Abstract
The concept that myeloablation to open space was a prerequisite for marrow stem cell engraftment has been challenged by studies showing high rates of engraftment in nonmyeloablated mice (Stewart et al,Blood 81:2566, 1993; Quesenberry et al, Blood Cells20:97, 1994; Brecher et al, Blood Cells 5:237, 1979; Saxe et al, Exp Hematol 12:277, 1984; and Wu et al, Exp Hematol21:251, 1993). However, relatively large numbers of marrow cells were necessary to achieve high long-term donor percentages. We have demonstrated, using a BALB/c male/female marrow transplant model and detecting male DNA in host tissues by Southern blot or fluorescent in situ hybridization, that exposure to doses of irradiation that cause minimal myeloablation (50 to 100 cGy) leads to very high levels of donor chimerism, such that relatively small numbers of marrow cells (10 to 40 million) can give donor chimerism in the 40% to 100% range. Studies of radiation sensitivity of long-term engrafting cells have shown that 100 cGy, although not myelotoxic, is stem cell toxic, and indicate that the final host:donor ratios are determined by competition between host and donor stem cells. These data indicate that low levels of irradiation should be an effective approach to nontoxic marrow transplantation in gene therapy or in attempts to create allochimerism to treat such diseases as cancer, sickle cell anemia, or thalassemia.
CLASSIC TRANSPLANTATION models involve lethal myeloablation, a setting in which a few or very large numbers of infused marrow stem cells will give 100% donor cells after transplantation; in the case of low numbers of infused marrow cells, hematopoiesis in the transplanted animal is oligoclonal,1,2whereas with large numbers, polyclonal hematopoiesis ensues.3 In addition, lower levels of irradiation have been extensively evaluated for effects on marrow recovery, but not in a quantitative fashion in syngeneic or autologous models, because most studies have not used cells with a donor-specific marker.
We have previously described very high levels of stable marrow cell engraftment in normal nonmyeloablated murine hosts, a model in which donor cells are competed against host cells.4 Data on cell dose effects suggested that donor cell engraftment was quantitative at the stem cell level and that the final percentage of donor chimerism might be determined by the ratio of host to donor stem cells, rather than by any effect on opening space for stem cell engraftment.5 Previous studies using a variety of stem/progenitor assays have indicated relatively high rates of killing at levels of irradiation between 50 and 100 cGy.6 7 The present data suggest that 40 million male BALB/c marrow cells with quantitative stem cell engraftment into female BALB/c hosts exposed to 50 to 100 cGy total body irradiation, a level that might eliminate the bulk of host stem cells (vide infra), should give high donor-host ratios in marrow, spleen, and thymus.
MATERIALS AND METHODS
Mice.
Six- to 8-week-old BALB/c H-2D mice (Taconic Farm, Germantown, NY) were housed in a conventional clean facility for at least 1 week before experimental use. Mice received mouse chow and acidified water ad libitum.
Marrow cell suspension.
Mice were killed by cervical dislocation and bone marrow collected from tibia and femurs. Cells were flushed from femurs and tibia with cold phosphate-buffered saline (PBS) supplemented with 5% heat-inactiviated (HI) fetal calf serum (FCS; Hyclone, Logan, UT) and filtered through a 40-μm filter (Becton Dickinson, Franklin Lakes, NJ). The cells were washed and suspended for injection in PBS.
Transplantation.
Normal or irradiated female BALB/c mice were infused with from 1 × 106 to 40 × 106 normal male BALB/c marrow cells or 40 × 106 irradiated male BALB/c marrow cells, and the percentage of male DNA per female was determined by Southern blot analysis as described below.
Southern blot.
Spleen, thymus, and marrow cell extracts were prepared by lysis in 0.15 mol/L NaCl, 0.02 mol/L Tris, 0.02 mol/L EDTA, and 1% sodium dodecyl sulfate followed by organic extraction with proteinase K (Sigma, St Louis, MO), RNAse (Sigma), and phenol-chloroform and precipitation in ethanol. The presence of Y-specific DNA sequences was assessed using a pY2-cDNA probe (donated by I. Lemischka, Princeton University, Princeton, NJ). DNA samples were digested with the restriction enzyme Dra I and separated by gel electrophoresis in 0.8% agarose (GIBCO, Richmond, CA) according to established Southern blotting techniques. Sample loading was assessed by reprobing membranes with a partial or full length cDNA for interleukin-3 (donated by J. Ihle and DNAX, Palo Alto, CA). Probes were32P-labeled using a random primed labeling kit (Boehringer Mannheim, Mannheim, Germany) and autoradiographs were made using Kodak XRP x-ray film (Eastman Kodak, Rochester, NY). Blots were exposed to photostimulatable storage phosphorimaging plates, and the percentage of male and female DNA was quantitated after scanning the plates with a GS-363 molecular imager system (Bio-Rad, Hercules, CA).
Differential cell count.
Cells from spleen samples from posttransplant mice were centrifuged onto slides (500 rpm for 5 minutes) by cytospin (Shandon, Pittsburgh, PA). Slides were fixed in 100% methanol and stained with Wright-Giemsa staining. At least 100 mononuclear cells were counted using the Nikon E400 (MicroVideo Instruments, Avon, MA) with 40× lens to determine lymphocyte percentages.
Fluorescence in situ hybridization (FISH).
Cytospins were fixed in a 50% Carnoys (75% methanol/25% acetic acid) and 50% PBS solution for 10 minutes before being baked at 72°C for 1 hour. The slides were then further fixed in 100% Carnoys for 5 minutes before permeabilization using proteinase K (0.2 μg/mL) enzymatic digestion in 2 mmol/L CaCl2 and 20 mmol/L Tris buffer (pH 7.5) at 37°C for 1.5 minutes. The cytospins were dehydrated once more and hybridized with a digoxigenin-labeled Y chromosome-specific probe at 45°C overnight. Unbound probe was removed by stringent washings in 3 changes of 50% formamide in 2× SSC and 2 changes of 2× SSC at 45°C. After washing in 4× SSC (0.6 mol/L NaCl and 0.06 mol/L sodium citrate, pH 6.4) at room temperature, the slides were bleached using a blocking buffer consisting of 5% FCS, 5% nonfat milk (Shaw's, Bridgewater, MA) and 0.05% Triton X-100 (Sigma) in 4× SSC for 15 minutes. Detection of digoxigenin was performed using anti-digoxigenin rhodamine–labeled Fab fragments (Boehringer Mannheim) at a concentration of 6.5 μg/mL in PBS containing 2% bovine serum albumin (BSA) fraction V (Sigma) for 30 minutes in the dark. Nonbound antibody was removed through three extensive, light-protected washings: first in 4× SSC for 10 minutes, then in 4× SSC containing 0.05% Triton X-100 for 10 minutes, and finally in 4× SSC for 10 minutes. Cytospins were counterstained in 0.4 μmol DAP1 (4.6-Diamidino-2-phenylindole; Sigma) and mounted in the antifade media Vectashield (Vector, Burlingame, CA). Specific positive label was confirmed under the microscope by a visual check at excitation and emission wavelength other than that of rhodamine.
FISH on sections of paraffin-embedded whole murine femur.
Sections of paraffin-embedded murine femurs were prepared as previously noted.8 Mice were perfused with 4% paraformaldehyde into the descending aorta and femurs were removed, decalcified in EDTA, dehydrated in graded ethanol, and cleared in mineral spirits (Aldrich Chemical Co, Milwaukee, WI) before infiltration and embedding in Paraplast x-tra (Oxford Labware, St Louis, MO). Five-micrometer femoral sections were mounted on 0.01% poly-L-lysine (molecular weight 150,000 to 300,000; Sigma Diagnostics, St Louis, MO) subbed slides, deparaffinized in xylene, rehydrated in graded ethanol, and washed in distilled water and then PBS. Binding to nonspecific proteins was blocked using blocking buffer consisting of 5% FCS, 5% nonfat milk (Shaw's) and 0.05% Triton X-100 (Sigma) in 4× SSC (0.06 mol/L NaCl and 0.06 mol/L sodium citrate, pH 6.4) for 15 minutes at room temperature. The FISH-labeled sections were mounted using Vectashield (Vector), and each section was mounted in approximately 5 μL of mounting media. The cover slips were sealed with nail polish. Mounted slides were stored at 4°C protected from light. Sections were evaluated using a Nikon Microphot-FXA microscope equipped for epifluorescence (100-W high-pressure mercury lamp; MicroVideo Instruments). Sections were viewed using a 40/1.0 oil Nikon objective. Fluorescent photomicrographs were taken with Kodak Ektachrome EL IS0 400/27°C. UV excitation was performed to evaluate nonspecific autofluorescence not representing the male signal.
Irradiation of cells or mice.
Balb/c female hosts, Balb/c male donors, or male Balb/c marrow cells suspended in PBS in 50-mL conical tubes received varying doses of irradiation from a cesium source (Gamma cell 40; Nordian, Kanata, Ontario, Canada) at a dose rate of 92 to 94 cGy/min.
Purification of stem cells.
Bone marrow was collected from femurs, tibia, and iliac crests by grinding in PBS supplemented with 5% HI FCS (Hyclone) using a mortar and pestle. The bone fragments were washed multiple times and the supernatant cell suspension and wash fractions were filtered through a 40-μm filter (Becton Dickinson) to remove large bone particles. High lipid concentrations were reduced by the centrifugation and resuspension of the cells in fresh buffer. The cells were allowed to sit on ice for 5 minutes so that small bone particles would settle out. The cell supernatant, depleted of these fragments, was then diluted to 107 cells/mL PBS 5% HI FCS.
Lineage-negative cells were isolated in a manner very similar to that previously described by Bertoncello et al.9 Briefly, low-density cells (<1.0777 g/mL) were isolated by discontinuous density centrifugation using Nycoprep for animals (Accurate Chemical and Scientific Corp, Westbury, NY), washed, and resuspended at 108 cells/mL PBS 5% HI FCS. Cells were labeled with a cocktail of primary antibodies: anti-B220 (B cells) Coffman10; anti–Mac-1 (macrophages)11; anti–Gr-1 (neutrophils)12; anti–Lyt-2 (CD8) and anti-L3T4 (CD4) (T cells) Cobbold13(Becton Dickinson); YW25.12.7 (erythroid precursors)14; and TER119 (erythrocytes; a kind gift from Tatsuo Kina, Chest Research Institute, Kyoto University, Kyoto, Japan). Each batch of antibody was evaluated by flow cytometric analysis for the concentration that resulted in the greatest shift in mean channel fluorescence and/or the percentage of positive cells detected. The optimal dilution for each antibody was in the range of 1:10 to 1:100 (final). After 15 minutes of incubation on ice, the labeled cells were washed in PBS 5% HI FCS and resuspended at 108cells/mL PBS 5% HI FCS. The cells were incubated with sheep antirat IgG-conjugated immunomagnetic polystyrene spheres (M-450 Dynabeads; Dynal, Lake Success, NY) at 4°C for 3 minutes by adding a 1:1 bead:cell ratio. The beads were suspended in PBS 5% HI FCS and, when added to the cells, resulted in 1.5 times the original cell volume. Immunomagnetic bead-rosetted cells were removed using a magnetic particle concentrator (Dynal MPC-6), and the unrosetted cells remaining in suspension were obtained by pipette. The beads were washed three times, and the supernatant was pooled with the cell suspension. The unrosetted cells were further incubated with antirat-conjugated immunomagnetic beads at 4°C for 20 minutes by adding a 4:1 bead:cell ratio, resulting in double the original cell volume. Again, immunomagnetic bead-rosetted cells were removed using a magnetic particle concentrator, and the unrosetted cells remaining in suspension were harvested by pipette. The beads were washed three times, and the supernatant was pooled with the cell suspension.
Rhodamine 123 (Rho)/Hoechst 33342 (Ho) labeled cell separation.
Immunomagnetically enriched cell suspensions were washed and resuspended at 106 cells/mL in PBS 5% HI FCS and incubated in a final Rho concentration 0.1 μg/mL for 20 minutes at 37°C in the dark. A final Ho concentration of 10 μmol/L was then added, and the cells were incubated at 37°C in the dark for 1 further hour. The cells were washed in ice-cold PBS 5% HI FCS and held on ice in preparation for sorting.
The overall procedure for sorting of Lin−, Rholow/Holow cells from murine bone marrow is essentially as described by Wolf et al.15 Briefly, this procedure involved recovering lineage-depleted bone marrow cells as described above and labeling them with Rhodamine-123 and Hoechst-33342. The labeled cells were then sorted on MoFlo (Cytomation, Fort Collins, CO) cell sorter to recover the lowest 10% Rhodamine-123 staining and lowest 3% Hoechst-33342 staining cells.
Assessment of cell cycle status of engrafting stem cell.
Donor male mice were injected with 900 mg/kg hydroxyurea intravenously. Control animals received PBS intravenously. Marrow cells were harvested 3 hours after the injection, and cells were pooled separately for hydroxyurea group and control group. Forty million cells from hydroxyurea-treated mice were infused into each of 10 female recipients that were exposed to 100 cGy 4 hours previously. Forty million PBS-treated bone marrow cells were infused into each of 10 female recipients exposed to 100 cGy 4 hours previously. Mice were killed and analyzed 8 weeks posttransplantation.
Assessment of hematologic effects of minimal irradiation.
To determine the hematologic effects of low doses of irradiation on the normal host, animals in groups of five received low doses of whole animal irradiation (0, 20, 50, and 100 cGy) without donor cells. At days 2, 7, and 14, animals were killed and tissues were analyzed for white blood cell count (×103/μL), platelet count (×109/L), and marrow cellularity (×103; 2 tibias and 1 femur).
Statistical methods.
The nonparametric Kruskal-Wallis one-way rank test was used for all statistical comparisons.16 Kruskal-Wallis analysis and Cuzick two-sided test were used to evaluate engraftment trends over time.
RESULTS
Engraftment in minimally irradiated hosts.
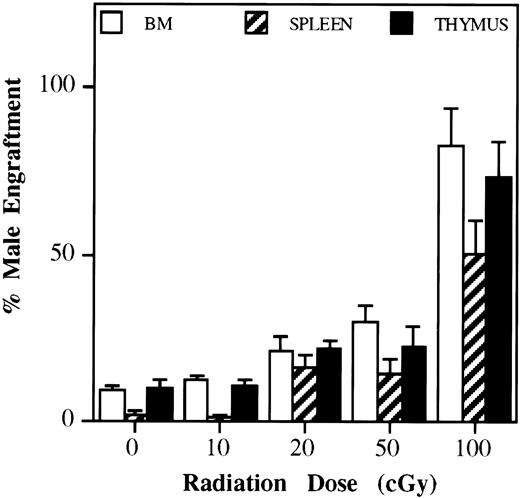
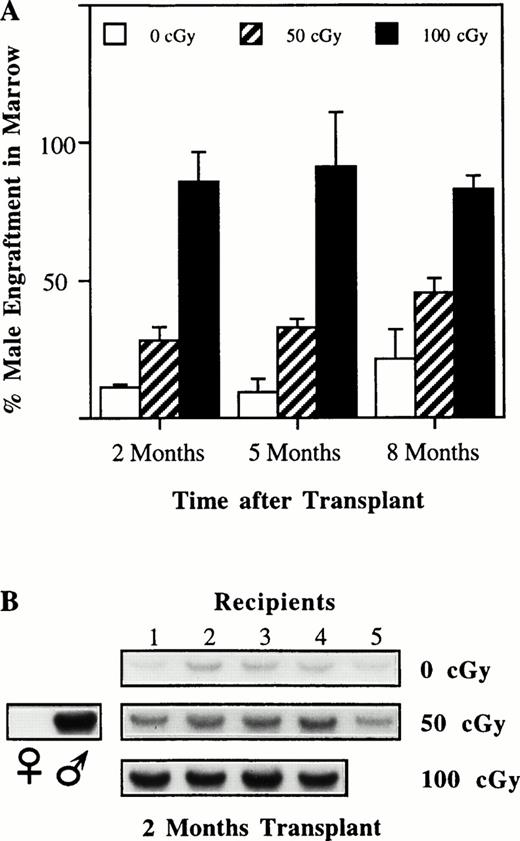
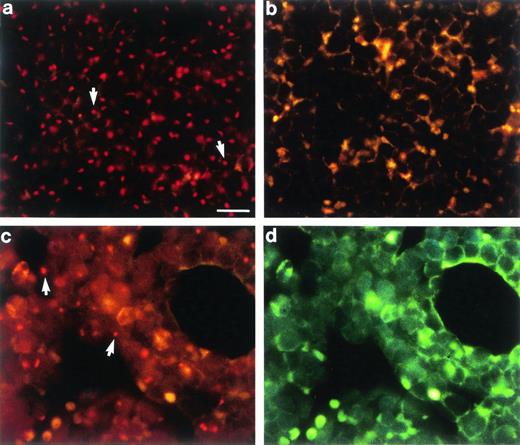
To determine if low levels of irradiation might alter competitive pressure after engraftment to favor donor cells, BALB/c female mice were treated with 0, 10, 20, 50, or 100 cGy; were infused with 40 million normal BALB/c male marrow cells; and were evaluated at 2, 5, and 8 months after marrow infusion (Figs 1and 2). Engraftment was quantitated by determining the percentage of male DNA in host marrow, spleen, and thymus using Southern blot analysis and the Y-specific pY2 DNA probe. These results indicate very high rates of male cell engraftment at 100 cGy with significant, but lower levels of engraftment seen at both 20 and 50 cGy. Engraftment was stable from 2 to 8 months after marrow infusion and in general was comparable in all three tissues analyzed. Increasing the dose of irradiation to 200 to 300 cGy did not increase engraftment at 2 months (data not shown). The high rates of engraftment seen with Southern blot analysis were confirmed with FISH on marrow sections (Fig 3).
Effect of minimal irradiation on engraftment. Balb/c female hosts received graded doses of whole animal irradiation (0, 10, 20, 50, and 100 cGy) followed 4 hours later by infusion of 40 × 106 normal Balb/c male marrow cells of the same strain in a single injection. To evaluate repopulation patterns by Southern blot analysis, we used the Y-chromosome specific pY-2 probe. Female recipient mice were killed 2 months after 0, 10, 20, 50, and 100 cGy and infusion of male marrow cells with 5 to 10 transplanted animals per dose level. A dose of 100 compared with 0 cGy showed increased engraftment in marrow, spleen, and thymus (P < .01). At 20 and 50 cGy, both bone marrow and spleen engraftment was increased compared with 0 cGy (P < .02). Compared with 50 cGy, 100 cGy produced superior engraftment in spleen, thymus, and marrow (P< .01).
Effect of minimal irradiation on engraftment. Balb/c female hosts received graded doses of whole animal irradiation (0, 10, 20, 50, and 100 cGy) followed 4 hours later by infusion of 40 × 106 normal Balb/c male marrow cells of the same strain in a single injection. To evaluate repopulation patterns by Southern blot analysis, we used the Y-chromosome specific pY-2 probe. Female recipient mice were killed 2 months after 0, 10, 20, 50, and 100 cGy and infusion of male marrow cells with 5 to 10 transplanted animals per dose level. A dose of 100 compared with 0 cGy showed increased engraftment in marrow, spleen, and thymus (P < .01). At 20 and 50 cGy, both bone marrow and spleen engraftment was increased compared with 0 cGy (P < .02). Compared with 50 cGy, 100 cGy produced superior engraftment in spleen, thymus, and marrow (P< .01).
Female recipient mice were killed at 2, 5, and 8 months after 0, 10, 50, 100 cGy. (A) Male marrow engraftment over time. (B) Southern blot showing 2-month time point. Kruskal-Wallis analysis and Cuzick two-sided test for trend over time showed that engraftment was sustained (eg, no downward trend) for bone marrow and spleen (not shown). Thymic engraftment (not shown) showed a modest decrease over time (P < .05 for all levels of irradiation).
Female recipient mice were killed at 2, 5, and 8 months after 0, 10, 50, 100 cGy. (A) Male marrow engraftment over time. (B) Southern blot showing 2-month time point. Kruskal-Wallis analysis and Cuzick two-sided test for trend over time showed that engraftment was sustained (eg, no downward trend) for bone marrow and spleen (not shown). Thymic engraftment (not shown) showed a modest decrease over time (P < .05 for all levels of irradiation).
In situ hybridization of femoral marrow sections. (a) Balb/c male control showing Y-chromosome specific signal (arrows). (b) Balb/c female control showing Y-chromosome negative cells. (c) Balb/c female transplant recipient 6 months after receiving 100 cGy and 40 × 106 Balb/c male marrow cells. (d) Same as (c) except excited with UV. The transplant resulted in 81% marrow chimerism as determined by Southern blot analysis. Arrows indicated positive marrow cells of donor origin. Scale bar for (a) through (d) = 30 μm.
In situ hybridization of femoral marrow sections. (a) Balb/c male control showing Y-chromosome specific signal (arrows). (b) Balb/c female control showing Y-chromosome negative cells. (c) Balb/c female transplant recipient 6 months after receiving 100 cGy and 40 × 106 Balb/c male marrow cells. (d) Same as (c) except excited with UV. The transplant resulted in 81% marrow chimerism as determined by Southern blot analysis. Arrows indicated positive marrow cells of donor origin. Scale bar for (a) through (d) = 30 μm.
Engraftment was present in myeloid lineages, as shown by the high percentage of chimerism seen in marrow, which is predominantly myeloid. Engraftment was also represented in lymphoid lineages, as shown by the high chimerism rates in spleen, which has greater than 90% lymphocytes (Table 1).
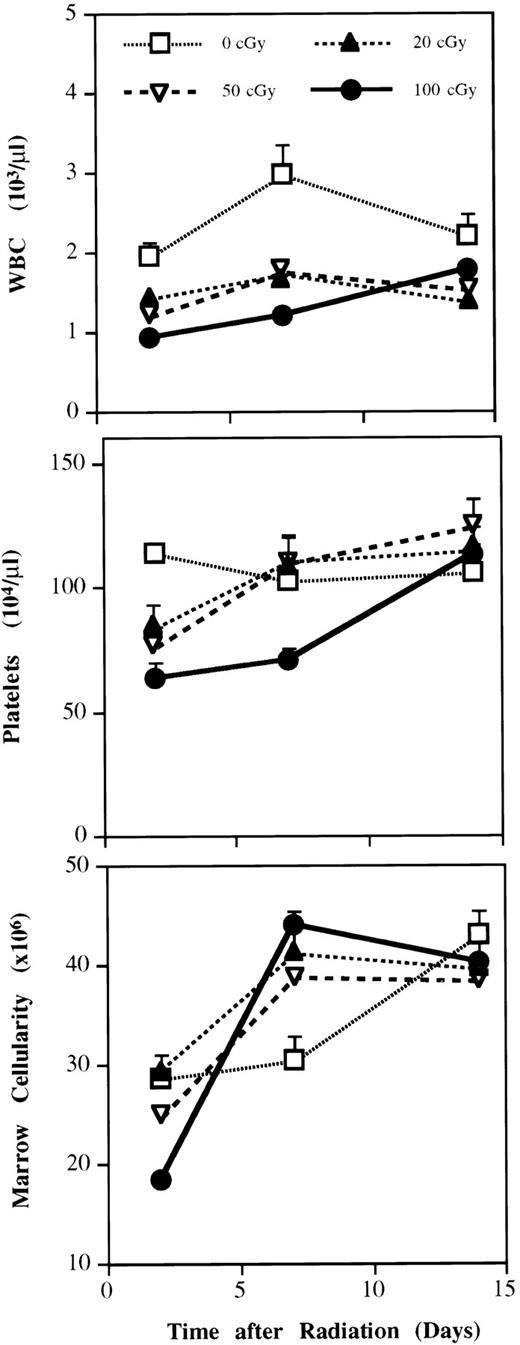
Doses of 50 to 100 cGy induced moderate and transient depression of peripheral white blood cells, platelets, and marrow cellularity (Fig 4) and no apparent toxicity.
Effect of minimal irradiation on differentiated cell levels. To determine the hematologic effects of low doses of irradiation on the normal host, animals in groups of five received low doses of whole animal irradiation (0, 20, 50, and 100 cGy) without donor cells. At days 2, 7, and 14, animals were killed and tissues were analyzed for white blood cell count (×103/μL), platelet count (×109/L), and marrow cellularity (×103; 2 tibias and 1 femur).
Effect of minimal irradiation on differentiated cell levels. To determine the hematologic effects of low doses of irradiation on the normal host, animals in groups of five received low doses of whole animal irradiation (0, 20, 50, and 100 cGy) without donor cells. At days 2, 7, and 14, animals were killed and tissues were analyzed for white blood cell count (×103/μL), platelet count (×109/L), and marrow cellularity (×103; 2 tibias and 1 femur).
Effect of cell dose on engraftment in nonablated, minimally ablated, and intensively ablated hosts.
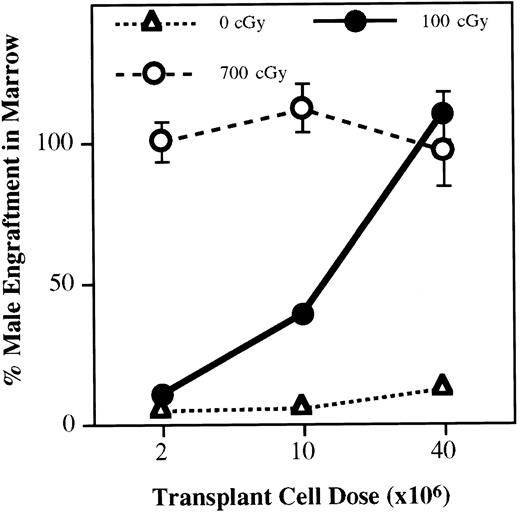
Cell dose appears to be a critical factor in determining the levels of engraftment. We assessed this effect by infusing 2, 10, or 40 million male BALB/c marrow cells into nonirradiated BALB/c female hosts or into female hosts exposed to 100 cGy or 700 cGy before marrow infusion (Fig 5). At 700 cGy, full repopulation (100% donor) was seen with 2 million cells, whereas this level of engraftment was approached with 40 million donor cells in mice exposed to 100 cGy. Ten million cells gave approximately 40% engraftment at 2 months. Although exact extrapolation is difficult, this relative level of cells (10 million) is probably less than the average human marrow harvest used for therapeutic transplantation and indicates that minimal myeloablation (100 cGy) may be feasible for clinical marrow transplantation.
Cell dose and engraftment in minimally irradiated recipients. Male marrow cells in doses of 2, 10, or 40 million cells were infused into female recipients treated with 0, 100, and 700 cGy, and the percentage of engraftment was determined after 2 months. The results show that donor cell readout in hosts after transplant is related to cell dose and irradiation dose to recipient animals. Cell doses as low as 10 million may yield up to 40% in the readout in animals receiving 100 cGy. Experimental points include 5 mice per cell level; where standard errors are not apparent, they fall within the symbol.
Cell dose and engraftment in minimally irradiated recipients. Male marrow cells in doses of 2, 10, or 40 million cells were infused into female recipients treated with 0, 100, and 700 cGy, and the percentage of engraftment was determined after 2 months. The results show that donor cell readout in hosts after transplant is related to cell dose and irradiation dose to recipient animals. Cell doses as low as 10 million may yield up to 40% in the readout in animals receiving 100 cGy. Experimental points include 5 mice per cell level; where standard errors are not apparent, they fall within the symbol.
Engraftment of purified stem cells in minimally ablated hosts.
To establish that the hematopoiesis observed at 2 months and beyond in fact was derived from stem cells and not from long-lived differentiated cell populations, such as lymphocytes or monocytes, we evaluated the capacity of marrow depleted of differentiated lineages (lin−) to engraft (Table2). We also evaluated highly purified stem cells separated on the basis of low Hoechst and Rhodamine (HoechstlowRhodaminelow) staining for their capacity to engraft in mice exposed to 100 cGy. These data show high levels of engraftment at 100 cGy, indicating that stem cells are in fact being monitored. Engraftment levels were lower than expected from the starting number of cells. The explanations for this could include loss of cells with purification, depletion of a facilitator cell population, or high rates of progenitor engraftment in the unseparated marrow.
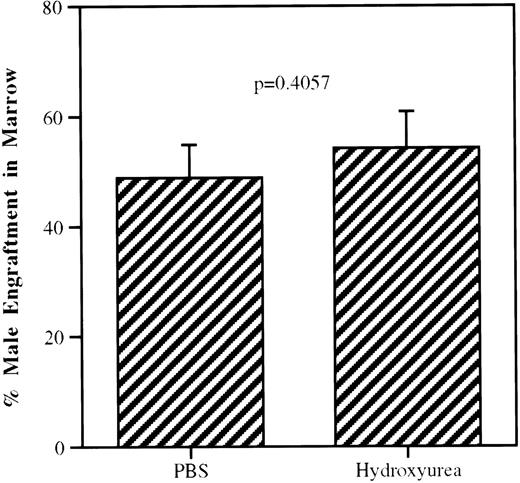
Cell cycle status of engrafting stem cell.
The cells engrafting into minimally myeloablated mice are quiescent as determined by administration of hydroxyruea or PBS to donor mice 2 hours before death (Fig 6).
Effect of hydroxyurea on donor stem cell engraftment in hosts irradiated with 100 cGy. To selectively kill cells transiting S phase, donor male BALB/c mice received an injection of 900 mg/kg hydroxyurea 3 hours before death. Mice injected with PBS constituted the control donor group. The two cell populations were infused into separate groups of irradiated (100 cGy) female hosts and the percentage of male cells in female host marrow was assessed 8 weeks after cellular infusion. Actively cycling cells will be killed by hydroxyurea and noncycling cells will be spared. The present results are from two experiments with 5 mice per experiment and show no significant differences, indicating that the engrafting cells were quiescent.
Effect of hydroxyurea on donor stem cell engraftment in hosts irradiated with 100 cGy. To selectively kill cells transiting S phase, donor male BALB/c mice received an injection of 900 mg/kg hydroxyurea 3 hours before death. Mice injected with PBS constituted the control donor group. The two cell populations were infused into separate groups of irradiated (100 cGy) female hosts and the percentage of male cells in female host marrow was assessed 8 weeks after cellular infusion. Actively cycling cells will be killed by hydroxyurea and noncycling cells will be spared. The present results are from two experiments with 5 mice per experiment and show no significant differences, indicating that the engrafting cells were quiescent.
Stem cell survival and repopulating ability after exposure to minimal irradiation in vivo or in vitro.
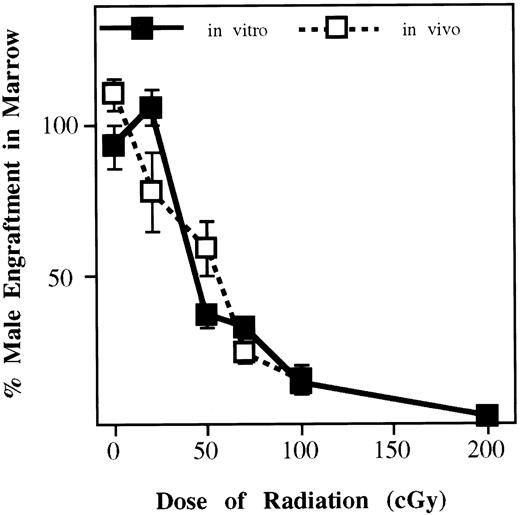
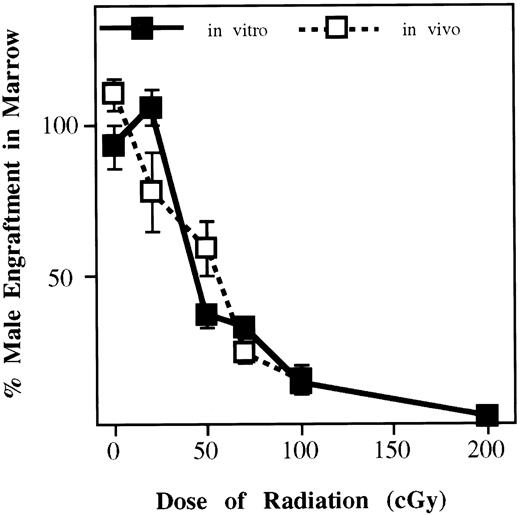
We examined the effect of in vitro or in vivo exposure to 0, 20, 50, 70, 100, or 200 cGy on the ability of 40 million BALB/c marrow cells to engraft and populate irradiated (100 cGy) female BALB/c hosts 2 months postinfusion (Fig 7). Exposure to 100 cGy, either in vitro or in vivo, reduced the populating ability to 14% of that seen with marrow that had not been exposed to irradiation.
Effect of minimal irradiation on stem cells irradiated in vivo or in vitro. Male marrow cells from BALB/c male mice were exposed to irradiation (0, 20, 50, 70, 100, and 200 cGy) in vitro and 40 × 106 was immediately infused into female recipients irradiated with 100 cGy. In another experiment, BALB/c male mice in groups of 5 were exposed to irradiation (0, 20, 50, 70, and 100 cGy), marrow cells were harvested, and 40 × 106 male marrow cells were immediately infused into female recipients irradiated with 100 cGy (groups of 5). At 2 months, the percentage of male engraftment was determined. The results show that increasing doses of minimal irradiation have a profoundly toxic effect on stem cells irradiated in vitro or in vivo.
Effect of minimal irradiation on stem cells irradiated in vivo or in vitro. Male marrow cells from BALB/c male mice were exposed to irradiation (0, 20, 50, 70, 100, and 200 cGy) in vitro and 40 × 106 was immediately infused into female recipients irradiated with 100 cGy. In another experiment, BALB/c male mice in groups of 5 were exposed to irradiation (0, 20, 50, 70, and 100 cGy), marrow cells were harvested, and 40 × 106 male marrow cells were immediately infused into female recipients irradiated with 100 cGy (groups of 5). At 2 months, the percentage of male engraftment was determined. The results show that increasing doses of minimal irradiation have a profoundly toxic effect on stem cells irradiated in vitro or in vivo.
DISCUSSION
Previous dogma suggested that irradiation facilitated engraftment by opening space. As noted above, the studies of engraftment in nonmyeloablated hosts have challenged this concept. Only a few studies have compared engraftment of marrow stem cells in mice subjected to low dose irradiation with that seen in mice receiving no irradiation. These studies used higher levels of irradiation or showed only minimal engraftment.17,18 Shirot and Tavassoli19evaluated mice treated with 100 to 2,000 cGy and studied perfusion-fixed marrow by transmission electron microscopy. They showed sloughing and denudation of plasma membranes on the luminal side of the endothelium in irradiated mice. Other changes, predominately noted with doses of greater than 250 cGy, included membrane vesiculation, dilatation of the perinuclear space and rough endoplasmic reticulum, focal cytoplasmic swelling of endothelium, and bleeding into the marrow space. Although injury was apparent in mice exposed to 100 cGy, this appeared to heal quickly. At 1,000 cGy, cellular disruption was irreversible. Work by Hendrikx et al20 using purified stem cells labeled with the fluorescent membrane stain PKH-26 and engrafted into lethally irradiated mice or nonirradiated mice indicated that homing to nonirradiated marrow was 2.5 times higher than to irradiated bone marrow, suggesting a deleterious effect on engraftment of stem cells by high levels of host irradiation.
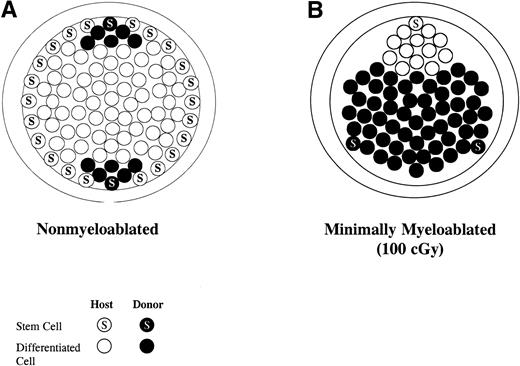
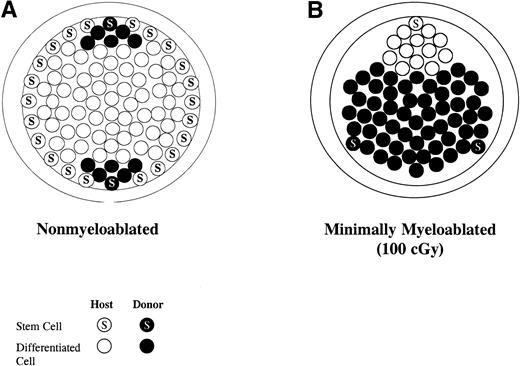
Although the low levels of irradiation used here could be physically opening space, the minimal effect on total marrow cellularity, the high levels of stem cell engraftment seen in nonmyeloablated mice,21-24 and the above-noted homing studies all argue against this mechanism. Our previous data suggest that the final host:donor ratios might be determined by competition between host and donor stem cells. To test this directly, we examined the effect of in vitro or in vivo exposure to 0, 20, 50, 70, 100, or 200 cGy on the ability of 40 million BALB/c marrow cells to engraft and populate irradiated (100 cGy) female BALB/c hosts 2 months postinfusion (Fig 6). Exposure to 100 cGy, either in vitro or in vivo, reduced populating ability to 14% of that seen with marrow that had not been exposed to irradiation. This level of host stem cell reduction, either by death or alteration in function, coupled with the infusion of 40 million marrow cells (in a host presumed to have approximately 300 million total marrow cells), could explain the high levels of donor cell chimerism on a simple stem cell competition model (Fig8). These data indicated that engraftment at the stem cell level is very efficient in minimally myeloablated mice and that the final donor:host ratios are determined by competition between host and donor stem cells. It is possible that the majority of donor cells are radiosensitive but that there is a population existing of relatively radioresistant cells. Minimal myeloablation, in concert with clinically obtainable stem cell numbers, provides an approach to gene therapy or for the creation of allochimeras in such diseases as sickle cell anemia or thalassemia, which should be both effective and nontoxic. In addition, this approach, with appropriate immunosuppression, may allow for the creation of allochimeras in cellular immunotherapy strategies for the treatment of cancer.
Model of competitive stem cell engraftment into (A) normal (nonirradiated host) and (B) minimally irradiated host (100 cGy).
Model of competitive stem cell engraftment into (A) normal (nonirradiated host) and (B) minimally irradiated host (100 cGy).
P.J.Q. was supported by grants from the National Institutes of Diabetes and Digestive and Kidney Diseases (P0-1 DK 50222-01, R0-1 DK 49650-03, and R0-1 DK 27424-15) and the National Heart, Lung and Blood Institute (P0-1 HL 56920-01). F.M.S. was supported by a grant from the Leukemia Society of America (New York, NY; Grant No. 6207). J.W. and C.-c.H. were supported in part by a grant from the Howard Hughes Medical Institute (HHMI Grant No. 76296-550401).
Address reprint requests to F.M. Stewart, MD, Division of Hematology/Oncology, University of Massachusetts Medical Center, 55 Lake Ave N, Worcester, MA 01655.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.