease or in older patients not considered candidates for standard intensive chemotherapy. Novel therapies in preclinical or clinical development may be categorized as protein kinase inhibitors, epigenetic modulators, new cytotoxic agents, mitochondrial inhibitors including apoptosis therapies, therapies targeting specific oncogenic proteins, therapeutic and immune checkpoint antibodies and cellular immunotherapies, and therapies targeting the AML microenvironment (Table 10).
Efforts to develop protein kinase inhibitors, inhibiting mutated forms of the FLT3 receptor have led to successive generations of FLT3 inhibitors.280 The first generation comprised tandutinib, sunitinib, lestaurtinib, sorafenib, and midostaurin, and the next generation quizartinib, crenolanib, and gilteritinib. These compounds differ not only in their ability to inhibit FLT3-ITD or tyrosine kinase domain or even the wild-type receptor, but also in their selectivity for FLT3 as well as their toxicity profiles. As discussed in “Intensive induction therapy,” the phase 3 trial evaluating midostaurin in younger adult patients with FLT3 mutations reached its primary end point, improvement of OS.61 Randomized trials evaluating intensive chemotherapy with other FLT3 inhibitors, such as lestaurtinib and sorafenib, failed to show an improvement in response rate and in OS.281-284 The trial with sorafenib in younger patients (not restricted to AML with FLT3 mutations) showed an improvement in EFS, mainly reflecting results in patients without FLT3-ITD, that did not translate into a significant OS benefit.284 Randomized trials evaluating next-generation FLT3 inhibitors are ongoing.
Another rapidly expanding area is development of novel epigenetic therapies.285,286 Guadecitabine (SGI-110) is a second-generation HMA currently in phase 3 development.287 Guadecitabine is a dinucleotide of decitabine and deoxyguanosine that increases the in vivo exposure of decitabine by protecting it from inactivation by cytidine deaminase. One novel targeted approach is the inhibition of the metabolic enzymes IDH1 and IDH2 that are frequently mutated in AML.288 Early trial results with these inhibitors show durable responses and appear promising.289,290 Other examples are targeting of BRD4, a member of the BET family of bromodomain epigenetic readers,291 or of KMT2A (MLL)–rearranged leukemias.292,293
In a randomized trial conducted in patients with relapsed and refractory AML, the topoisomerase II inhibitor vosaroxin in combination with IDAC demonstrated a small survival benefit in patients older than 60 years (7.1 vs 5.0 months); a benefit was not shown in younger patients, potentially due to the higher transplant rate (45.8% <60 years vs 20.2% ≥60 years).222
Finally, targeted immunotherapy is an important novel approach.294 A variety of therapeutic antibodies directed against AML antigenic targets (eg, CD33, CD123, CLEC12A), bispecific T-cell engagers, or dual-affinity retargeting molecules as well as engineered chimeric antigen receptor T cells targeting the CD33 and CD123 antigens are currently in early clinical trial.
Management of special situations
Hyperleukocytosis
A recent systematic review assessed early mortality in patients with an initial white blood cell count ≥100 × 109/L and found neither leukapheresis nor hydroxyurea/low-dose chemotherapy influenced the early death rate.295 Hyperleukocytosis reflects a medical emergency. After immediate diagnostic testing, patients should begin cytoreductive treatment without delay preferably with the planned induction regimen.
Others
There have been no new developments in management of central nervous system (CNS) AML, myeloid sarcoma, or pregnancy in AML since the 2010 ELN publication and readers are referred there for information.1
Supportive care
Prophylactic anti-infectious treatment
For prophylaxis and treatment of infections, prevailing institutional infectious organisms and their drug-resistance pattern should primarily be considered. As noted in the 2010 ELN recommendations, prophylaxis with a quinolone should be given.1
A systematic survey of randomized trials in AML found “high-level evidence” supporting use of posaconazole to prevent invasive fungal infections during remission induction therapy and in patients with GVHD after allogeneic HCT. Micafungin can be used when azoles are strictly prohibited, although fluconazole is generally acceptable because it has a very low interaction with CYP3A4. There was insufficient evidence to guide antifungal prophylaxis in patients undergoing allogeneic HCT without GVHD or other high-risk factors.296
Other issues
There have been few new developments regarding use of myeloid growth factors or transfusion support since the 2010 ELN recommendations to which the reader is referred.1 Neither growth factors nor granulocyte transfusions can be recommended outside of the individual patient setting. In 2 randomized trials comparing prophylactic (at a count <10 × 109/L) vs therapeutic (only if bleeding) platelet transfusion, more grade 2-4 bleeding occurred in the therapeutic arms together with a slight excess in fatal (CNS) hemorrhage.297,298 Thus, prophylactic platelet transfusion at a count <10 × 109/L remains the standard for patients with AML.
Acknowledgments
The authors gratefully acknowledge Rüdiger Hehlmann for his continuous generous support of these recommendations on behalf of the European LeukemiaNet; Adam Ivey and Elli Papaemmanuil for their support in generating Figure 1; and Lucy Godley and Rafael Bejar for reviewing the section on myeloid neoplasms with germ line predisposition.
H. Döhner was supported by SFB 1074 “Experimental models and clinical translation in leukemia” funded by the Deutsche Forschungsgemeinschaft (DFG). D.G. was grateful for support from the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research Programme (grant reference RP-PG-0108-10093). J.S. was supported by grants from the Agència de Gestió d'Ajuts Universitaris i de Recerca (AGAUR) 2014SGR-1281, Instituto de Salud Carlos III (ISCIII) RD12/0036/0071 and Fondo de Investigación en Salud (FIS) PI14/00450. F.L.-C. was supported by Associazione Italiana per la Ricerca sul Cancro grant AIRC I.G. 5916. C.D.B. was supported by National Institutes of Health National Cancer Institute grants CA180861, CA016058.
Authorship
Contribution: All authors reviewed the literature and wrote first drafts of specific sections; H. Döhner and C.D.B. assembled the sections and wrote the final version of the manuscript; and all authors reviewed and approved the final version of the manuscript.
Conflict-of-interest disclosure: H. Döhner provided consultancy services to Agios, Amgen, Astex Pharmaceuticals, Celator, Celgene, Novartis, Roche, Seattle Genetics, Sunesis, and Tolero, and received research funding from Boehringer Ingelheim, Celgene, Novartis, Bristol-Myers Squibb, and Arog Pharmaceuticals. S.A. provided consultancy services to Amgen and Daiichi Sankyo. H. Dombret provided consultancy services to Roche/Genentech, Amgen, Pfizer, Novartis, Celgene, Jazz Pharmaceuticals, Agios, Sunesis, Ambit, Daiichi Sankyo, Karyopharm, Kite Pharma, Menarini, Astellas, Janssen, Servier, and Seattle Genetics, and received research funding from Roche/Genentech, Amgen, Ariad, Jazz Pharmaceuticals, and Kite Pharma. B.L.E. provided consultancy services to Celgene, Genoptix, and H3 Biomedicine, and received research funding from Celgene. P.F. provided consultancy services to Celgene, Novartis, and Teva, and received research funding from Celgene, Janssen, Novartis, Astex, and Teva. R.A.L. provided consultancy services to Novartis, Ariad, CVS/Caremark, Erytech, Pfizer, Celgene, and Bristol-Myers Squibb, and received research funding from Astellas, Erytech, Novartis, and Daiichi Sankyo. R.L.L. provided consultancy services to Novartis and served on the supervisory board for Qiagen. F.L.-C. provided consultancy services to Teva and Novartis, received honoraria from Teva and Lundbeck, and received research support from Teva and Novartis. D.N. received research funding from Novartis and Amgen, and served on the speakers’ bureaus for Novartis and Amgen. G.J.O. provided consultancy services to Novartis, Pfizer, Bristol-Myers Squibb, Johnson & Johnson, Sunesis, Celgene, Karypharm, and Amgen, and received research support from Novartis, Johnson & Johnson, Celgene, Immunogene, and Becton Dickinson. J.S. provided consultancy services to Celgene, Novartis, Sunesis, Karyopharm, Pfizer, Janssen, and Meda Pharmaceuticals; received research support from Celgene, Novartis, and Amgen; was a speaker for Celgene, Pfizer, and Janssen; and was a member of the Board of Directors for the European Haematology Association, the Spanish Society of Hematology, and the José Carreras International Leukemia Foundation. A.H.W. provided consultancy services to Novartis, Celgene, Servier, Abbvie, Roche, Amgen, and CTI, and received research funding from Abbvie, Novartis, Celgene, Servier, Ariad, and Amgen. B.L. provided consultancy services to Celgene, Agios, AstraZeneca, and Astex, and was a Section Editor for Leukemia. The remaining authors declare no competing financial interests.
Thomas Büchner died on 5 August 2016. David Grimwade died on 17 October 2016.
Correspondence: Hartmut Döhner, Department of Internal Medicine III, University of Ulm, Albert-Einstein-Allee 23, 89081, Ulm, Germany; e-mail: hartmut.doehner@uniklinik-ulm.de.