Key Points
HDAC8 plays a key role in maintaining long-term hematopoietic repopulation.
HDAC8 modulates p53 activity to ensure LT-HSC cell survival under stress.
Abstract
The maintenance and functional integrity of long-term hematopoietic stem cells (LT-HSCs) is critical for lifelong hematopoietic regeneration. Histone deacetylases (HDACs) modulate acetylation of lysine residues, a protein modification important for regulation of numerous biological processes. Here, we show that Hdac8 is most highly expressed in the phenotypic LT-HSC population within the adult hematopoietic hierarchy. Using an Hdac8-floxed allele and a dual-fluorescence Cre reporter allele, largely normal hematopoietic differentiation capacity of Hdac8-deficient cells was observed. However, the frequency of phenotypic LT-HSC population was significantly higher shortly after Hdac8 deletion, and the expansion had shifted to the phenotypic multipotent progenitor population by 1 year. We show that Hdac8-deficient hematopoietic progenitors are compromised in colony-forming cell serial replating in vitro and long-term serial repopulating activity in vivo. Mechanistically, we demonstrate that the HDAC8 protein interacts with the p53 protein and modulates p53 activity via deacetylation. Hdac8-deficient LT-HSCs displayed hyperactivation of p53 and increased apoptosis under genotoxic and hematopoietic stress. Genetic inactivation of p53 reversed the increased apoptosis and elevated expression of proapoptotic targets Noxa and Puma seen in Hdac8-deleted LT-HSCs. Dramatically compromised hematopoietic recovery and increased lethality were seen in Hdac8-deficient mice challenged with serial 5-fluorouracil treatment. This hypersensitivity to hematopoietic ablation was completely rescued by inactivation of p53. Altogether, these results indicate that HDAC8 functions to modulate p53 activity to ensure LT-HSC maintenance and cell survival under stress.
Introduction
Long-term hematopoietic stem cells (LT-HSCs) have the unique potential of both self-renewal to maintain their pool and multilineage differentiation to produce all types of blood cells throughout life. The intricate balance between alternative cell fates, including differentiation, self-renewal, quiescence, and apoptosis, is achieved by integrating a variety of intrinsic and extrinsic regulatory mechanisms concertedly governing the HSC function.1,2 To ensure regeneration of the hematopoietic system throughout life, HSCs must also respond efficiently to hematopoietic stresses, such as blood loss, infection, or exposure to genotoxic agents.3
The tumor suppressor p53, a sequence-specific transcriptional regulator, is known to centrally coordinate cellular processes, including cell-cycle progression, cellular senescence, DNA repair, and apoptosis, in response to a wide variety of stressors. In hematopoietic cells, p53 plays important roles in proliferation, differentiation, apoptosis, and aging.4-6 It has also been shown to regulate self-renewal and quiescence of HSCs during steady-state hematopoiesis.7,8 The stability and transcriptional activity of the p53 protein are modulated through several posttranslational modifications, such as ubiquitination, phosphorylation, methylation, and acetylation.9-11 Notably, acetylation of the p53 protein is critical for its activation.12
Histone deacetylase 8 (HDAC8) is a member of the class I HDAC enzymes that remove acetyl moieties from lysine residues on histones and a variety of nonhistone proteins. HDAC8 is important for diverse biological functions, including smooth muscle contraction,13 telomere protection,14 skull morphogenesis,15 and regulation of cohesin dynamics.16 HDAC8 is highly expressed in multiple tumor types, including myeloid and lymphoid leukemia cells,17 neuroblastoma, glioma,18 and childhood acute lymphoblastic leukemia.19 We previously showed that the acute myeloid leukemia (AML)–associated inv(16) fusion protein binds both HDAC8 and p53 proteins, leading to aberrant deacetylation of p53 in inv(16)+ AML cells.20 However, the expression and function of HDAC8 in normal hematopoiesis and HSCs remain unknown.
Here, we investigate the contribution of HDAC8 to LT-HSC function and maintenance using an Hdac8-floxed allele and reporter mice. We demonstrate that HDAC8 plays a pivotal role in controlling LT-HSC maintenance and functional integrity by modulating p53 activity.
Materials and methods
Mice
Hdac8f/f(y)20 and Mx1-Cre21 mice were backcrossed to C57BL/6 for >10 generations. ROSAmT/mG mice (C57BL/6) were purchased from the Jackson Laboratory. Mice with the p53ERTAM knockin (KI)22 allele were generously donated by Gerard Evan (University of Cambridge). To induce Hdac8 deletion, 6- to 8-week-old Mx1-Cre/Hdac8f/f(y), Mx1-Cre/Hdac8f/f(y)/mTmG+, or Mx1-Cre/Hdac8f/f(y)/p53ERKI/KI mice were injected intraperitoneally with 14 mg/kg per dose of polyinosinic-polycytidylic acid (poly [I:C]; InvivoGen) every other day for 7 doses. Similarly treated littermates lacking 1 or all alleles were used as control. For in vivo bromodeoxyuridine (BrdU) labeling, mice were injected intraperitoneally with 1.5 mg of BrdU 24 hours before analysis. All mice were maintained and all procedures were performed in accordance with federal and state government guidelines and established institutional guidelines and protocols approved by the Institutional Animal Care and Use Committee at City of Hope.
Cell isolation and flow cytometry
Bone marrow (BM) mononuclear cells were collected from femurs, tibias, and pelvis as previously described.23,24 For fluorescence-activated cell-sorting analyses, cells were stained in phosphate-buffered saline with 0.5% bovine serum albumin for 15 minutes on ice with fluorescently labeled antibodies. Antibodies used included CD3, CD4, CD8, B220, CD19, immunoglobulin M, NK1.1, CD11b, CD11c, Gr1, CD41, interleukin-7 (IL-7) receptor α, cKit, Sca1, CD16/32, CD105, CD150, CD48, and Ter119 purchased from BD Biosciences, BioLegend, or eBiosciences. Flow cytometry was performed using a 5-laser, 15-detector LSRII (BD Biosciences). For cell sorting, lineage-negative cells were enriched using EasySep selection reagents (StemCell Technologies), and sorting was performed using ARIA-III (BD Biosciences). Acquired data were analyzed by Flowjo software (Tree Star). Phenotypic hematopoietic stem and progenitor cell (HSPC) populations were defined as previously described (supplemental Methods, available on the Blood Web site).23,24
Colony-forming cell assays
Myeloid/erythroid colony-forming units (CFUs; CFU-GEMMs, CFU-GMs, and BFU-Es) were enumerated using MethoCult containing stem-cell factor, IL-3, IL-6, and erythropoietin (M3434; StemCell Technologies) and pre-B CFUs were enumerated using MethoCult containing IL-7 (M3630; StemCell Technologies) according to manufacturer’s protocol. Mouse BM cells were seeded in MethoCult (1 × 104 cells per mL per dish) and were counted at day 7 according to the manufacturer’s protocol. For replating assays, cells from each plate were harvested and replated at 1 × 104 cells per mL per dish.
In vivo repopulation assays and 5-FU treatment
Mononuclear BM cells (2 × 105) were transplanted IV into lethally irradiated (11 Gy; 2 split doses) CD45.1+ 6- to 8-week-old C57BL/6 congenic mice together with 2 × 105 CD45.1+ wild-type (WT) BM supporting cells. After 4 weeks, mice were administered 7 doses (14 mg/kg per dose) of poly (I:C). Donor chimerism in peripheral blood (PB) was analyzed over time and in BM at 16 weeks. For secondary or tertiary transplantation, 2 × 106 BM cells were injected IV into lethally irradiated congenic CD45.1+ mice. For 5-fluorouracil (5-FU) ablation, 8- to 10-week-old induced mice were injected with 100 mg/kg 5-FU intraperitoneally every 7 days. Weekly differential blood count was performed using Hemavet HV950 (Drew Scientific). Mice were euthanized for phenotypic analysis at specified time points or monitored for survival.
Statistics
Statistical analyses were performed with Student t test or analysis of variance for normal distributions. Mann-Whitney U tests were used when the criteria for a normal distribution were not satisfied. P <.05 was considered statistically significant.
Results
Hdac8 contributes to HSC homeostasis and long-term colony-forming progenitor activity
As a first step to evaluate the role of HDAC8 in hematopoiesis, we assessed the expression level of Hdac8 in various hematopoietic populations in C57BL/6 mice (2-3 months old). We sorted cells of different lineages as well as phenotypic HSPC populations, including LT-HSCs (Lin−cKit+Sca1+CD48−CD150+), multipotent progenitors (MPPs; Lin−cKit+/Sca1+CD150+/−CD48+), lymphoid-primed MPPs (LMPPs; Lin−cKithiSca1+Flt3+CD48+CD150+/−), common lymphoid progenitors (CLP) (Lin−IL-7Rα+cKitloSca1lo), pregranulocyte macrophages (pre-GMs; Lin−cKit+Sca1−CD16/32−/loCD105−CD150−), granulocyte-macrophage progenitors (GMPs; Lin−cKit+Sca1−CD16/32+CD150−), premegakaryocytes/erythrocytes (pre-Meg/Es; Lin−cKit+Sca1−CD16/32−/loCD105−CD150+), and erythroid progenitors (EPs; Lin−cKit+Sca1−CD16/32−/loCD105+, including pre–CFU-E, CFU-E, and proerythrocytes [pro-Erys]) as previously defined (supplemental Methods).23,24 Highest level of Hdac8 was seen in the phenotypic LT-HSC subset followed by MPP and lymphoid-primed MPP subpopulations (Figure 1A). To further investigate Hdac8 function in hematopoiesis, we generated conditional Hdac8-deficient mice (Mx1-Cre/Hdac8f/f(y)) using Mx1-Cre and an Hdac8-floxed (Hdac8f) allele as previously described.20 Hdac8 deletion (Hdac8Δ/Δ) in adult hematopoietic cells was induced by 7 doses of poly (I:C) treatment (14 mg/kg) and confirmed by polymerase chain reaction (data not shown) and western blot analysis (Figure 1B). Similarly poly (I:C)–treated littermates (WT, Hdac8f/f(y), or Mx1-Cre) were included as controls, and no differences were observed among the 3 genotypes (supplemental Figure 1A-B). Total BM cellularity of Hdac8Δ/Δ mice was slightly reduced 6 weeks after induction compared with control mice (supplemental Figure 1C). Phenotypic analysis by flow cytometry showed largely normal frequencies and numbers of hematopoietic cells of various lineages in Hdac8Δ/Δ mice (Figure 1C; supplemental Figure 1D). Analysis of BM HSPC populations revealed no significant changes in progenitor subsets, including LSK (Lin−cKit+Sca1+) and myeloid/erythroid progenitors (pre-GMs, GMPs, pre-Meg/Es, EPs, pre–CFU-Es, CFU-Es, and pro-Erys) in Hdac8Δ/Δ mice (Figure 1E; supplemental Figure 1E). However, the frequency of phenotypic LT-HSC population was significantly higher in Hdac8Δ/Δ mice compared with similarly treated littermate control mice (Figure 1D). The estimated LT-HSC cell number was not significantly changed in Hdac8Δ/Δ mice (supplemental Figure 1F), because of the slightly reduced overall cellularity (supplemental Figure 1C).
Hdac8 contributes to HSC homeostasis and long-term CFC activity. (A) Relative expression levels of Hdac8 messenger RNA (mRNA) in sorted phenotypic HSPC and lineage populations (n = 2-7) assessed by SYBR Green–based quantitative reverse transcription polymerase chain reaction assays. Shown is the relative expression level (mean ± standard error of the mean [SEM]) for Hdac8 mRNA normalized to the Hprt mRNA expression level. (B) Schematic of experimental design (left). Mx1-Cre/Hdac8f/f(y) or controls (WT, Hdac8f/f(y), or Mx1-Cre) were injected with 7 doses (14 mg/kg) of poly (I:C) to induce the expression of Cre. Phenotypic analysis of HSPCs and CFC assays were performed 6 weeks after induction. Hdac8 protein levels in induced Mx1-Cre/Hdac8f/f(y) (Hdac8Δ/Δ) or control (Ctrl) BM cells shown by western blotting using Hdac8 specific antibody (right). (C) Frequency of various lineage populations in 2- to 3-month-old Hdac8Δ/Δ (n = 7) or Ctrl (n = 15) BM assessed by fluorescence-activated cell sorting. (D) Frequency of LT-HSC, short-term HSC (ST-HSC), and MPP subsets in Hdac8Δ/Δ (n = 10) or Ctrl (n = 13-19) BM. (E) Frequency of LSK, myeloid/erythroid progenitor populations in Hdac8Δ/Δ (n = 10) or Ctrl (n = 13-19) BM. (F) Number of CFU-Cs derived from Hdac8Δ/Δ or Ctrl BM cells (1 × 104 cells) in serial replating assays every 7 days. Shown is mean ± SEM with triplicates from 2 independent experiments. (G) The percentage of CFU-GEMM, CFU-GM, and BFUE colony types determined based on morphology. Shown is mean ± SEM with triplicates from 2 independent experiments. (H) Number of pre-B CFU-Cs derived from Hdac8Δ/Δ or Ctrl BM cells (1 × 104 cells). Shown is mean ± SEM. *P < .05, **P < .01, ***P < .001.
Hdac8 contributes to HSC homeostasis and long-term CFC activity. (A) Relative expression levels of Hdac8 messenger RNA (mRNA) in sorted phenotypic HSPC and lineage populations (n = 2-7) assessed by SYBR Green–based quantitative reverse transcription polymerase chain reaction assays. Shown is the relative expression level (mean ± standard error of the mean [SEM]) for Hdac8 mRNA normalized to the Hprt mRNA expression level. (B) Schematic of experimental design (left). Mx1-Cre/Hdac8f/f(y) or controls (WT, Hdac8f/f(y), or Mx1-Cre) were injected with 7 doses (14 mg/kg) of poly (I:C) to induce the expression of Cre. Phenotypic analysis of HSPCs and CFC assays were performed 6 weeks after induction. Hdac8 protein levels in induced Mx1-Cre/Hdac8f/f(y) (Hdac8Δ/Δ) or control (Ctrl) BM cells shown by western blotting using Hdac8 specific antibody (right). (C) Frequency of various lineage populations in 2- to 3-month-old Hdac8Δ/Δ (n = 7) or Ctrl (n = 15) BM assessed by fluorescence-activated cell sorting. (D) Frequency of LT-HSC, short-term HSC (ST-HSC), and MPP subsets in Hdac8Δ/Δ (n = 10) or Ctrl (n = 13-19) BM. (E) Frequency of LSK, myeloid/erythroid progenitor populations in Hdac8Δ/Δ (n = 10) or Ctrl (n = 13-19) BM. (F) Number of CFU-Cs derived from Hdac8Δ/Δ or Ctrl BM cells (1 × 104 cells) in serial replating assays every 7 days. Shown is mean ± SEM with triplicates from 2 independent experiments. (G) The percentage of CFU-GEMM, CFU-GM, and BFUE colony types determined based on morphology. Shown is mean ± SEM with triplicates from 2 independent experiments. (H) Number of pre-B CFU-Cs derived from Hdac8Δ/Δ or Ctrl BM cells (1 × 104 cells). Shown is mean ± SEM. *P < .05, **P < .01, ***P < .001.
We next evaluated the functional capacity of Hdac8Δ/Δ hematopoietic progenitor cells using an in vitro colony-forming cell (CFC) assay. Hdac8Δ/Δ or WT BM cells (1 × 104 cells) were seeded in semisolid methylcellulose culture media supplemented with stem-cell factor, IL-3, IL-6, and erythropoietin. Hdac8Δ/Δ progenitors generated similar numbers of total CFU-C scored at day 7 (Figure 1F plating 1). We then performed serial replating every 7 days to assess their capacity to maintain progenitor activity over time. Significantly reduced numbers of CFU-Cs were generated from Hdac8Δ/Δ progenitor cells in secondary and tertiary platings (Figure 1F). Differential counts of colony morphology revealed that Hdac8Δ/Δ cells produced an increased frequency of CFU-GEMMs and a reduced frequency of CFU-GMs compared with control cells, especially in the first plating (Figure 1G). No significant difference in pre-B lymphoid progenitor activity was seen in a CFC assay supplemented with IL-7 (Figure 1H). Collectively, Hdac8 seems largely dispensable for lineage differentiation but might contribute to LT-HSC homeostasis or output.
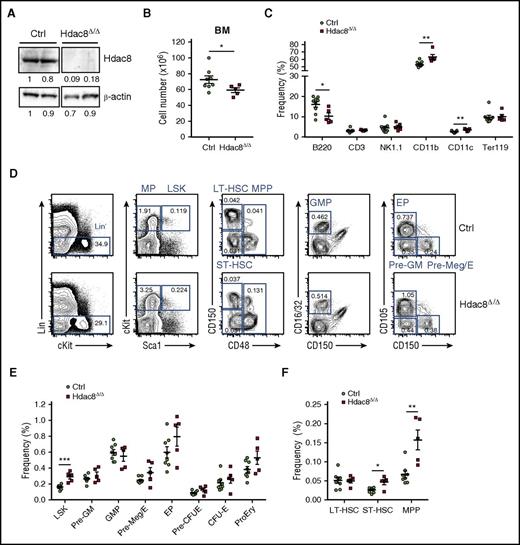
Hdac8 is essential for long-term HSC maintenance in vivo
Given that Hdac8 deletion results in compromised CFC progenitor activity over time, we reasoned that alterations of phenotypic populations by Hdac8 deletion might manifest over time in older mice. Thus, we analyzed HSPC and lineage populations in the BM 1 year after induction of Hdac8 deletion in Mx1-Cre/Hdac8f/f(y), confirmed by western blot analysis (Figure 2A; data not shown), compared with similarly treated age-matched littermate control Hdac8f/f(y) mice. We observed that BM cellularity was slightly but significantly reduced in 1-year-old Hdac8Δ/Δ mice (Figure 2B). The frequency and cell number of B cells (B220+) were significantly reduced, whereas the frequency of myeloid cells (CD11b+, CD11c+) was significantly increased, in Hdac8Δ/Δ BM (Figure 2C; supplemental Figure 2A). There was also a significant increase in the frequency and cell number of LSK population (Figure 2D-E; supplemental Figure 2B), which was predominantly due to expansion of the MPP subpopulation (Figure 2D,F; supplemental Figure 2C). In contrast to the findings in young mice, phenotypic short-term (ST)-HSCs were increased, whereas no change in phenotypic LT-HSC frequency was seen, in old mice (Figure 2F; supplemental Figure 2C). These results indicate that Hdac8 deletion perturbs homeostasis of HSPCs and hematopoietic output over time.
Hdac8 deficiency results in altered hematopoietic output over time. (A) Western blot analysis of Hdac8 and β-actin in control (Ctrl) or Mx1-Cre/Hdac8f/f(y) BM (13-15 months old) >1 year after poly (I:C) treatment. (B) Total number of BM cells harvested from Hdac8Δ/Δ (n = 5) or Ctrl (Hdac8f/f(y) ; n = 8) 1 year after poly (I:C) induction. (C) Frequency of lymphoid and myeloid lineage populations in Hdac8Δ/Δ (n = 5) or Ctrl (n = 8) BM assessed by fluorescence-activated cell sorting (FACS). (D) Representative FACS plots showing gating strategy and frequency of phenotypic populations including LSKs, LT-HSCs, ST-HSCs, MPPs, GMPs, pre-GMs, pre-Meg/Es, and EPs from Hdac8Δ/Δ or Ctrl BM. (E) Frequency of LSK, myeloid/erythroid progenitor populations in Hdac8Δ/Δ (n = 5) or Ctrl (n = 8) BM. (F) Frequency of LT-HSC, ST-HSC, and MPP subsets in Hdac8Δ/Δ (n = 5) or Ctrl (n = 8) BM. Lines indicate mean ± SEM. *P < .05, **P < .01, ***P < .001. MP, myeloid progenitor.
Hdac8 deficiency results in altered hematopoietic output over time. (A) Western blot analysis of Hdac8 and β-actin in control (Ctrl) or Mx1-Cre/Hdac8f/f(y) BM (13-15 months old) >1 year after poly (I:C) treatment. (B) Total number of BM cells harvested from Hdac8Δ/Δ (n = 5) or Ctrl (Hdac8f/f(y) ; n = 8) 1 year after poly (I:C) induction. (C) Frequency of lymphoid and myeloid lineage populations in Hdac8Δ/Δ (n = 5) or Ctrl (n = 8) BM assessed by fluorescence-activated cell sorting (FACS). (D) Representative FACS plots showing gating strategy and frequency of phenotypic populations including LSKs, LT-HSCs, ST-HSCs, MPPs, GMPs, pre-GMs, pre-Meg/Es, and EPs from Hdac8Δ/Δ or Ctrl BM. (E) Frequency of LSK, myeloid/erythroid progenitor populations in Hdac8Δ/Δ (n = 5) or Ctrl (n = 8) BM. (F) Frequency of LT-HSC, ST-HSC, and MPP subsets in Hdac8Δ/Δ (n = 5) or Ctrl (n = 8) BM. Lines indicate mean ± SEM. *P < .05, **P < .01, ***P < .001. MP, myeloid progenitor.
To further determine the functional consequences of Hdac8 deletion and track Hdac8Δ/Δ cells in vivo, we crossed Mx1-Cre/Hdac8f/f(y) mice with a dual-fluorescence Rosa26mT/mG (mT/mG) Cre reporter allele, which expresses tdTomato and becomes green fluorescent protein positive (GFP+) after Cre-mediated recombination. We performed a hematopoietic repopulation assay by transplanting BM cells (2 × 105) from Mx1-Cre/Hdac8f/f(y)/mTmG+ (CD45.2+) mice together with WT (CD45.1+) support cells (2 × 105) into lethally irradiated (11 Gy) CD45.1+ congenic recipients. Hdac8 deletion was then induced by treating the recipients with 7 doses of poly (I:C) (Figure 3A). Flow cytometry analysis of PB every 4 weeks and in BM at 16 weeks posttransplantation revealed that Hdac8 deletion did not affect overall CD45.2+ or GFP+ donor-derived repopulation or GFP+ chimerism in various lineages (B220+, CD3+, CD11b+, CD11c+, Gr1+, and Ter119+; Figure 3B; supplemental Figure 3A; data not shown). Similar frequencies of GFP+ donor-derived lineage populations were seen between Hdac8Δ/Δ and control groups (Figure 3C; supplemental Figure 3B). There was also no change in the frequency or number of GFP+ donor-derived phenotypic LT-HSCs or lymphoid/myeloid/erythroid progenitor subpopulations (CLP, pre-GMs, GMPs, pre-Meg/Es, EPs, pre–CFU-Es, CFU-Es, and pro-erys) in the BM (Figure 3D-E; supplemental Figure 3C-D). Similar compositions of phenotypic HSPCs were observed between control and Hdac8Δ/Δ GFP+ donor-derived populations (supplemental Figure 3E-F). To further assess long-term repopulating activity of Hdac8Δ/Δ HSCs, we performed serial transplantation repopulation assays. BM cells (2 × 106 cells) isolated from primary recipients 16 weeks posttransplantation were transplanted into lethally irradiated CD45.1+ congenic recipients. In secondary transplant recipients, Hdac8Δ/Δ GFP+ donor-derived multilineage repopulation was significantly compromised at multiple time points (Figure 3F). The repopulation deficiency was a result of reduction of all lineage populations (Figure 3G), suggesting that the deficiency was at the level of functional HSCs. In tertiary transplantation, little or no donor chimerism was observed in recipients of Hdac8Δ/Δ cells compared with 4 of 8 recipients showing long-term (16 weeks) repopulation of control cells (Figure 3H). To confirm that the Hdac8Δ/Δ phenotypic LT-HSCs were functionally compromised, we sorted CD45.2+ LT-HSCs from a cohort of secondary transplant recipients and transplanted 200 LT-HSCs along with WT CD45.1+ support cells (2 × 105) into lethally irradiated (11 Gy) CD45.1+ congenic recipients. Analysis of CD45.2+ donor-derived repopulation in transplant recipients showed significantly reduced Hdac8Δ/Δ LT-HSC–derived populations over time (Figure 3I). Together, these results indicate that Hdac8 is essential for maintaining long-term serial repopulating activity of HSCs over time.
Hdac8 deletion leads to loss of long-term serial repopulating activity in vivo. (A) Schematic of experimental design. Mx1-Cre/Hdac8f/f(y)/mTmG+ (Hdac8Δ/Δ) or Mx1-Cre/mTmG+ (control [Ctrl]) mouse (CD45.2+; 2-3 months old) BM cells (2 × 105) were transplanted into lethally irradiated (11 Gy) CD45.1+ congenic recipients, along with CD45.1+ supporter BM cells (2 × 105). Cre-mediated deletion of Hdac8 was induced in recipients by 7 doses of poly (I:C). Phenotypic HSPCs and GFP chimerism in the BM were analyzed 16 weeks after transplantation by flow cytometry. (B) Percentage of GFP+ donor chimerism in various lineage population at 16 weeks (n = 5-7). (C) Frequency of GFP+ donor-derived lineage populations 16 weeks after the first transplantation (n = 5-7). (D-E) The frequency of GFP+ donor-derived phenotypic HSPCs in the BM analyzed at 16 weeks (n = 5). (F) Frequency of GFP+ donor-cell repopulation over time (8-16 weeks). (G) The frequency of GFP+ donor-derived lineage populations in PB of secondary recipients (n = 3). (H) Frequency of GFP+ donor-derived cells in tertiary transplant recipients (Ctrl, n = 8; Hdac8Δ/Δ, n = 4). Dashed line indicates 1%, above which is considered positive engraftment. (I) Phenotypic CD45.2+ LT-HSCs (200 cells) sorted from secondary recipient mice were transplanted along with CD45.1+ supporter BM cells (2 × 105) into lethally irradiated (11 Gy) CD45.1+ congenic recipients. Frequency of Ctrl or Hdac8Δ/Δ CD45.2+ donor-derived populations in the transplant recipients (Ctrl, n = 8; Hdac8Δ/Δ, n = 5-6) over time. Mean ± SEM is shown. *P < .05, **P < .01, ***P < .001. IR, irradiation.
Hdac8 deletion leads to loss of long-term serial repopulating activity in vivo. (A) Schematic of experimental design. Mx1-Cre/Hdac8f/f(y)/mTmG+ (Hdac8Δ/Δ) or Mx1-Cre/mTmG+ (control [Ctrl]) mouse (CD45.2+; 2-3 months old) BM cells (2 × 105) were transplanted into lethally irradiated (11 Gy) CD45.1+ congenic recipients, along with CD45.1+ supporter BM cells (2 × 105). Cre-mediated deletion of Hdac8 was induced in recipients by 7 doses of poly (I:C). Phenotypic HSPCs and GFP chimerism in the BM were analyzed 16 weeks after transplantation by flow cytometry. (B) Percentage of GFP+ donor chimerism in various lineage population at 16 weeks (n = 5-7). (C) Frequency of GFP+ donor-derived lineage populations 16 weeks after the first transplantation (n = 5-7). (D-E) The frequency of GFP+ donor-derived phenotypic HSPCs in the BM analyzed at 16 weeks (n = 5). (F) Frequency of GFP+ donor-cell repopulation over time (8-16 weeks). (G) The frequency of GFP+ donor-derived lineage populations in PB of secondary recipients (n = 3). (H) Frequency of GFP+ donor-derived cells in tertiary transplant recipients (Ctrl, n = 8; Hdac8Δ/Δ, n = 4). Dashed line indicates 1%, above which is considered positive engraftment. (I) Phenotypic CD45.2+ LT-HSCs (200 cells) sorted from secondary recipient mice were transplanted along with CD45.1+ supporter BM cells (2 × 105) into lethally irradiated (11 Gy) CD45.1+ congenic recipients. Frequency of Ctrl or Hdac8Δ/Δ CD45.2+ donor-derived populations in the transplant recipients (Ctrl, n = 8; Hdac8Δ/Δ, n = 5-6) over time. Mean ± SEM is shown. *P < .05, **P < .01, ***P < .001. IR, irradiation.
Hyperactivation of p53 mediates increased sensitivity to hematopoietic stress in Hdac8-deficient LT-HSCs
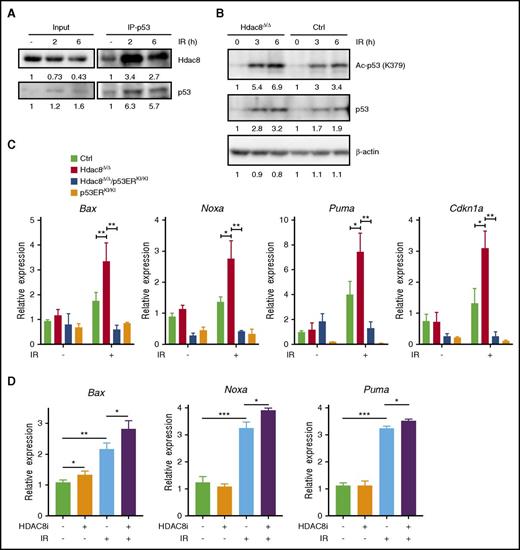
We previously showed that HDAC8 acts to inhibit p53 activity through deacetylating p53 in inv(16)+ AML cells.20 We reasoned that Hdac8 could perhaps modulate p53 activity under conditions of stress, given that acetylation is crucial for p53 activation.11,12,25 Indeed, coimmunoprecipitation assay revealed that Hdac8 binds to the p53 protein, which can be strongly enhanced upon radiation (3 Gy) exposure (Figure 4A). Analysis of BM cells after 2 to 6 hours of irradiation (3 Gy) showed elevated acetylated p53 levels (Figure 4B) and increased p53 target gene expression, including Bax, Noxa, Puma, and Cdkn1a, in Hdac8Δ/Δ mice compared with similarly treated WT control mice (Figure 4C). To confirm that these effects resulted from p53 activity, we crossed Mx1-Cre/Hdac8f/f(y) mice with the p53ERTAM KI mice carrying a p53 fusion protein completely dependent on ectopic 4-hydroytamoxifen. In homozygote p53ERKI/KI mice, p53 protein is not functional in the absence of 4-hydroytamoxifen.22 Hdac8 deletion did not cause increased radiation-induced expression of Bax, Cdkn1a, Noxa, or Puma when p53 was also deleted (Figure 4C), suggesting that these effects were indeed mediated by p53. To test whether Hdac8 modulates p53 activation via its deacetylase activity, we treated WT BM cells with HDAC8-selective inhibitor 22d26 (10 μM for 2 hours) targeting HDAC8 catalytic site before exposure to radiation (3 Gy). Treatment with the HDAC8-selective inhibitor significantly enhanced the responsiveness of p53 targets to radiation (Figure 4D), supporting that the effect on p53 was dependent on HDAC8 deacetylase activity.
Hdac8 modulates stress-induced p53 acetylation and target gene expression. (A) Coimmunoprecipitation (IP; anti-p53) and immunoblotting (anti-HDAC8 or anti-p53) analyses in 32D cells before or 2 to 6 hours after exposure to radiation (3 Gy). (B) Western blot analysis of acetylated p53, total p53, and β-actin before and after (3-6 hours) after irradiation (IR; 3 Gy) in control (Ctrl) or Hdac8Δ/Δ BM (2-3 months old) cells. (C) Relative expression of Bax, Noxa, Puma, and Cdnk1a, without IR and 6 hours after IR (3 Gy) in Ctrl, Hdac8Δ/Δ, Hdac8Δ/Δ/p53ERKI/KI, or p53ERKI/KI BM cells, measured by qRT-PCR assays. Bars represent mean ± standard deviation (n = 3-5). (D) Relative expression of p53 targets Bax, Noxa, and Puma in WT BM cells treated with HDAC8-selective inhibitor 22d (10 μM for 2 hours) or vehicle, without IR or 6 hours after IR (3 Gy). *P < .05, **P < .01, ***P < .001.
Hdac8 modulates stress-induced p53 acetylation and target gene expression. (A) Coimmunoprecipitation (IP; anti-p53) and immunoblotting (anti-HDAC8 or anti-p53) analyses in 32D cells before or 2 to 6 hours after exposure to radiation (3 Gy). (B) Western blot analysis of acetylated p53, total p53, and β-actin before and after (3-6 hours) after irradiation (IR; 3 Gy) in control (Ctrl) or Hdac8Δ/Δ BM (2-3 months old) cells. (C) Relative expression of Bax, Noxa, Puma, and Cdnk1a, without IR and 6 hours after IR (3 Gy) in Ctrl, Hdac8Δ/Δ, Hdac8Δ/Δ/p53ERKI/KI, or p53ERKI/KI BM cells, measured by qRT-PCR assays. Bars represent mean ± standard deviation (n = 3-5). (D) Relative expression of p53 targets Bax, Noxa, and Puma in WT BM cells treated with HDAC8-selective inhibitor 22d (10 μM for 2 hours) or vehicle, without IR or 6 hours after IR (3 Gy). *P < .05, **P < .01, ***P < .001.
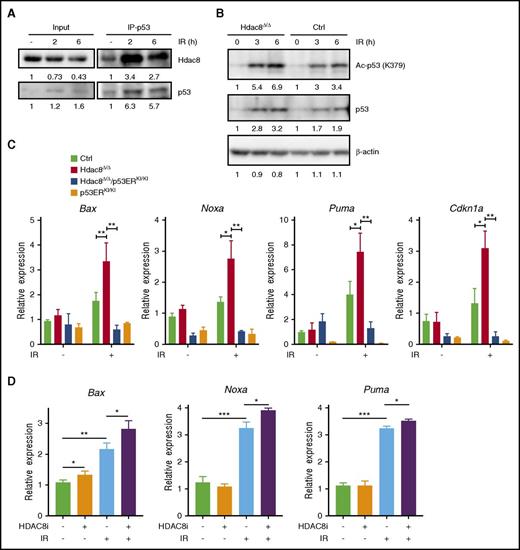
We reasoned that enhanced p53 activity could render Hdac8Δ/Δ LT-HSCs more sensitive to radiation-induced apoptosis. To test this, we induced Hdac8 deletion in Mx1-Cre/Hdac8f/f(y) or Mx1-Cre/Hdac8f/f(y)/p53ERKI/KI along with Hdac8f/f(y) control mice by poly (I:C) and sorted phenotypic LT-HSC, ST-HSC, MPP, and myeloid progenitor (MP) subpopulations; administered radiation (3 Gy); and conducted apoptosis analysis 48 hours later (Figure 5A). Annexin V and DAPI staining revealed that Hdac8Δ/Δ LT-HSCs were significantly more susceptible to apoptosis after irradiation (control, mean 21.95% with a standard error of 0.425%; Hdac8Δ/Δ, mean 30.3% with a standard error of 0.807%; P = .00006), whereas no difference was seen in spontaneous apoptosis (Figure 5B-C; supplemental Figure 4A). There were no significant changes in spontaneous or radiation-induced apoptosis in Hdac8Δ/Δ ST-HSC, MPP, or MP populations, suggesting a distinct regulatory program operative in the LT-HSC compartment (Figure 5C; supplemental Figure 4A-C). Inactivation of p53 in Hdac8Δ/Δ/p53ERKI/KI mice reversed the increased apoptosis of Hdac8Δ/Δ LT-HSCs induced by radiation (Figure 5B-C), indicating that this increased sensitivity to radiation was indeed mediated by p53. Consistent with this, Hdac8Δ/Δ LT-HSCs showed increased radiation-induced expression of apoptosis mediators Noxa and Puma, which was also reversed by p53 deletion (Figure 5D). We further examined apoptosis of HSPCs induced by whole-body irradiation (3 Gy) in vivo. Both Annexin V and DAPI staining and intracellular-activated caspase 3 staining 6 hours after irradiation showed significantly higher frequency of apoptotic cells, specifically in the LT-HSC compartment, in Hdac8Δ/Δ mice relative to controls (Figure 5E-F; supplemental Figure 4D-E). This increased radiation-induced LT-HSC apoptosis was completely rescued when 1 or both alleles of p53 were inactivated (Figure 5E-F; supplemental Figure 4D-F), confirming that this effect was mediated by p53.
Hdac8-deficient LT-HSCs are hypersensitive to p53-mediated apoptosis induced by genotoxic stress. (A) Schematic of experimental design. Hdac8f/f(y) (control [Ctrl]), Mx1-Cre/Hdac8f/f(y) (Hdac8Δ/Δ), or Mx1-Cre/Hdac8f/f(y)/p53ERKI/KI (Hdac8Δ/Δ/p53ERKI/KI) mice (2 months old) were induced by 7 doses of poly (I:C). Two weeks after induction, phenotypic LT-HSC, ST-HSC, MPP, and MP populations were sorted from BM and underwent irradiation (IR; 3 Gy). Gene expression was analyzed at 24 hours and apoptosis was assessed at 48 hours after exposure to radiation. (B) Representative FACS plots of annexin V/DAPI staining in sorted Ctrl, Hdac8Δ/Δ, or Hdac8Δ/Δ/p53ERKI/KI LT-HSCs with or without IR. (C) Frequency of annexin V+ cells in LT-HSC and MPP populations from Ctrl (n = 4), Hdac8Δ/Δ (n = 5), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) with or without IR. (D) Relative expression levels of Puma, Noxa, and Cdkn1a assessed by quantitative reverse transcription polymerase chain reaction in Ctrl (n = 4), Hdac8Δ/Δ (n = 5), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) LT-HSCs with or without IR. (E) Frequency of annexin V+ cells in the LT-HSC and MPP compartments of Ctrl (n = 6), Hdac8Δ/Δ (n = 6), Hdac8Δ/Δ/p53ERKI/+ (n = 7), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) mice 6 hours after whole-body IR (3 Gy). (F) Frequency of activated caspase 3+ cells in the LT-HSC and MPP compartment in Ctrl (n = 6), Hdac8Δ/Δ (n = 6), Hdac8Δ/Δ/p53ERKI/+ (n = 7), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) mice 6 hours after whole-body IR (3 Gy) assessed by intracellular staining followed by flow cytometry. Mean ± SEM is shown. *P < .05, **P < .01, ***P < .001.
Hdac8-deficient LT-HSCs are hypersensitive to p53-mediated apoptosis induced by genotoxic stress. (A) Schematic of experimental design. Hdac8f/f(y) (control [Ctrl]), Mx1-Cre/Hdac8f/f(y) (Hdac8Δ/Δ), or Mx1-Cre/Hdac8f/f(y)/p53ERKI/KI (Hdac8Δ/Δ/p53ERKI/KI) mice (2 months old) were induced by 7 doses of poly (I:C). Two weeks after induction, phenotypic LT-HSC, ST-HSC, MPP, and MP populations were sorted from BM and underwent irradiation (IR; 3 Gy). Gene expression was analyzed at 24 hours and apoptosis was assessed at 48 hours after exposure to radiation. (B) Representative FACS plots of annexin V/DAPI staining in sorted Ctrl, Hdac8Δ/Δ, or Hdac8Δ/Δ/p53ERKI/KI LT-HSCs with or without IR. (C) Frequency of annexin V+ cells in LT-HSC and MPP populations from Ctrl (n = 4), Hdac8Δ/Δ (n = 5), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) with or without IR. (D) Relative expression levels of Puma, Noxa, and Cdkn1a assessed by quantitative reverse transcription polymerase chain reaction in Ctrl (n = 4), Hdac8Δ/Δ (n = 5), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) LT-HSCs with or without IR. (E) Frequency of annexin V+ cells in the LT-HSC and MPP compartments of Ctrl (n = 6), Hdac8Δ/Δ (n = 6), Hdac8Δ/Δ/p53ERKI/+ (n = 7), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) mice 6 hours after whole-body IR (3 Gy). (F) Frequency of activated caspase 3+ cells in the LT-HSC and MPP compartment in Ctrl (n = 6), Hdac8Δ/Δ (n = 6), Hdac8Δ/Δ/p53ERKI/+ (n = 7), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) mice 6 hours after whole-body IR (3 Gy) assessed by intracellular staining followed by flow cytometry. Mean ± SEM is shown. *P < .05, **P < .01, ***P < .001.
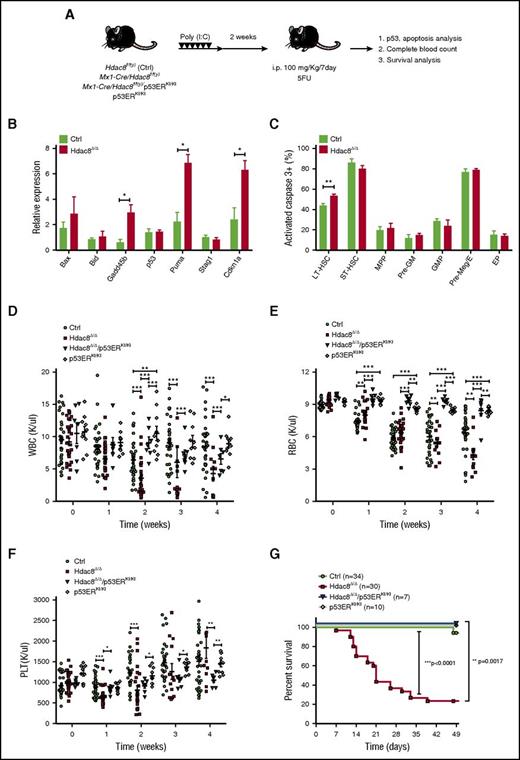
Hyperactivation of p53 could render LT-HSCs more sensitive to hematopoietic stressors, such as ablation with 5-FU, a cell cycle–dependent cytotoxic chemotherapeutic agent. We tested this by treating control or Hdac8Δ/Δ mice with serial 5-FU (100 mg/kg) weekly (Figure 6A). We confirmed that elevated acetylated p53 levels (supplemental Figure 5A-B) and increased p53 target gene expression were seen in Hdac8Δ/Δ LT-HSCs 2 days after 5-FU treatment compared with similarly treated controls (Figure 6B). Intracellular staining for activated caspase 3 revealed significantly (P = .0054) increased apoptosis in Hdac8Δ/Δ LT-HSCs (54.1% ± standard error of 1.058%) compared with control LT-HSCs (44.4% ± standard error of 1.418%; Figure 6C). After serial 5-FU (2 rounds), Hdac8Δ/Δ LT-HSC and various HSPC populations showed significantly increased apoptosis and reduced cell numbers, which could be reversed by inactivation of 1 p53 allele (supplemental Figure 5C-D). To further examine the hematopoietic consequences and functional contribution of p53, we monitored blood counts and survival of a cohort of Hdac8Δ/Δ, Hdac8Δ/Δ/p53ERKI/KI, p53ERKI/KI, or control mice treated with 5-FU weekly. Hdac8Δ/Δ mice were significantly compromised in their recovery of white blood cell, red blood cell, and platelet counts over time (Figure 6D-F). Notably, significantly increased lethality (P < .0001) was seen in Hdac8Δ/Δ mice (76% lethality; n = 30) compared with similarly treated control mice (5.9%; n = 34; Figure 6G), indicating that Hdac8 deletion indeed results in hypersensitivity to hematopoietic ablation. Loss of p53 in Hdac8Δ/Δ/p53ERKI/KI mice largely restored the hematopoietic recovery (Figure 6D-F) and completely rescued the lethality caused by Hdac8 deficiency (Figure 6G), confirming that the increased sensitivity to 5-FU ablation is indeed mediated by p53 hyperactivation. Altogether, these results indicate that Hdac8 functions to modulate p53 activity in LT-HSCs to ensure cell survival and maintenance under stress.
Hyperactivation of p53 mediates hematopoietic deficiency and increased lethality in Hdac8-deficient mice challenged with serial 5-FU. (A) Schematic of experimental design. Two-month-old mice were induced by 7 doses of poly (I:C) and complete blood count analyzed 2 weeks later (time 0), followed by 5-FU (100 mg/kg) injection every 7 days. Mice were monitored for survival or analyzed for phenotypic HSPC populations by flow cytometry. (B) Relative expression of p53 and p53 target genes Bax, Bid, Gadd45b, Puma Stag1, and Cdkn1a in control (Ctrl) or Hdac8Δ/Δ LT-HSCs 2 days after treatment with 5-FU (100 mg/kg). (C) Frequency of activated caspase 3+ cells in phenotypic HSPC subpopulations 2 days after 5-FU treatment in Ctrl or Hdac8Δ/Δ mice (n = 3). Shown is mean ± SEM. (D-F) Weekly white blood cell (WBC), red blood cell (RBC), and platelet (PLT) counts of 5-FU–treated mice (Ctrl, n = 34; Hdac8Δ/Δ, n = 30; Hdac8Δ/Δ/p53ERKI/KI, n = 7; p53ERKI/KI, n = 10). Mean ± SEM is shown. (G) Kaplan-Meier survival curves of serial 5-FU–treated Ctrl (n = 34), Hdac8Δ/Δ (n = 30), Hdac8Δ/Δ/p53ERKI/KI (n = 7), or p53ERKI/KI (n = 10) mice. *P < .05, **P < .01, ***P < .001.
Hyperactivation of p53 mediates hematopoietic deficiency and increased lethality in Hdac8-deficient mice challenged with serial 5-FU. (A) Schematic of experimental design. Two-month-old mice were induced by 7 doses of poly (I:C) and complete blood count analyzed 2 weeks later (time 0), followed by 5-FU (100 mg/kg) injection every 7 days. Mice were monitored for survival or analyzed for phenotypic HSPC populations by flow cytometry. (B) Relative expression of p53 and p53 target genes Bax, Bid, Gadd45b, Puma Stag1, and Cdkn1a in control (Ctrl) or Hdac8Δ/Δ LT-HSCs 2 days after treatment with 5-FU (100 mg/kg). (C) Frequency of activated caspase 3+ cells in phenotypic HSPC subpopulations 2 days after 5-FU treatment in Ctrl or Hdac8Δ/Δ mice (n = 3). Shown is mean ± SEM. (D-F) Weekly white blood cell (WBC), red blood cell (RBC), and platelet (PLT) counts of 5-FU–treated mice (Ctrl, n = 34; Hdac8Δ/Δ, n = 30; Hdac8Δ/Δ/p53ERKI/KI, n = 7; p53ERKI/KI, n = 10). Mean ± SEM is shown. (G) Kaplan-Meier survival curves of serial 5-FU–treated Ctrl (n = 34), Hdac8Δ/Δ (n = 30), Hdac8Δ/Δ/p53ERKI/KI (n = 7), or p53ERKI/KI (n = 10) mice. *P < .05, **P < .01, ***P < .001.
Discussion
Mechanisms that safeguard the maintenance and functional integrity of LT-HSCs under stress are critical for lifelong hematopoietic regeneration. In this study, we demonstrate that Hdac8 is a novel regulator of LT-HSC function in that it is critical for long-term hematopoietic repopulating activity and protection from hematopoietic stress. We show that loss of Hdac8 renders LT-HSCs hypersensitive to genotoxic and hematopoietic stress. Our results indicate that Hdac8 interacts with the p53 protein and modulates its activity via deacetylation. Inactivation of p53 completely rescued the hypersensitivity to stress and apoptosis of LT-HSCs caused by Hdac8 deletion. Altogether, this study highlights Hdac8 as a novel HSC regulator that ensures survival and functional integrity of LT-HSCs, particularly under hematopoietic stress.
As the master guardian of the genome, the p53 protein has vastly diverse functions, including cell-cycle arrest, DNA repair, senescence, and apoptosis. The activity of p53 is uniquely regulated in HSC to achieve an appropriate balance between maintaining the HSC pool and genetic integrity. Indeed, various genetic models harboring hyperactive p53 have shown increased apoptosis and decreased HSC pool size.6,27-29 We show that Hdac8 deficiency resulted in enhanced acetylation of p53 and thus hyperactivation of p53 in HSCs upon irradiation or 5-FU treatment. We observed that loss of p53 itself could speed up hematopoietic recovery, particularly erythropoiesis after 5-FU ablation (Figure 6E), consistent with reported roles of p53 in stress erythropoiesis.30-32 There was no significant change in Hdac8Δ/Δ LT-HSC apoptosis under steady state (supplemental Figure 4A-B). Consistent with the proapoptotic role of p53 in HSCs under stress, Hdac8Δ/Δ LT-HSCs expressed higher levels of Noxa and Puma and were prone to stress-induced apoptosis. Genetic inactivation of p53 reversed the upregulation of Noxa and Puma and rescued the apoptosis seen in Hdac8Δ/Δ LT-HSCs after irradiation, confirming that p53 indeed mediates these effects. In contrast, the cell-cycle inhibitor Cdkn1a was downregulated in Hdac8Δ/Δ LT-HSCs both before and after irradiation (Figure 5D). It has been shown that p53 functions to promote HSC quiescence in steady state.8,33 We performed cell-cycle analysis using Ki67/DAPI staining and found significant reduction in G0 phase and increase in G2/M phase, specifically in the Hdac8Δ/Δ LT-HSC and not other HSPC subpopulations (supplemental Figure 6A-J). Using an in vivo BrdU labeling (24 hours) assay, we also observed similar decrease in G0 cells and significant increase in S phase cells, specifically in the Hdac8Δ/Δ LT-HSC compartment (supplemental Figure 7A-I). In addition, steady-state Hdac8Δ/Δ LT-HSCs showed significantly reduced Cdkn1a and Ndn expression (supplemental Figure 7J), consistent with their reported role in maintaining HSC quiescence.8,34 Thus, an alternative regulatory mechanism likely mediates the reduced quiescence and Cdkn1a and Ndn downregulation in Hdac8Δ/Δ LT-HSCs. Nevertheless, increased HSC cycling could have contributed to the hypersensitivity to 5-FU, a cell cycle–dependent chemotherapeutic. Our study reveals that the function of Hdac8 is clearly cellular context and compartment specific, likely related to the distinct wiring of interconnected HSC regulatory networks operative in the stem-cell compartment during homeostasis and under stress.
It has been reported that other class 1 HDAC members have important functions in HSCs. Hdac1 and Hdac2, known to act in concert to promote G1-to-S progression,35 seem to have compensatory and overlapping functions in HSC maintenance.36,37 HDAC3, however, was shown to be essential for DNA replication in hematopoietic progenitor cells.38 We found that Hdac8 deletion caused hypersensitivity to stress and increased apoptosis specifically in the LT-HSC compartment. There was no apparent deficiency in short-term lineage differentiation capacity or steady-state survival of Hdac8-deleted HSPCs. Although Hdac8 deletion reduced BM cellularity and altered hematopoietic output in aged mice (>1 year), hematopoietic defects were only evident upon long-term serial repopulation and hematopoietic ablation, consistent with the specific effects in the LT-HSC population. Given that serial transplantation and aging processes place high demands and stress on LT-HSCs, p53-dependent hypersensitivity to stress may represent a major mechanism contributing to loss of HSC function over time. However, reduced quiescence through alternative regulatory target(s) likely also contributes to the loss of long-term repopulating capacity. Given that p53 also regulates HSC quiescence, it is difficult to separate the effects of p53 from the effects of quiescence in the context of Hdac8 deficiency and long-term repopulation activity. The NAD-dependent Sirtuin (SIRT)1 deacetylase, also capable of modulating p53 acetylation,39-42 was shown to be essential for HSPC homeostasis under stress and prevention of premature aging.43,44 However, the effects of Hdac8 deficiency are more restricted to the LT-HSC subpopulation compared with those of Sirt1 deletion. Given these differences in phenotypes seen in Hdac8-deficient mice, Hdac8 likely has unique regulatory functions in HSCs.
Loss-of-function mutations in HDAC8, located on the X chromosome q13, have been linked to Cornelia de Lange Syndrome (CdLS) and CdLS-like features.16,45-47 These HDAC8 mutations are associated with severely skewed X inactivation in the PB of female patients. CdLS, a dominantly inherited congenital malformation disorder, is typically associated with mutations in the cohesin loading protein NIPBL or less frequently with mutations in the core cohesin components SMC1A and SMC3. Mutations in cohesin complex members have been identified in myelodysplastic syndrome and AML.48-50 Recent studies have demonstrated a dose-dependent role of cohesin complex in normal and malignant hematopoiesis.51-54 Because HDAC8 was found to be responsible for deacetylation of cohesin components, HDAC8 deficiency resulted in increased acetylation of SMC3 and thus could have affected cohesin recycling.16 The distinct functional impacts seen between Hdac8-deficient and cohesion-deficient HSCs may have been due to a relatively minor impact of SMC3 acetylation on cohesin function and the dominant role of p53 in the HSCs. However, altered cohesin function and increased cell cycling could possibly feed into elevated replication stress in Hdac8-deficient LT-HSCs and contribute to its loss of functional integrity over time. Our findings likely explain the marked skewing and selection against the HDAC8-mutated allele seen in the PB of female patients with CdLS with heterozygote HDAC8 mutation.
Given the aberrant expression and activity of HDAC8 in a variety of cancers, HDAC8 represents a rational therapeutic target. Indeed, development of highly selective inhibitors has been achieved because of the unique structural characteristics of HDAC8.26,55-58 On the basis of our studies, no overall hematologic toxicity would be expected for on-target HDAC8 inhibition. It is noteworthy, however, that long-term adverse effects on HSCs, particularly under conditions of chemotherapy or hematopoietic stress, need to be considered.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported in part by the National Institutes of Health, National Cancer Institute under award #R01CA178387 (Y.-H.K.) and the Gehr Family Center for Leukemia Research. Research reported in this publication included work performed in the Analytical Cytometry Core and Animal Resource Center, supported by the National Cancer Institute of the National Institutes of Health under award #P30CA33572.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Authorship
Contribution: W.-K.H. designed and performed research, analyzed data, and wrote the manuscript; J.Q., Q.C., E.C., and M.A.R. performed research, analyzed data, and reviewed manuscript; L.L. and G.M. designed research and reviewed manuscript; and Y.-H.K. designed research, analyzed and interpreted data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ya-Huei Kuo, Department of Hematological Malignancies Translational Science, Gehr Family Center for Leukemia Research, Hematologic Malignancies and Stem Cell Transplantation Institute, Beckman Research Institute, City of Hope Medical Center, 1500 E. Duarte Rd, Duarte CA 91010; e-mail: ykuo@coh.org.

![Figure 1. Hdac8 contributes to HSC homeostasis and long-term CFC activity. (A) Relative expression levels of Hdac8 messenger RNA (mRNA) in sorted phenotypic HSPC and lineage populations (n = 2-7) assessed by SYBR Green–based quantitative reverse transcription polymerase chain reaction assays. Shown is the relative expression level (mean ± standard error of the mean [SEM]) for Hdac8 mRNA normalized to the Hprt mRNA expression level. (B) Schematic of experimental design (left). Mx1-Cre/Hdac8f/f(y) or controls (WT, Hdac8f/f(y), or Mx1-Cre) were injected with 7 doses (14 mg/kg) of poly (I:C) to induce the expression of Cre. Phenotypic analysis of HSPCs and CFC assays were performed 6 weeks after induction. Hdac8 protein levels in induced Mx1-Cre/Hdac8f/f(y) (Hdac8Δ/Δ) or control (Ctrl) BM cells shown by western blotting using Hdac8 specific antibody (right). (C) Frequency of various lineage populations in 2- to 3-month-old Hdac8Δ/Δ (n = 7) or Ctrl (n = 15) BM assessed by fluorescence-activated cell sorting. (D) Frequency of LT-HSC, short-term HSC (ST-HSC), and MPP subsets in Hdac8Δ/Δ (n = 10) or Ctrl (n = 13-19) BM. (E) Frequency of LSK, myeloid/erythroid progenitor populations in Hdac8Δ/Δ (n = 10) or Ctrl (n = 13-19) BM. (F) Number of CFU-Cs derived from Hdac8Δ/Δ or Ctrl BM cells (1 × 104 cells) in serial replating assays every 7 days. Shown is mean ± SEM with triplicates from 2 independent experiments. (G) The percentage of CFU-GEMM, CFU-GM, and BFUE colony types determined based on morphology. Shown is mean ± SEM with triplicates from 2 independent experiments. (H) Number of pre-B CFU-Cs derived from Hdac8Δ/Δ or Ctrl BM cells (1 × 104 cells). Shown is mean ± SEM. *P < .05, **P < .01, ***P < .001.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/24/10.1182_blood-2017-03-771386/4/m_blood771386f1.jpeg?Expires=1767777074&Signature=pahS-~6yCtRP8yCM22TU6dkrKVCxnGZOdzAbgDHaakIoLuboyIz-sUQOeSZhthi6cWJwgpx0SNTBItRUltwvKI7kbCA5ixbt2s0~cZAiKpaNpWNVd9tR6GERt-s5SWcUGg49wxjX0XTVq60HmSNHOKz02PYttcGapVAjO8bPCKp8yX0oYIa~eROQiOOxc6AuUHvTEJuM6EiuE8RjvADg9W1Ne70paw7ly04XoMqoSzpEMCRtD8WykHXcI8FpYbFhczoUE0uEkGyvKZmZlg4CwrDIuOR21BjTn9xinGYWsskhZt-RDsgxQbBpnv~I3jbLubkBbEJNhb-cY5osBK9n9Q__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)

![Figure 3. Hdac8 deletion leads to loss of long-term serial repopulating activity in vivo. (A) Schematic of experimental design. Mx1-Cre/Hdac8f/f(y)/mTmG+ (Hdac8Δ/Δ) or Mx1-Cre/mTmG+ (control [Ctrl]) mouse (CD45.2+; 2-3 months old) BM cells (2 × 105) were transplanted into lethally irradiated (11 Gy) CD45.1+ congenic recipients, along with CD45.1+ supporter BM cells (2 × 105). Cre-mediated deletion of Hdac8 was induced in recipients by 7 doses of poly (I:C). Phenotypic HSPCs and GFP chimerism in the BM were analyzed 16 weeks after transplantation by flow cytometry. (B) Percentage of GFP+ donor chimerism in various lineage population at 16 weeks (n = 5-7). (C) Frequency of GFP+ donor-derived lineage populations 16 weeks after the first transplantation (n = 5-7). (D-E) The frequency of GFP+ donor-derived phenotypic HSPCs in the BM analyzed at 16 weeks (n = 5). (F) Frequency of GFP+ donor-cell repopulation over time (8-16 weeks). (G) The frequency of GFP+ donor-derived lineage populations in PB of secondary recipients (n = 3). (H) Frequency of GFP+ donor-derived cells in tertiary transplant recipients (Ctrl, n = 8; Hdac8Δ/Δ, n = 4). Dashed line indicates 1%, above which is considered positive engraftment. (I) Phenotypic CD45.2+ LT-HSCs (200 cells) sorted from secondary recipient mice were transplanted along with CD45.1+ supporter BM cells (2 × 105) into lethally irradiated (11 Gy) CD45.1+ congenic recipients. Frequency of Ctrl or Hdac8Δ/Δ CD45.2+ donor-derived populations in the transplant recipients (Ctrl, n = 8; Hdac8Δ/Δ, n = 5-6) over time. Mean ± SEM is shown. *P < .05, **P < .01, ***P < .001. IR, irradiation.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/24/10.1182_blood-2017-03-771386/4/m_blood771386f3.jpeg?Expires=1767777074&Signature=jp6C5XJKZHMvyqQc4fIxji51lFc~kqVqaM3IIv-cJDxalZWmBT7UHg8TpGpyfLmZraEMJdN~4PPTxL-7TnD2OV2XXkOOG4qjQ3qDXhAhLG1AA-FTRD-BbvVH4CuAY5meVzNNz7tOwwH8HPVxnAqXCsyrdJgDZyyrZjgY3ILPdPt~Asnyqauy9WGXdkyNITbV-33iNKxg5tn~jEDelJlBsGP6GB4EqTeT44dSKEyKn~rJYojnY-bNpIMljyMtbYnRLovukd8IhUZvav9LJnFym0Gh3W8z1I6VLZsf8acwLSAmvGdlvBNHMwHMDhx1Q-hdmupwm4wi59IwJ0~tm-48Ag__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 5. Hdac8-deficient LT-HSCs are hypersensitive to p53-mediated apoptosis induced by genotoxic stress. (A) Schematic of experimental design. Hdac8f/f(y) (control [Ctrl]), Mx1-Cre/Hdac8f/f(y) (Hdac8Δ/Δ), or Mx1-Cre/Hdac8f/f(y)/p53ERKI/KI (Hdac8Δ/Δ/p53ERKI/KI) mice (2 months old) were induced by 7 doses of poly (I:C). Two weeks after induction, phenotypic LT-HSC, ST-HSC, MPP, and MP populations were sorted from BM and underwent irradiation (IR; 3 Gy). Gene expression was analyzed at 24 hours and apoptosis was assessed at 48 hours after exposure to radiation. (B) Representative FACS plots of annexin V/DAPI staining in sorted Ctrl, Hdac8Δ/Δ, or Hdac8Δ/Δ/p53ERKI/KI LT-HSCs with or without IR. (C) Frequency of annexin V+ cells in LT-HSC and MPP populations from Ctrl (n = 4), Hdac8Δ/Δ (n = 5), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) with or without IR. (D) Relative expression levels of Puma, Noxa, and Cdkn1a assessed by quantitative reverse transcription polymerase chain reaction in Ctrl (n = 4), Hdac8Δ/Δ (n = 5), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) LT-HSCs with or without IR. (E) Frequency of annexin V+ cells in the LT-HSC and MPP compartments of Ctrl (n = 6), Hdac8Δ/Δ (n = 6), Hdac8Δ/Δ/p53ERKI/+ (n = 7), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) mice 6 hours after whole-body IR (3 Gy). (F) Frequency of activated caspase 3+ cells in the LT-HSC and MPP compartment in Ctrl (n = 6), Hdac8Δ/Δ (n = 6), Hdac8Δ/Δ/p53ERKI/+ (n = 7), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) mice 6 hours after whole-body IR (3 Gy) assessed by intracellular staining followed by flow cytometry. Mean ± SEM is shown. *P < .05, **P < .01, ***P < .001.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/24/10.1182_blood-2017-03-771386/4/m_blood771386f5.jpeg?Expires=1767777074&Signature=OuJMby~cXwDJYBbi4A~xtA4UA8SvsZcRF3srHVuqlcS-7PFL7rtDQL7KPZIUqUMvSthQHRM-2BBR2DGo600PqRKzq6wOyhoeJ4B6mz1dCZ9dMQ6bk~UyQA41hkEjRCWI~6g257quB2PQhp8EhDcZDKrwn-J972QY2ZQIQd6u7FgvtZJcV7bBKm3U9~mrZgS~g17aB8ktMGFjCX~VvfAoDRKRJDY719dwLl8BRP2ZmkWklfCNz0jsaeA4oAftu7E6-KhNERxipXqx~rBTnE4hwYuqeYkt6parGLTZLDvhuDuBBXyaCbql1VDd6EuOty2t8SG~L8ILhKVUAEksIRnnvQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)


![Figure 1. Hdac8 contributes to HSC homeostasis and long-term CFC activity. (A) Relative expression levels of Hdac8 messenger RNA (mRNA) in sorted phenotypic HSPC and lineage populations (n = 2-7) assessed by SYBR Green–based quantitative reverse transcription polymerase chain reaction assays. Shown is the relative expression level (mean ± standard error of the mean [SEM]) for Hdac8 mRNA normalized to the Hprt mRNA expression level. (B) Schematic of experimental design (left). Mx1-Cre/Hdac8f/f(y) or controls (WT, Hdac8f/f(y), or Mx1-Cre) were injected with 7 doses (14 mg/kg) of poly (I:C) to induce the expression of Cre. Phenotypic analysis of HSPCs and CFC assays were performed 6 weeks after induction. Hdac8 protein levels in induced Mx1-Cre/Hdac8f/f(y) (Hdac8Δ/Δ) or control (Ctrl) BM cells shown by western blotting using Hdac8 specific antibody (right). (C) Frequency of various lineage populations in 2- to 3-month-old Hdac8Δ/Δ (n = 7) or Ctrl (n = 15) BM assessed by fluorescence-activated cell sorting. (D) Frequency of LT-HSC, short-term HSC (ST-HSC), and MPP subsets in Hdac8Δ/Δ (n = 10) or Ctrl (n = 13-19) BM. (E) Frequency of LSK, myeloid/erythroid progenitor populations in Hdac8Δ/Δ (n = 10) or Ctrl (n = 13-19) BM. (F) Number of CFU-Cs derived from Hdac8Δ/Δ or Ctrl BM cells (1 × 104 cells) in serial replating assays every 7 days. Shown is mean ± SEM with triplicates from 2 independent experiments. (G) The percentage of CFU-GEMM, CFU-GM, and BFUE colony types determined based on morphology. Shown is mean ± SEM with triplicates from 2 independent experiments. (H) Number of pre-B CFU-Cs derived from Hdac8Δ/Δ or Ctrl BM cells (1 × 104 cells). Shown is mean ± SEM. *P < .05, **P < .01, ***P < .001.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/24/10.1182_blood-2017-03-771386/4/m_blood771386f1.jpeg?Expires=1767812961&Signature=LuzznbxoQprULIiU0k~4SF-Ri0YdW77cQsx-dgCZptlfdZFREoJrnhvua8cc0A6OZquwETg8ntQLdncajrPQoyWmuBfv3MA4YqJaCmhMkg2oEsKj~E0NytIoVrrR4KxZG4BEA4r01AA6br1xA-KeBgJL2KGfWvPIaUAPPGexhD5vS5A57lJWIr3LwKEy-t7r3Bh7C8rorlCHGtidumpqQf1ihGjY0RWOBPLGCz2ZtQ8r04ugUIRBU43ZFEx1hd9m9M9zUeGb0qT~VY2lLKnfn5XmOGTLHZnjUKSNC6hlrYIkvDPAJxzQzJfh3dSKwOTQMcVbegYX4Yfa5JGwssOCkg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 3. Hdac8 deletion leads to loss of long-term serial repopulating activity in vivo. (A) Schematic of experimental design. Mx1-Cre/Hdac8f/f(y)/mTmG+ (Hdac8Δ/Δ) or Mx1-Cre/mTmG+ (control [Ctrl]) mouse (CD45.2+; 2-3 months old) BM cells (2 × 105) were transplanted into lethally irradiated (11 Gy) CD45.1+ congenic recipients, along with CD45.1+ supporter BM cells (2 × 105). Cre-mediated deletion of Hdac8 was induced in recipients by 7 doses of poly (I:C). Phenotypic HSPCs and GFP chimerism in the BM were analyzed 16 weeks after transplantation by flow cytometry. (B) Percentage of GFP+ donor chimerism in various lineage population at 16 weeks (n = 5-7). (C) Frequency of GFP+ donor-derived lineage populations 16 weeks after the first transplantation (n = 5-7). (D-E) The frequency of GFP+ donor-derived phenotypic HSPCs in the BM analyzed at 16 weeks (n = 5). (F) Frequency of GFP+ donor-cell repopulation over time (8-16 weeks). (G) The frequency of GFP+ donor-derived lineage populations in PB of secondary recipients (n = 3). (H) Frequency of GFP+ donor-derived cells in tertiary transplant recipients (Ctrl, n = 8; Hdac8Δ/Δ, n = 4). Dashed line indicates 1%, above which is considered positive engraftment. (I) Phenotypic CD45.2+ LT-HSCs (200 cells) sorted from secondary recipient mice were transplanted along with CD45.1+ supporter BM cells (2 × 105) into lethally irradiated (11 Gy) CD45.1+ congenic recipients. Frequency of Ctrl or Hdac8Δ/Δ CD45.2+ donor-derived populations in the transplant recipients (Ctrl, n = 8; Hdac8Δ/Δ, n = 5-6) over time. Mean ± SEM is shown. *P < .05, **P < .01, ***P < .001. IR, irradiation.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/24/10.1182_blood-2017-03-771386/4/m_blood771386f3.jpeg?Expires=1767812961&Signature=sNekLTAQXHKrtLALYB3Y7tNT8mV7JAdXLUzQOgUMHNjs4vmNE328~rJp-GVZfQ-WFaq4BnTolaoJA4Nr4IQbK~jIzABPGCuvVGh1ZTu8HsNtHIKw7sO-YPnXKCAXnKUcX6rUBsdbbZqc~14tsaOYgzPr5vR-CRLzrrUKra9Je9hNThtiSHK4OweeoScpmFLIqalZBZ0KMZrmxeXQHztKV7-3XsmrlVY7XwHj5~PuMCePhvyCwKL5fM5YirFHMVwWVJDj5wLjk7Kn088gUMTp2dV6jmJGX~7A5fBzRRKSzJhu2CIhS3Z0WtAFhf1EM1oIoSILmuMhvqG6AjImURjS7w__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
![Figure 5. Hdac8-deficient LT-HSCs are hypersensitive to p53-mediated apoptosis induced by genotoxic stress. (A) Schematic of experimental design. Hdac8f/f(y) (control [Ctrl]), Mx1-Cre/Hdac8f/f(y) (Hdac8Δ/Δ), or Mx1-Cre/Hdac8f/f(y)/p53ERKI/KI (Hdac8Δ/Δ/p53ERKI/KI) mice (2 months old) were induced by 7 doses of poly (I:C). Two weeks after induction, phenotypic LT-HSC, ST-HSC, MPP, and MP populations were sorted from BM and underwent irradiation (IR; 3 Gy). Gene expression was analyzed at 24 hours and apoptosis was assessed at 48 hours after exposure to radiation. (B) Representative FACS plots of annexin V/DAPI staining in sorted Ctrl, Hdac8Δ/Δ, or Hdac8Δ/Δ/p53ERKI/KI LT-HSCs with or without IR. (C) Frequency of annexin V+ cells in LT-HSC and MPP populations from Ctrl (n = 4), Hdac8Δ/Δ (n = 5), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) with or without IR. (D) Relative expression levels of Puma, Noxa, and Cdkn1a assessed by quantitative reverse transcription polymerase chain reaction in Ctrl (n = 4), Hdac8Δ/Δ (n = 5), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) LT-HSCs with or without IR. (E) Frequency of annexin V+ cells in the LT-HSC and MPP compartments of Ctrl (n = 6), Hdac8Δ/Δ (n = 6), Hdac8Δ/Δ/p53ERKI/+ (n = 7), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) mice 6 hours after whole-body IR (3 Gy). (F) Frequency of activated caspase 3+ cells in the LT-HSC and MPP compartment in Ctrl (n = 6), Hdac8Δ/Δ (n = 6), Hdac8Δ/Δ/p53ERKI/+ (n = 7), or Hdac8Δ/Δ/p53ERKI/KI (n = 3) mice 6 hours after whole-body IR (3 Gy) assessed by intracellular staining followed by flow cytometry. Mean ± SEM is shown. *P < .05, **P < .01, ***P < .001.](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/130/24/10.1182_blood-2017-03-771386/4/m_blood771386f5.jpeg?Expires=1767812961&Signature=Zw4JuU8Q9WZ6-hellj-A6f15h052NQGJ7gT5o3-ULW8DCJorI85dNvrCDOy26Jkh1xE52DLOlp~6-XWzFQAnGtG6OBo0DHEB1M9uuJiuV~IN8KGc6cKCJpZIlacqHAJoblO3fupKsW9XFNFP5V0fNM12pyivXv2f-~f0tpewB2SfaP0ftcGQypmCEvxoQ5hseul3GrPBETKxdoseINz8JQ22NnmJJau~vc1w7XmEtkoMJS2EYLgPjVRqTQYQpwXU4MBa5OwxJtMHTNKM5EEvAHOHMLap1iGdwmqW94uwVJhpnefa~JaUulXRXBwNc6gz6z1sQW8TQ2knjQ52QGftDA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)