Abstract
Background To assess the optimal treatment strategy for fit older patients with acute myeloid leukemia (AML), we performed a large international phase III randomized controlled trial (RCT) in fit AML patients aged >60 years, comparing 10-day decitabine (DEC) followed by allografting (HSCT) versus intensive chemotherapy (IC, "3+7" regimen) followed by HSCT. This trial revealed comparable HSCT rates and survival outcomes, but a more favorable safety profile with DEC when compared to IC (Lübbert M. et al, HemaSphere, 6, 26-27, 2022), supporting the hypothesis that reduced toxicity translates into a better health-related quality of life (HRQoL).
Objective We hereby report the HRQoL outcomes of this international RCT.
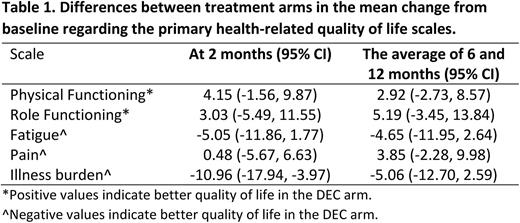
Patients and Methods HRQoL was a secondary endpoint and was assessed by the EORTC QLQ-C30 and its validated module for evaluating HRQoL in older patients, namely the EORTC QLQ-ELD14. Key inclusion criteria were: newly diagnosed AML, age >60 years, eligibility for IC, and a WHO performance status of ≤2. Assessments of HRQoL were performed at baseline and then at 2 (at regeneration after two treatment cycles), 6 and 12 months. For patients undergoing a HSCT, HRQoL was assessed prior to the procedure and at day 100 after the transplant. Quality of life deterioration (QD) was defined as any of the following events: death, progression, and clinically meaningful deterioration from baseline in at least one of the five pre-selected primary HRQoL scales (i.e., physical functioning, role functioning, fatigue, pain, and illness burden). The two co-primary endpoints were: QD at 2 months and QD at 6 or 12 months. A difference of 10 points or more was considered clinically meaningful. We hypothesized better HRQoL outcomes for patients treated with DEC. The changes in the primary HRQoL scales from baseline to 2 months and from baseline to the average of 6 and 12 months were secondary HRQoL endpoints. HRQoL trajectories of patients undergoing HSCT on-study based on evaluations at baseline, prior to HSCT and at day 100 after HSCT were also described. This study was registered at ClinicalTrials.gov (NCT02172872).
Results Between December 2014 and August 2019, 606 patients were randomized and a baseline HRQoL assessment was available for 549 patients (91%): 279 out of 303 in the DEC arm and 270 out of 303 in the IC arm. Compliance among alive patients at 2, 6 and 12 months was 57%, 57%, and 64%, respectively. The proportion of patients evaluable for QD at 2 months was 60%. The proportion of patients evaluable for QD at 6 or 12 months was 82%.
Analysis of the primary HRQoL endpoint showed that the proportion of patients deteriorating at 2 months was 76% (95% CI, 69 to 82%) in the DEC group vs 88% (95% CI, 82 to 93%) in the IC group (odds ratio 0.43 [95% CI, 0.24 to 0.76], P=.003). Several sensitivity analyses, using multiple imputation to deal with missing values and predefined modifications of the definition of QD, confirmed this finding. QD analysis at 6 or 12 months indicated no statistically significant difference between both arms (odds ratio 0.83 [95% CI, 0.46 to 1.52]).
At 2 months from randomization, the illness burden scale increased by 4.19 (95% CI, -0.44 to 8.83) points in the DEC and by 15.15 (95% CI, 9.88 to 20.42) points in the IC arm, indicating a clinically meaningful and statistically significant difference of -10.96 (95% CI, -17.94 to -3.97), P=.004. The changes in the primary HRQoL scales from baseline to 2 months and from baseline to the average of 6 and 12 months are presented in Table 1.
Baseline data were available for 218 of the 240 patients who received an on-study HSCT. Clinically meaningful HRQoL deteriorations between baseline and post-HSCT in the IC group were observed in all primary HRQoL scales except for pain. The change from baseline to post-HSCT HRQoL in the DEC arm appeared less pronounced and did not reach the threshold of clinical relevance.
Conclusions Following two months of treatment, there was a significantly lower percentage of patients treated with DEC who reported HRQoL deterioration, compared to those treated with IC. Additionally, patients treated with DEC did not experience any clinically meaningful deterioration in key pre-specified HRQoL domains post-HSCT, while this was the case for patients treated with IC.
Disclosures
Efficace:Abbvie: Consultancy, Research Funding; Janssen: Consultancy; Novartis: Consultancy, Research Funding; Amgen: Research Funding. Kicinski:MSD, Pierre Fabre, BMS, Janssen: Research Funding. Griskevicius:Miltenyi Biomedicine: Membership on an entity's Board of Directors or advisory committees. Luppi:Gilead sci: Other: Travel grant; Abbvie, Jazz Pharma, Gilead sci, MSD, Novartis, Sanofi, Daiichi-Sankyo, Grifols: Membership on an entity's Board of Directors or advisory committees. Fuhrmann:Amgen, Sanofi, GSK, Gilead Sci, Roche and Janssen: Other: Advisory Board. Crysandt:Pfizer: Honoraria; Astra Zeneca: Honoraria; Novartis: Honoraria. Gaidano:Roche: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Incyte: Membership on an entity's Board of Directors or advisory committees; Beigene: Membership on an entity's Board of Directors or advisory committees; Astra-Zeneca: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Vrhovac:Abbvie, Astellas, Pfizer, Pharmas: Consultancy; Abbvie, Astellas, MSD, Novartis, Pfizer, Pharmas, Servier, Teva: Speakers Bureau. Venditti:Medac: Consultancy; Jazz Pharmaceuticals: Honoraria, Research Funding; Janssen & Cylag: Honoraria; Astellas: Membership on an entity's Board of Directors or advisory committees; Amgen: Membership on an entity's Board of Directors or advisory committees; astrazeneca: Honoraria; abbvie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Pfizer: Honoraria, Speakers Bureau; Servier: Membership on an entity's Board of Directors or advisory committees. Candoni:Celgene, Abbvie, Pfizer, Janssen, Astellas, Jazz, Gilead, Incyte, Amgen: Other: Speaker honoraria. Baron:Celgene, Abbvie, Novartis, Pfizer: Other: Travel grant; Abbvie and Sanofi: Other: Speaker honoraria. Vignetti:IQVIA, Dephaforum, AbbVie, Astrazeneca: Speakers Bureau. Luebbert:AbbVie: Honoraria; Astex: Honoraria; Janssen: Research Funding; Otsuka: Consultancy; Syros: Consultancy; Cheplapharm: Other: study drug.
Author notes
Asterisk with author names denotes non-ASH members.