Abstract
A novel BβAsn-160 (TAA) to Ser (TGA) substitution has been identified in fibrinogen Niigata derived from a 64-year-old asymptomatic woman, who is heterozygotic for this abnormality. The mutation creates an Asn-X-Ser–type glycosylation sequence, and a partially sialylated biantennary oligosaccharide was linked to the BβAsn-158 residue. The functional abnormality was attributed to delayed lateral association of normally formed double-stranded protofibrils based on normal cross-linking of fibrin γ-chains and tissue-type plasminogen activator-catalyzed plasmin generation by polymerizing fibrin monomers. Enzymatic removal of all the N-linked oligosaccharides from fibrinogen Niigata accelerated fibrin monomer polymerization that reached the level of untreated normal fibrin monomers, but the thrombin time was prolonged from 18.2 seconds to 113 seconds (normal: 11.2 seconds to 8.9 seconds). By scanning electron micrographic analysis, Niigata fibrin fibers were found to be more curvilinear than normal fibrin fibers. After deglycosylation, Niigata fibers became straight being similar to untreated normal fibrin fibers, whereas normal deglycosylated fibrin appeared to be less-branched than untreated normal or deglycosylated Niigata fibrin. Although normal and Niigata fibrins were similar to each other in permeation and compaction studies, deglycosylated normal and Niigata fibrins had much higher permeability and compaction values, indicating that deglycosylation had brought about the formation of more porous networks. The enzymatic deglycosylation necessitates an Asn to Asp change at position Bβ-158 that is responsible for reducing the fiber thickness because of either local repulsive forces or steric hindrance in the coiled-coil region.
FIBRINOGEN IS a glycoprotein composed of 3 pairs of nonidentical chains (Aα, Bβ, γ)2 with a combined molecular weight of 340,000. It contains approximately 3% carbohydrate consisting of Asn-linked biantennary oligosaccharide skeletons with different amounts of sialic acid linked to their terminal galactose residues.1,2 The major component is a monosialylated oligosaccharide accounting for about 62% followed by a disialylated oligosaccharide accounting for 22%.1-4 The oligosaccharide chains are normally linked to Asn-364 of the Bβ chain5and Asn-52 of the γ-chain.6 There are 2 other potential N-glycosylation sequences on the Aα chain, but they are not linked with oligosaccharide moieties because of the presence of neighboring Pro residues.7 No O-linked oligosaccharides have been identified in any subunits of human fibrinogen.
Five hereditary dysfibrinogens with an amino acid substitution that generates an Asn-X-Ser/Thr type sequence have been reported to have an extra oligosaccharide at an Asn residue with the same biantennary structures found in normal fibrinogen.3,4,8-10 Such an extra oligosaccharide has been identified in fibrinogen Pontoise at Bβ Asn-333,8 Asahi at γ Asn-308,9 Lima at Aα Asn-139,4 Caracas II at Aα Asn-434,3 and Kaiserslautern at γ Asn-380.10 In the last 3 fibrinogens, the major component was a disialylated oligosaccharide accounting for 68.6%, 81.9%, and 95%, respectively.
The role of carbohydrate in fibrinogen function has not been clarified as yet, but carbohydrate is proposed to be involved in the regulation of fibrin assembly by contributing a repulsive force to form stable fibrin networks.11 Indeed, all the extra-glycosylated dysfibrinogens manifest altered fibrin assembly at various stages of fibrin network formation. Electron microscopic analysis of the Caracas II fibrin showed that the fibrin networks were made up of thinner and less ordered fibers than normal control and retained normal stiffness, although permeability of the clots increased.12 These data were consistent with biochemical analysis data.3
In this paper, we describe a dysfibrinogen, designated as fibrinogen Niigata, associated with an extra oligosaccharide unit at Asn-158 on the Bβ-chain. The study involves ultrastructural analysis of fibrinogen Niigata and its fibrin structure, mainly focusing on the evaluation of the extra oligosaccharide in the molecule.
MATERIALS AND METHODS
Fibrinogen was purified from normal and patient citrated plasma, and human α-thrombin was prepared from prothrombin essentially as described previously.13 14 Recombinant 2-chain tissue-plasminogen activator (t-PA) was prepared from myeloma cells. The following enzymes were purchased: human α-thrombin used in the permeation and compaction experiments was from Enzyme Research Laboratories (South Bend, IL); lysylendopeptidase from Wako Chemical Co (Osaka, Japan); almond glycopeptidase from Seikagaku Kogyo (Tokyo, Japan); and recombinant N-Glycosidase F from Boehringer Mannheim Biochemica (Mannheim, Germany). The following HPLC columns were used: phenyl-5PW-RP and TSK-Gel Amide-80 from Tosoh (Tokyo, Japan); Cosmosil 5C18P from Nakalai Chemicals Ltd (Kyoto, Japan); and Shimpack CLC-ODS from Shimadzu (Kyoto, Japan).
Description of the patient.
A 64-year-old woman was suspected of having a dysfibrinogenemia based on coagulation studies conducted before surgery for a urinary bladder tumor. Namely, there was a marked discrepancy between fibrinogen levels in plasma determined by 2 assays: less than 50 mg/100 mL by a thrombin time method and 412 mg/100 mL by a turbidimetric method, where the heat-denatured (56°C, 10 minutes) fibrinogen in 30-fold diluted plasma with 0.5% EDTA in 0.9% NaCl was quantified at 660 nm by using a calibration curve with normal pooled plasma. The one-stage prothrombin time (PT) and the activated partial thromboplastin time (aPTT) were both in the normal ranges. The patient underwent surgery without any excessive bleeding or postoperative thrombosis despite this abnormality. Her son displayed the same type of coagulation abnormalities but no history of bleeding or thrombotic tendencies.
Studies on purified fibrinogen.
Coagulation studies were performed according to standard procedures. When the Niigata fibrinogen was clotted with α-thrombin (1.0 NIH U/mL), the fibrin clot remained transparent over 1 hour of incubation but became turbid with further elapse of time. Aggregation studies of preformed and acid-solubilized fibrin monomer and the enhancement of t-PA–catalyzed activation of plasminogen by the polymerizing fibrin monomer were performed essentially as described previously.15
Factor XIIIa-catalyzed cross-linking of fibrin.
The Niigata fibrinogen (0.5 mg/mL) was clotted at 25°C with α-thrombin (1.0 NIH U/mL) and factor XIII (1.25 U/mL) in 32 μL of TBS containing 5 mmol/L CaCl2. At timed intervals, 0.6 μL of 0.2 mol/L ethylendiaminetetraacetate-Na2 (EDTA) was added and the clots were immediately dissolved in a reducing sodium dodecylsulfate-polyacrylamide gel electrophoresis (SDS-PAGE) solution (1.5 mol/L Tris-HCl, pH 8.8 containing 3% SDS, 8 mmol/L dithiothreitol, 2 mmol/L EDTA, and 8 mol/L urea) and subjected to PAGE analysis.
Lysylendopeptidase mapping of the fibrinogen Bβ-chain.
The 3 subunits of fibrinogen were separated after reduction and S-pyridylethylation by high performance liquid chromatography (HPLC) using a TSK gel Phenyl-5PW-RP column (4.6 × 75 mm). They were eluted in the order of Aα, Bβ, and γ chains with a linear gradient (40 minutes) from 30% to 40% acetonitrile. The Niigata Bβ chain was eluted in 2 partially separated peaks, namely, when the gradient was withheld while the Aα-chain was being eluted; they were separated into 2 peaks with a ratio of about 1:1 (calculated from peak areas). For better estimation of the ratio of normal (Bβ) and abnormal (Bβ′) peptide in peptide mapping experiments, the 2 peaks were combined as the pyridylethylated (PE)-Niigata Bβ-chain. The PE-Niigata Bβ-chain (0.1 mg/mL, 130 μg) was digested with lysylendopeptidase (E/S = 1/50, w/w) at 37°C for 18 hours in 50 mmol/L Tris-HCl, pH 9.0 containing 3 mol/L urea and analyzed by HPLC on a column of Cosmosil 5C18P (4.6 × 150 mm) using a linear gradient elution from 0% to 40% acetonitrile in 100 minutes.
Amino acid composition and sequence analysis.
The amino acid compositions of fibrinopeptides A, AY, and B were analyzed with an amino acid analyzer, Derivatizer, model 420H (PE-Biosystems, Foster City, CA). The amino acid sequence analyses of 3 peptides, Niigata K47, Niigata K49 and normal K48 (see Fig 2 in Results) were conducted by using a 20% to 25% volume of each fraction with a Protein Sequencer, model 476A (PE-Applied Biosystems).
Analysis of N-linked oligosaccharide moieties by 3-dimensional mapping.
About 1 nmol of Niigata K-47 was double digested with almond glycopeptidase A and thermolysin to liberate the oligosaccharide moieties. The oligosaccharide moieties were purified by HPLC on an anion-exchange column, and then modified to pyridylaminated (PA)-oligosaccharide as described previously.3,4 The PA-oligosaccharide was injected onto an ODS-silica column for identification by a 3-dimensional mapping technique as described previously.16
Enzymatic elimination of N-linked oligosaccharides in fibrinogen.
To eliminate N-linked oligosaccharide from fibrinogen, we selected Glycosidase F as a cleaving enzyme because it is known to function under a neutral pH and nondenaturing conditions. Fibrinogen (10 mg/mL) was incubated with 4 units of Glycosidase F in a 120 μL of 10 mmol/L Tris-HCl, pH 7.4, containing 0.15 mol/L NaCl (TBS) at 37°C for 24 hours. After this incubation, most of the N-linked oligosaccharides from the Bβ, Bβ′, and γ chains were removed as evidenced by SDS-PAGE. Removal of oligosaccharide moieties was confirmed also by agarose gel electrophoresis, in which both enzyme-treated normal and Niigata fibrinogens migrated to more anodal regions than the intact molecules (data not shown). The fibrinogens thus prepared were subjected to functional analyses including clotting, aggregation of fibrin monomer, permeation and compaction studies.
Nucleotide sequencing of exon IV of the fibrinogen Bβ-chain gene.
The DNA fragment coding exon IV of the fibrinogen Bβ-chain gene was amplified by polymerase chain reaction (PCR) using a synthesized primer, BF4, corresponding to nucleotides 4872-4896 in intron 3 (TATATGTCATGCGCCAAATCATTTC), and a 100-fold excess of primer B4R (GGTGTGTGAGTTCTTCTGGAACTCT), corresponding to the complementary sequence of nucleotides 5298-5322 in intron 4 of the fibrinogen Bβ-chain gene. The DNA product obtained consisted mostly of a single-strand DNA fragment with the primer B4R-derived fragment on its 5′ end, and was directly sequenced using Sequenase (Amersham, Arlington Heights, IL), 35S-dATP (Amersham) and primer B4F essentially according to Gyllensten and Erlich.17
Permeation studies.
Permeability measurements were performed according to the methods of Nair and Dhall,18 with a slight modification. Fibrin networks with a height of approximately 4 cm were formed in polystyrene tubes (4 mm in diameter), which had been precoated with fibrinogen at 1 mg/mL and air-dried before use. Clotting was initiated in a separate tube with a mixture of fibrinogen (2 mg/mL) and thrombin (0.05 NIH U/mL) in TBS, and the mixture was immediately transferred to another tube and incubated overnight at 22°C. Before the measurement of flow rate, irregularities or defects in fibrin network formation (ie, channeling) were examined by passing a solution of fuchsin basic. Permeation experiments were performed with pressure gradients of 2- to 3-fold clot height, and pressure was kept constant during the experiment. Flow rate was determined by measurements of the volume of liquid eluted over a fixed period of time. After the rate determinations, channeling along the walls or other irregularities of flow through the gels were again examined by passing a solution of fuchsin basic.
The permeability constant (τ) was determined from Darcy’s law:
where “Q/t” is the flow rate; “η,” the relative viscosity of the buffer; “h,” the length of the clot; “F,” its cross-sectional area and “p,” the applied pressure.
Compaction studies.
Compaction experiments were performed by a minor modification of a previously described method.19 Conical microfuge tubes were precoated with cooking oil and dried with a cotton swab. The fibrin matrix was formed in these tubes with 0.60 mg/mL fibrinogen, 0.06 NIH U/mL thrombin in TBS. After incubation at 25°C for 2 hours, the tubes were centrifuged at 4200g for 30 seconds and the volume of the expelled buffer was withdrawn and measured with a Hamilton syringe (Hamilton Co, Reno, NV). Percentage compaction was expressed as the ratio of the expressed volume to the original volume (0.75 mL) of the clot.
Specimen preparation for electron microscopy.
For examination of fibrin by scanning electron microscopy (SEM), fibrin was formed on carbon-formvar coated gold grids in 50 mmol/L Tris-HCl, pH 7.4, containing 0.1 mol/L NaCl and 0.1 U/mL thrombin. Clots were incubated for 3 hours in a humidity chamber, then fixed with 2.5% glutaraldehyde in 0.1 mol/L Hepes buffer, pH 7 containing 0.2% tannic acid, washed several times with Hepes buffer, dehydrated in graded ethanol solutions, CO2 critical point dried, and sputter-coated with platinum-gold. SEM was performed in a JEOL JSM6300F Field Emission Scanning Electron Microscope (Japan Electron Optics Laboratory, Tokyo, Japan). Samples of fibrinogen for transmission electron microscopy (TEM) were formed from stock solutions of 1 mg/mL or higher in 30% glycerol, containing 0.15 mol/L ammonium acetate, pH 7 buffer, diluted to 30 μg/mL in the above buffer, sprayed onto freshly cleaved mica sheets, rotary shadowed with platinum-carbon, and then examined in a Philips 400 electron microscope (Philips, Amsterdam, The Netherlands).
RESULTS
Abnormality of purified fibrinogen Niigata.
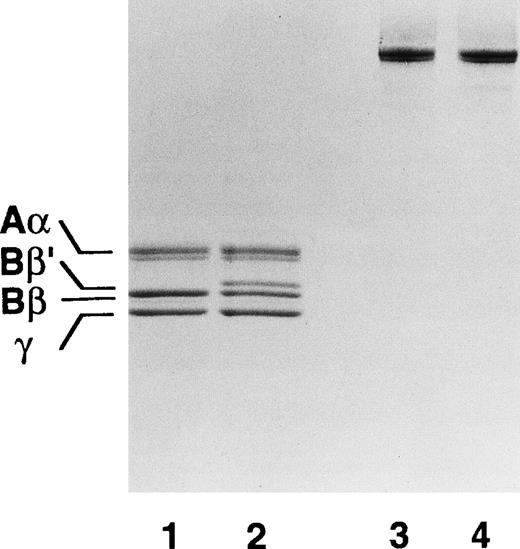
The patient-derived purified fibrinogen has 2 species of the Bβ chain denoted as Bβ′ and Bβ as evidenced by SDS-PAGE (Fig1). The Bβ chain species corresponded to the normal Bβ chain, whereas the Bβ′ chain species was found to have a molecular weight higher by about 3,000 as compared with the normal Bβ chain. The Aα and γ chains appeared to be normal.
Subunit polypeptides of purified fibrinogen Niigata examined by SDS-PAGE. To each lane 1.5 μg of protein was loaded on 7.5% to 12.5% gradient gel under the reducing (lanes 1 and 2) or nonreducing (lanes 3 and 4) conditions and the proteins were stained with Coomassie Brilliant Blue R250. Lanes 1 and 3 are normal fibrinogen and lanes 2 and 4 are patient’s fibrinogen.
Subunit polypeptides of purified fibrinogen Niigata examined by SDS-PAGE. To each lane 1.5 μg of protein was loaded on 7.5% to 12.5% gradient gel under the reducing (lanes 1 and 2) or nonreducing (lanes 3 and 4) conditions and the proteins were stained with Coomassie Brilliant Blue R250. Lanes 1 and 3 are normal fibrinogen and lanes 2 and 4 are patient’s fibrinogen.
The thrombin time of fibrinogen Niigata was 18.4 seconds (control, 11.8 seconds) and the addition of Ca2+ corrected it partially (14.8 seconds; control, 10.8 seconds). Profiles of α-thrombin–released fibrinopeptides A and B were indistinguishable from those for normal as evidenced by SDS-PAGE and HPLC elution profiles, and both peptides were normal as assessed by amino acid composition analysis (data not shown).
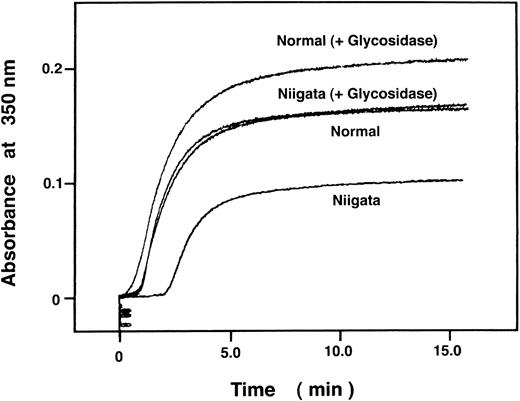
In the absence of Ca2+, fibrinogen Niigata formed at first a transparent clot on incubation with thrombin, which then gradually transformed to a turbid clot. The aggregation profile of Niigata fibrin monomer disclosed an elongated lag phase, a normal increase in turbidity and low maximum amplitude as compared with normal control (Fig 2). In the presence of Ca2+, a turbid clot was formed as a normal fibrin clot, which was expected from the normal aggregation profile of Niigata fibrin in the presence of Ca2+. Because the Niigata fibrin monomer manifested almost normal enhancement of t-PA–mediated plasminogen activation (data not shown), and the factor XIIIa-catalyzed cross-linking of the γ-chain took place in a normal fashion (data not shown), double-stranded protofibrils may have been constructed normally via a set of ‘A’-‘a’ polymerization sites.
Aggregation profiles of acid-solubilized fibrin monomers derived from normal, DG-normal, Niigata, and DG-Niigata fibrinogen. Aggregation of acid-solubilized fibrin monomer was studied by monitoring absorbance at 350 nm. Each fibrin monomer was prepared as described in Materials and Methods. DG-normal and Niigata fibrin monomer were expressed as Normal (+Glycosidase) and Niigata (+Glycosidase).
Aggregation profiles of acid-solubilized fibrin monomers derived from normal, DG-normal, Niigata, and DG-Niigata fibrinogen. Aggregation of acid-solubilized fibrin monomer was studied by monitoring absorbance at 350 nm. Each fibrin monomer was prepared as described in Materials and Methods. DG-normal and Niigata fibrin monomer were expressed as Normal (+Glycosidase) and Niigata (+Glycosidase).
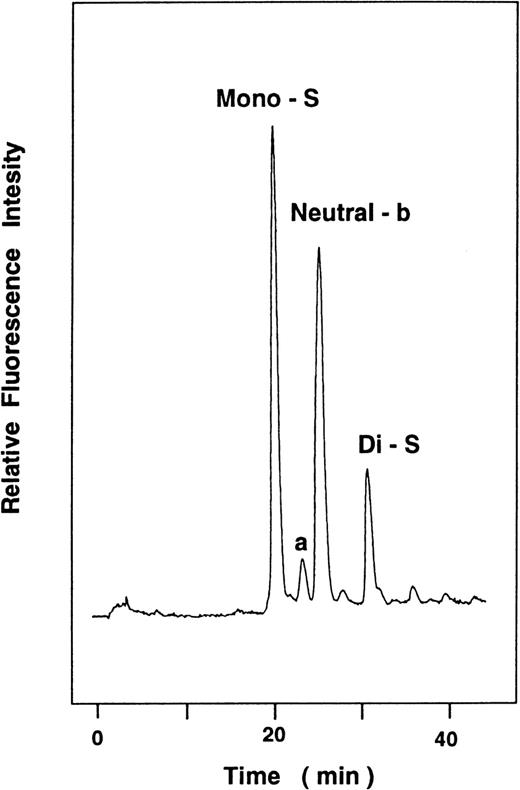
Identification of an aberrant peptide in lysylendopeptidase digests of the PE-Bβ-chain.
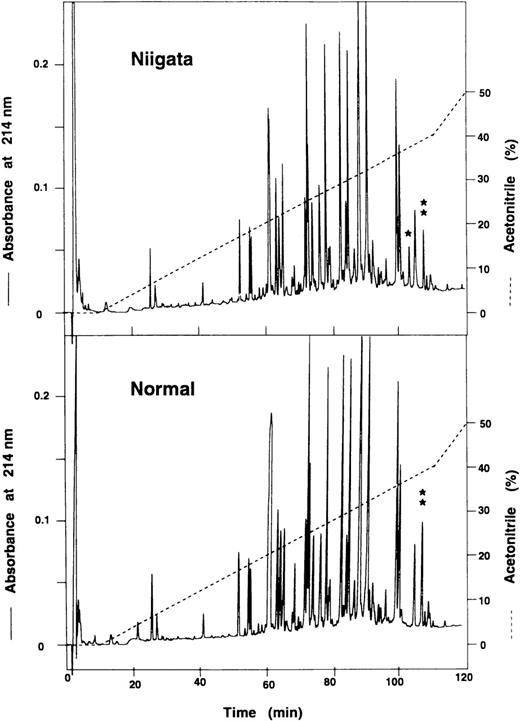
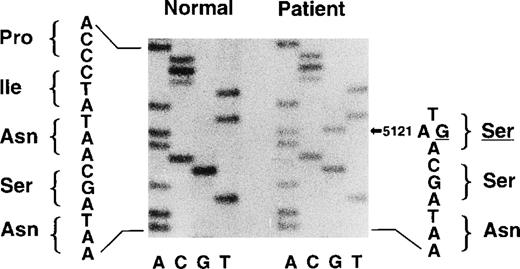
In the mapping profile of the lysylendopeptidase digests of PE-Bβ chain derived from the patient’s and normal fibrinogen, there was an aberrant peptide peak in the patient’s PE-Bβ digests (Fig3, upper panel), denoted as K47, which was not present in the normal PE-Bβ digests (Fig 3, lower panel). On the other hand, the peptide peak denoted as K49 in the patient’s PE-Bβ digests was apparently smaller than the normal counterpart (K48) in the normal PE-Bβ digests. Niigata K47 and K49 and normal K48 were found to compose the Bβ (149-178) segment by amino acid sequence analysis. The amino acid sequence of Niigata K47 was identical with that of Niigata K49 except at cycles 10 and 12 (Table1). At cycle 10 (position 158), no PTH-amino acid derivative was identified, because the solvent system used in the protein sequencer could not extract the sugar-attached PTH-Asn. At cycle 12, (position 160), Ser was identified instead of Asn. The amino acid substitution was verified by analysis of the nucleotide sequence of PCR-amplified exon-IV of the fibrinogen Bβ-chain gene derived from the patient, in which adenine (A) at position 5121 had been replaced by guanine (G), thus constructing a codon TGA coding for Ser instead of Asn at position 160 of the Bβ-chain (Fig 4). This mutation created an Asn-X-Ser–type consensus sequence for N-glycosylation of the Asn residue in this region. Indeed, we isolated oligosaccharide moieties from Niigata K47 as anticipated and identified their structure by the 3-dimensional oligosaccharide mapping technique (Fig5). The purified oligosaccharides were mixtures of 4 kinds of biantennary skeleton oligosaccharides with or without sialic acid linked to their terminal galactose residues. The major component was monosialyl oligosaccharides (Mono-S) accounting for 47%, followed by neutral oligosaccharides (Neutral-a and Neutral-b) and disialyl oligosaccharides (Di-S) accounting for 39% and 13%, respectively (Table 2). The content of neutral oligosacharides in K47 was higher than those found in the extra oligosaccharide units in fibrinogens Lima, Caracas II, and Kaiserslautern, where at much higher rates the oligosaccharides were disialylated.3,4 10 The structures of the extra oligosaccharides are shown in Table 2.
HPLC profile of lysylendopeptidase digests of Bβ-chain. The lysylendopeptidase digests of PE-Bβ chains derived from normal fibrinogen and fibrinogen Niigata were injected on to a Cosmosil 5C18P column (4.6 × 150 nm), and the peptides were eluted with a linear gradient from 0% to 40% acetonitril in 100 minutes. Three peaks, Niigata K47 (*), Niigata K49 (**), and normal K48 (**), were collected and subjected to N-terminal amino acid sequence analysis.
HPLC profile of lysylendopeptidase digests of Bβ-chain. The lysylendopeptidase digests of PE-Bβ chains derived from normal fibrinogen and fibrinogen Niigata were injected on to a Cosmosil 5C18P column (4.6 × 150 nm), and the peptides were eluted with a linear gradient from 0% to 40% acetonitril in 100 minutes. Three peaks, Niigata K47 (*), Niigata K49 (**), and normal K48 (**), were collected and subjected to N-terminal amino acid sequence analysis.
Direct nucleotide sequencing of PCR-amplified exon IV of the patient-derived fibrinogen Bβ-chain gene. The DNA sample of PCR-amplified exon of patient’s fibrinogen Bβ-chain gene was subjected to urea-PAGE and subsequently to autoradiography. Part of the autoradiogram is shown. The arrow indicates the mutation of G for A at position 5121, coding Ser (TGA) for Asn (TAA) at position 160 of the fibrinogen β chain.
Direct nucleotide sequencing of PCR-amplified exon IV of the patient-derived fibrinogen Bβ-chain gene. The DNA sample of PCR-amplified exon of patient’s fibrinogen Bβ-chain gene was subjected to urea-PAGE and subsequently to autoradiography. Part of the autoradiogram is shown. The arrow indicates the mutation of G for A at position 5121, coding Ser (TGA) for Asn (TAA) at position 160 of the fibrinogen β chain.
Analysis of PA-oligosaccharides derived from Niigata K47 peptide by HPLC on an octadecylsilyl (ODS)-silica column. The Niigata peptide was double digested with glycopeptidase from almond and thermolysin to form the oligosaccharides. The oligosaccharides were purified by HPLC on a column of DEAE column and then subjected to aminopyridylation. The PA-oligosaccharides were injected to an ODS column for the identification by 3-dimensional mapping technique. From the 3-D elution mapping chart, the Niigata K47 peptide was found to contain 2 kinds of biantennary neutral oligosaccharides (Neutral-a and Neutral-b) and biantennary sialyl oligosaccharides (Mono-S and Di-S), respectively.
Analysis of PA-oligosaccharides derived from Niigata K47 peptide by HPLC on an octadecylsilyl (ODS)-silica column. The Niigata peptide was double digested with glycopeptidase from almond and thermolysin to form the oligosaccharides. The oligosaccharides were purified by HPLC on a column of DEAE column and then subjected to aminopyridylation. The PA-oligosaccharides were injected to an ODS column for the identification by 3-dimensional mapping technique. From the 3-D elution mapping chart, the Niigata K47 peptide was found to contain 2 kinds of biantennary neutral oligosaccharides (Neutral-a and Neutral-b) and biantennary sialyl oligosaccharides (Mono-S and Di-S), respectively.
Effect of removal of extra oligosaccharides on the fibrin clot formation.
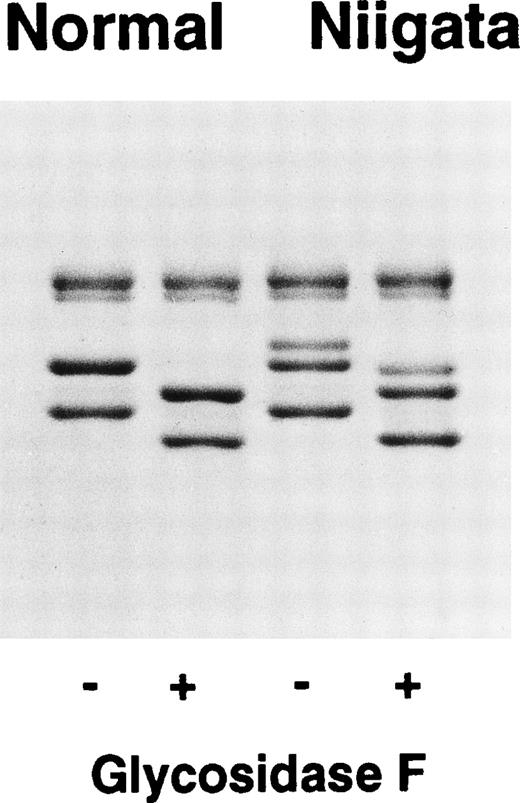
We prepared deglycosylated (DG)-Niigata fibrinogen to clarify the effect of extra oligosaccharides on the clot formation. Incubation of fibrinogens with Glycosidase F resulted in the decrease of relative molecular masses of the Bβ and γ-chains of normal and Niigata fibrinogens by about 4,000 (Fig 6), which was consistent with the oligosaccharide moiety at Asn-364 and Asn-52 of normal fibrinogen, respectively. It is notable that 2 Bβ-chain bands were detected in Niigata fibrinogen on Laemmli’s SDS-PAGE even after the removal of all N-linked oligosaccharides. This molecular difference may be because of the presence of newly formed Asp-158 in the variant Bβ-chain, because such alterations in electrophoretic mobility have been described in a variety of proteins with a single point mutation including congenital dysfibrinogens.20-23 These data also suggest that there is a distinct structural difference between the 2 DG-fibrinogen molecules. Indeed, a significant difference in the thrombin clotting of these DG-fibrinogens was observed (Table3). DG-normal fibrinogen had a slightly shortened thrombin time (11.3 seconds to 8.9 seconds) and formed a highly turbid clot as compared with intact normal fibrinogen. These results were in agreement with those of Langer et al.11 On the other hand, DG-Niigata fibrinogen had a markedly prolonged thrombin time (18.4 seconds to 113 seconds) as compared with intact Niigata fibrinogen. Furthermore, DG-Niigata fibrinogen initially formed a transparent fibrin clot, but its turbidity increased rather rapidly as compared with untreated Niigata fibrinogen. The transformation from the transparent clot to the turbid clot seemed to be accelerated by the removal of oligosaccharide moieties from Niigata fibrinogen.
Removal of N-linked oligosaccharides from Bβ and γ chains of fibrinogen. Fibrinogen (10 mg/mL) was incubated with Glycosidase F (45 U/mL) or without enzymes at 37°C for 24 hours in TBS and then subjected to SDS-PAGE analysis.
Removal of N-linked oligosaccharides from Bβ and γ chains of fibrinogen. Fibrinogen (10 mg/mL) was incubated with Glycosidase F (45 U/mL) or without enzymes at 37°C for 24 hours in TBS and then subjected to SDS-PAGE analysis.
In aggregation experiments, DG-normal and Niigata fibrin monomers manifested a much shorter lag-time and a greater amplitude, though the turbidity of DG-Niigata fibrin monomer did not reach the level of DG-normal fibrin monomer (Fig 2). In the case of DG-Niigata fibrin monomer, the aggregation profile seemed to be almost identical with that of intact normal fibrin monomer.
Compaction and permeation studies.
Normal and Niigata fibrin had similar compactability, although their deglycosylated counterparts were more easily compacted (Table4), indicating that DG-fibrin networks have thicker fibers and larger pore sizes. DG-normal fibrin was considerably more compactible than DG-Niigata fibrin (P = .005), a finding that is consistent with the appearance of SEM images (see the following).
Results of permeation studies were less satisfactory, especially with respect to DG-fibrin values. The permeation values for normal and Niigata fibrin were in the same range and did not differ significantly from each other (P = .22). However, DG-fibrin, either normal or Niigata, tended to separate from the walls of the permeation tube. Permeation constants for those clots that did adhere adequately were considerably higher than those for the non-DG fibrin and the values covered a wide range (10 to 105 ×10−9 cm2, n = 10). This observation suggested that although there was no gross evidence for channeling, this was indeed occurring. Thus, apart from the high permeation constant, which was largely reflective of the high porosity observed in SEM experiments and detected by compactability, we did not use these values for quantitative determinations in Table4.
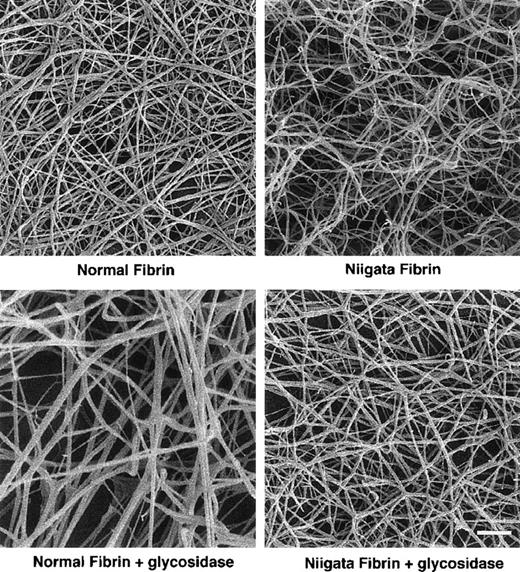
SEM of Niigata and its DG-fibrin clots.
SEM images of normal fibrin showed a typical matrix composed of thick elongated branching fibers (Fig 7). After treatment of normal fibrinogen with glycosidase, the resulting fibrin fibers were thicker than untreated fibrin fibers, yielding a network with greater porosity than normal fibrin, consistent with compaction and permeation measurements.
SEM image of fibrin derived from normal and Niigata and their DG-fibrins. Bar, 10 μm.
SEM image of fibrin derived from normal and Niigata and their DG-fibrins. Bar, 10 μm.
The Niigata fibrin matrix was similar to that of normal in that the fiber widths were about the same, but differed from normal in subtle ways. Most prominently, Niigata fibers were more curvilinear than those of normal fibrin. A sense of the porosity of this matrix relative to normal could not be gained from simply observing the overall network structure. After glycosidase treatment, the Niigata fibers became straighter and the general appearance was similar to those of untreated normal fibrin. There was a general sense that the porosity of this network was greater than those of normal or untreated Niigata fibrin, and this impression was confirmed by permeation and compaction experiments.
Examination of a rotary-shadowed preparation of fibrinogen Niigata showed trinodular molecules that did not differ in any recognizable way from normal fibrinogen molecules (data not shown).
DISCUSSION
Abnormal fibrinogens with extra oligosaccharides are occasionally endowed with strong negative electric charges. Thus, when they are converted to fibrin, extra repulsive forces may arise and affect lateral association of normally constructed fibrin protofibrils and fiber packing. In fact, such phenomena have been observed in fibrinogens Lima, Caracas II, and Kaiserslautern, and as anticipated, desialylation alone was able to normalize the prolonged thrombin times and altered fibrin polymerization profiles in these molecules.3,4 10 On the other hand, desialylation alone was unable to normalize these functional abnormalities as we have observed in fibrinogen Niigata, and also fibrinogen Asahi with an extra oligosaccharide at γAsn-308 (data not shown). These data indicate that some other factors such as the steric constraints by the backbone of neutral sugars or the amino acid substitution itself may profoundly affect the process of fibrin assembly in fibrinogens Niigata and Asahi.
The location of extra oligosaccharides in some abnormal fibrinogens suggests possible explanations of their effect on fibrin polymerization. In fibrinogen Caracas II, a highly negatively charged oligosaccharide is located at Aα Asn-434 in the αC domain3 that modulates lateral association of fibrin protofibrils,24,25 and indeed, untethered αC domains of fibrinogen molecules and loosely packed thin fibrin fibers were observed by electron microscopy.12 A recent crystal structure of the cross-linked fibrin D-dimer26 indicates that the position of γ-Asn-308 is not directly involved in the D:D interface but is close to the interface. Thus, the carbohydrate backbone attached at γ-Asn-308 in fibrinogen Asahi may have a high freedom of rotation and may be long enough to interfere with the E-D binding, D:D association,26,27 and factor XIIIa-catalyzed cross-linking of the γ-chain in concert with steric hindrance.9 On the basis of crystal structure of fragment D, the Bβ-158 residue is located in the middle of the coiled-coil region, a region interposed between the E and D domains.
It is well known that the ultrastructure of fibrin clots is highly dependent on ionic strength, pH, divalent metal ions, and negatively charged substances, and some plasma proteins, such as albumin, were reported to influence the structure of fibrin network.28-34The role of the carbohydrate as a regulating factor in the process of fibrin assembly was first shown by Langer et al11 in the experiments using deglycosylated normal fibrinogen, where the DG-fibrinogen manifested shortened thrombin clotting with accelerated polymerization and formation of highly turbid clots made of thick and less-branched straight fibers. These findings were confirmed in DG-normal fibrinogen, but not in DG-Niigata fibrinogen (Table 3 and Fig2). The enzymatic removal of N-linked oligosaccharides inevitably changes the Asn residue to an Asp residue by hydrolyzing the β-aspartylglucosamine bond, and results in the introduction of a negative charge in the variant Bβ-chain, as observed by increased mobility of DG-Niigata Bβ′-chain on SDS-PAGE (Fig 6). This additional negative charge of DG-Niigata fibrinogen was probably responsible for the difference in network structure, especially in fiber width, length, and the number of branch points of the 2 DG-fibrins (Fig 7). In SEM images, the DG-normal fibrin network was more porous, and was composed of thick and straight fibers, whereas the DG-Niigata fibrin network fibers were similar to the non-DG normal fibrin network. On the contrary, the differences between the 2 untreated fibrins seem to be minor, although the network of Niigata fibrin was made of more curvilinear fibers.
The change from a curvilinear fiber network to a straighter fiber network observed in the DG-Niigata fibrin suggested the restoration of the fibrin structures to that of normal, although the widths of Niigata fibrin fibers were generally not as wide as the DG-normal fibrin. The normal and DG-Niigata fibrins have different biophysical properties from their non-DG counterparts, as evidenced by permeability and compaction experiments (Table 4). Compaction, the collapsibility of the network under constant centrifugal forces, is dependent on the characteristics of the clot structure, ie, fiber thickness and branch point density in the network. It has been shown that when the number of branch points is reduced, fibrin fibers become thick and compaction increases proportionately. Because compaction and permeability correlate significantly to the overall network structure observed by electron microscopy, we speculate on Niigata fibrin as follows: (1) on incubation with thrombin, Niigata fibrinogen forms a fibrin network in which the fibers are curvilinear and more branched but their lengths and widths are similar to those of normal fibrin. This type of network retains similar network strength and permeation to that of normal fibrin. This is consistent with the observation that the patient and her son are asymptomatic. (2) DG-fibrinogen Niigata forms a fibrin network similar to non–DG-normal fibrin in appearance but its structure and biophysical characteristics may be intermediate between that of the non–DG-normal and DG-normal fibrin. This type of network has higher permeation and lower stiffness than that of untreated normal fibrin, suggesting that DG-Niigata fibrin aggregated obviously with a much slower rate than the non–DG-normal and Niigata fibrins. This retardation or perturbation of fiber aggregation of the DG-Niigata fibrin may partly be attributed to the negative charge of a newly formed Asp residue at position Bβ-158.
Taken together, we conclude that the extra oligosaccharide introduced into the middle of coiled-coil region of fibrinogen Niigata may perturb the lateral association of protofibrils and fiber aggregation by the steric constraint of the carbohydrate backbone and also by its terminal negative charges. However, their effect would not disrupt the interactions of major polymerization domains so that the fibrin Niigata retained normal stiffness and permeability.
ACKNOWLEDGMENT
We thank Michiko Takano for her expert secretarial assistance.
Supported in part by Scientific Research Grants-in-Aid for Scientific Research 08407034 and 11470250, and for International Scientific Research Program, Joint Research Grants 09044329, 10044316, and 11694308 from the Ministry of Education, Science and Culture of the Government of Japan and the American Heart Association, Wisconsin Affiliate, Grants-In-Aid 97-GB-88 and 97-GC-60.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Teruko Sugo, PhD, Division of Hemostasis and Thrombosis Research, Institute of Hematology, Jichi Medical School, Yakushiji 3311-1, Tochigi, 329-0498, Japan.