Background:
Novel agents such as IMIDs and proteasome inhibitors have substantially changed the therapeutic landscape in the first line treatment of multiple myeloma (MM). Better response rates and prolonged progression-free survival have lead to an improvement in overall survival (OS) with median values well beyond 5 years. Therefore to assess whether first line therapy strategies have an impact on the prognosis for patients with MM, long-term results of clinical trials with follow up covering >10 years are necessary.
Methods:
The HOVON-65/GMMG-HD4 study is a prospective randomized trial testing bortezomib+adriamycin+dexamethasone (PAD) for 3 cycles as induction prior to high-dose chemotherapy (HDT) and autologous stem cell transplantation compared to vincristine+adriamycin+dexamethasone (VAD) in the control arm. After one (HOVON) or two (GMMG) HDT maintenance was given for 2 years consisting of bortezomib every 2 weeks in the PAD arm and thalidomide 50 mg daily in the VAD arm. The study results were initially reported in 2012 (1) and with a median follow up of 91 months in 2018 (2). In this analysis we present OS results after a median follow up of 137 months. All hazard ratios (HR) are given with 95% confidence intervals (CI).
Results:
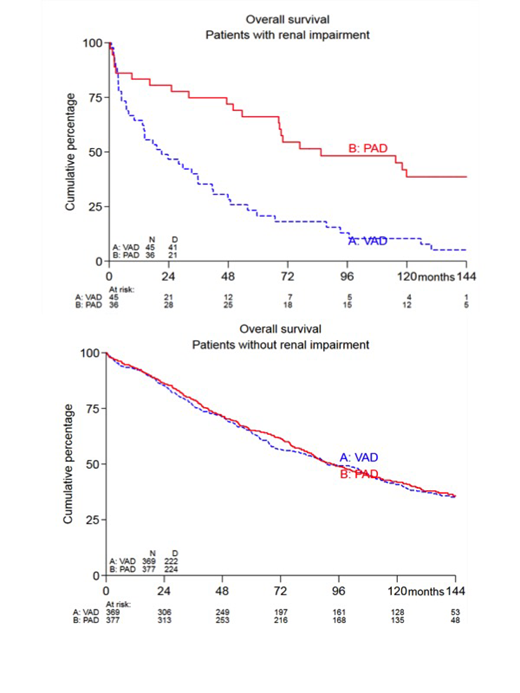
Overall survival at 12 years was 32% (CI 27-37%) in the VAD arm versus 36% (CI 31-41%) in the PAD arm without significant difference in the univariate Cox model (HR 0.87, CI 0.73 - 1.03, p=0. 11 or in multivariate Cox model including ISS stage and treatment arm (HR 0.87, CI 0.73 - 1.04, p=0.12; the primary analysis) as specified in the study protocol. When other factors including age, sex, ISS stage, WHO performance status, Immunoglobulin-type, Durie and Salmon-stage, LDH, del 13q, study group and renal impairment (RI, defined as serum creatinine ≥ 2 mg/dl) were added to the Cox model, treatment in the PAD arm was a significant factor for improved OS (HR 0.84, CI 0.7 - 1.0, p=0.048). Of the remaining factors age (HR 1.02, CI 1.01 - 1.03, p=0.002), female sex (HR 0.83, CI 0.69 - 0.99, p=0.044), ISS stage (HR 1.19, CI 1.04 - 1.35, p=0.01), WHO performance status (HR 1.32, CI 1.17 - 1.48, p<0.001), IgA (HR 1.56, CI 1.18 - 2.06, p=0.002), LDH>ULN (HR 1.44, CI 1.14 - 1.82, p=0.002), del 13q (HR 1.42, CI 1.17 - 1.73, p<0.001) and RI (HR 1.42, CI 1.04 - 1.95, p=0.026) were significantly associated with OS. Tests for heterogeneity revealed two factors as significant: RI and del17p (only fully evaluated for the GMMG cohort). For patients with RI the OS probability at 12 years was 39% in the PAD arm versus 5% in the VAD arm (HR 0.34, CI 0.20 - 0.59, p<0.0001, Fig. 1). 12 year OS in patients without RI was 36% in the PAD arm and 35% in the VAD arm without significant difference (HR 0.97, CI 0.81 - 1.17, p=0.77, Fig,1). In the GMMG cohort (receiving tandem-HDT) del17p results were available and patients with del17p had a significantly better OS in the PAD arm than in the VAD arm (HR 0.36, CI 0.17 - 0.77, p=0.006), while no significant difference between treatment arms was found in patients without del17p (HR 1.01, CI 0.75 - 1.37, p=0.92).
Discussion:
Long-term results of the HOVON-65/GMMG-HD4 trial show that one third of patients receiving HDT with either thalidomide-based or bortezomib-based maintenance are still alive at 12 years. In contrast to earlier analyses with shorter follow up (1,2) the use of bortezomib in the induction and maintenance treatment provided a significant OS benefit when adjusting for other risk in a multivariate Cox model, although not in the primary analysis. A particular OS benefit was found in patients with RI receiving bortezomib before and after HDT and this could completely abolish the negative prognostic impact of RI. Similarly bortezomib used in combination with tandem-HDT improved OS in patients with del17p so that more than a third of these patients with high-risk MM survived more than 10 years. Our results underline that despite the growing options for treatment at relapse the choice of an optimal first-line therapy is of critical prognostic importance, in particular for patients with high-risk myeloma.
References:
1) Sonneveld et al., J Clin Oncol, 2012; 30:2946-2955
2) Goldschmidt et al., Leukemia 2018; 32: 383-390
Scheid:Bristol Myers Squibb: Honoraria; Celgene: Honoraria; Amgen: Consultancy, Honoraria; Janssen: Consultancy, Honoraria, Research Funding; Takeda: Honoraria, Research Funding; Novartis: Honoraria, Research Funding. Bertsch:Celgene: Other: travel support; Sanofi: Other: travel support. Zweegman:Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees, Research Funding. Weisel:Celgene: Consultancy, Honoraria, Research Funding; Juno: Consultancy; Bristol-Myers Squibb: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria, Research Funding; GSK: Honoraria; Adaptive Biotech: Consultancy, Honoraria; Janssen: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria. Kersten:Gilead: Honoraria; Kite Pharma: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Novartis: Honoraria; Bristol-Myers Squibb: Honoraria, Research Funding; Mundipharma: Honoraria, Research Funding; Miltenyi: Honoraria; Roche: Honoraria, Research Funding; Takeda Oncology: Research Funding; Celgene: Honoraria, Research Funding. Mai:Mundipharma: Other: travel support; Takeda: Honoraria, Other: travel support, Research Funding; Janssen: Consultancy, Honoraria, Other: travel support; Celgene: Consultancy, Honoraria, Other: travel support. Hillengass:Amgen: Consultancy, Honoraria; Janssen: Honoraria. Stilgenbauer:AbbVie, AstraZeneca, Celgene, Gilead Sciences, Inc., GSK, Hoffmann La-Roche, Janssen, Novartis: Consultancy, Honoraria, Research Funding, Speakers Bureau. Broyl:Celgene, amgen, Janssen,Takeda: Honoraria. Bos:Kiadis Pharma: Other: Shareholder (of Cytosen, acquired by Kiadis); Celgene: Research Funding. Dührsen:Amgen: Consultancy, Honoraria, Research Funding; CPT: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria; Roche: Honoraria, Research Funding; Teva: Honoraria; Novartis: Consultancy, Honoraria; Alexion: Honoraria; Gilead: Consultancy, Honoraria; Takeda: Consultancy, Honoraria; Janssen: Honoraria; Celgene: Research Funding. Salwender:Celgene: Honoraria, Other: Travel or accommodations; Sanofi: Honoraria, Other: Travel or accommodations; Takeda: Honoraria, Other: Travel or accommodations; Bristol-Myers Squibb: Honoraria, Other: Travel or accommodations; AbbVie: Honoraria; Amgen: Honoraria, Other: Travel or accommodations; Janssen Cilag: Honoraria, Other: Travel or accommodations. Goldschmidt:Adaptive Biotechnology: Membership on an entity's Board of Directors or advisory committees; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Molecular Partners: Research Funding; Dietmar-Hopp-Stiftung: Research Funding; Mundipharma: Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding; John-Hopkins University: Research Funding; Amgen: Consultancy, Research Funding; Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Chugai: Honoraria, Research Funding; John-Hopkins University: Research Funding; Sanofi: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; MSD: Research Funding; Janssen: Consultancy, Research Funding. Sonneveld:Amgen: Honoraria, Research Funding; BMS: Honoraria; Celgene: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Karyopharm: Honoraria, Research Funding; Takeda: Honoraria, Research Funding; SkylineDx: Research Funding.
bortezomib maintenance thalidomide maintenance
Author notes
Asterisk with author names denotes non-ASH members.