The proteasome degrades unneeded and damaged proteins. Tumor cells highly depend on increased protein production and their degradation suggesting that malignant cells with a high proliferation index will be more sensitive to proteasome inhibition. The addition of the proteasome inhibitor Bortezomib (Velcade, 'BTZ') to standard pediatric AML chemotherapy (cytarabine, daunorubicin and etoposide, 'ADE') depleted leukemia-initiating cells in a phase 2 clinical trial in pediatric AML (pedi-AML) patients. A randomized phase 3 clinical trial was then conducted by the Children's Oncology Group (COG) comparing ADE and ADE+BTZ treatment regimes in pedi-AML (AAML1031). To determine if there were specific protein expression profiles that correlated with response to BTZ-containing chemotherapy, we analyzed key components of the proteome of pedi-AML that participated in the trial using reverse phase protein arrays (RPPA).
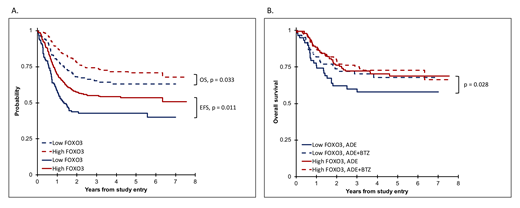
RPPA-based expression of 293 validated antibodies was tested in 500 leukemia samples and compared to expression in CD34+ samples from healthy individuals (n=30). Among all proteins, FOXO3 expression was identified as the protein with the highest influence on outcome in the ADE group. The expression of FOXO3 was prognostic for event-free survival (EFS) in both univariate (HR = 0.56, 95% CI = 0.34-0.90, P = 0.017) and multivariate (HR = 0.55, 95% CI = 0.34-0.88, P = 0.013) analysis. All patients were divided into two clusters (low and high) based on their FOXO3 expression level using median FOXO3 expression in normal CD34+. Kaplan-Meier survival analysis showed poor OS (3 year OS 65.3% vs. 73.9%, P = 0.03) and EFS (3 year EFS, 42.8% vs. 55%, P = 0.01) in low FOXO3 expressors (n=119) compared to patients with high FOXO3 expression (n=291) (fig. 1A). Notably, the poor prognostic effect of low FOXO3 for OS was seen in ADE (3 year OS 60% vs. 72.3%, P = 0.03), but not in ADE-BTZ (3 year OS 70.3% vs. 75.3%, P = 0.23) (fig. 1B). This suggests that in particular patients with low FOXO3 may be eligible candidates for BTZ-addition.
To validate our findings, we performed knockdown (KD) of FOXO3 using a short hairpin approach in OCI-AML3 (p53WT) and THP-1 (p53null) cell lines. KD FOXO3 in OCI-AML3 had a short-term growth advantage compared to controls (Day 4, P = 0.004), but not KD FOXO3 THP-1 cells suggesting a role for p53 in the FOXO3 functional pathway. KD FOXO3 cells were more resistant to doxorubicin and etoposide combination therapy than controls (P = 0.04), confirming our clinical observations. Since therapeutic regimes in AML are currently shifting towards Bcl-2 inhibition by Venetoclax (ABT-199, 'ABT'), we were eager to test whether BTZ and ABT could act in synergy, and if this is related to FOXO3 expression. Single low dose BTZ and ABT did not reduce cell numbers after 3 days, but were effective when used in combination (<12% survival, P < 0.001) in OCI-AML3 and THP-1. Although cell counts were lower regardless FOXO3 status in both cell lines, flow cytometry analysis using Annexin V staining revealed significant more apoptosis in KD FOXO3 THP-1 compared to controls.
Using RPPA-based profiling, we identified a cluster of pedi-AMLs that benefitted from BTZ-addition to standard therapy. We hypothesize that AML patients with low FOXO3 levels have less activation of their apoptotic transcriptional programs and that this subgroup may benefit from proteasome blockage to prevent FOXO3 proteasomal degradation. The use of FOXO3 as potential biomarker may identify a prognostically adverse cluster in pedi-AML that could stratify patients for ADE+BTZ therapy. Patients with low FOXO3 expression may potentially benefit from ADE+BTZ in combination with ABT, a novel and promising combination approach in AML that warrants further investigation.
Figure 1. A. Kaplan meier analysis comparing overall survival (OS) and event-free survival (EFS) between low (n=119, blue) and high (n=291, red) FOXO3 expression in pedi-AML patients. Children with low FOXO3 had significantly poorer OS (P = 0.033, Wilcoxon) and EFS (P = 0.011, Wilcoxon). B. Overall survival between ADE (solid) and ADE+BTZ (dashed) treated patients based on low (blue) or high (red) FOXO3 protein expression. The poor prognostic effect of FOXO3 is present in ADE, but not in ADE+BTZ treated patients (P = 0.028, Wilcoxon).
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.