Abstract
Families with 3 different syndromes characterized by autosomal dominant inheritance of low platelet count and giant platelets were studied. Fechtner syndrome is an autosomal-dominant variant of Alport syndrome manifested by nephritis, sensorineural hearing loss, and cataract formation in addition to macrothrombocytopenia and polymorphonuclear inclusion bodies. Sebastian platelet syndrome is an autosomal-dominant macrothrombocytopenia combined with neutrophil inclusions that differ from those found in May-Hegglin syndrome or Chediak-Higashi syndrome or the Dohle bodies described in patients with sepsis. These inclusions are, however, similar to those described in Fechtner syndrome. Other features of Alport syndrome, though, including deafness, cataracts, and nephritis, are absent in Sebastian platelet syndrome. Epstein syndrome is characterized by macrothrombocytopenia without neutrophil inclusions, in addition to the classical Alport manifestations—deafness, cataracts, and nephritis—and it is also inherited in an autosomal-dominant mode. We mapped the disease-causing gene to the long arm of chromosome 22 in an Italian family with Fechtner syndrome, 2 German families with the Sebastian platelet syndrome, and an American family with the Epstein syndrome. Four markers on chromosome 22q yielded an LOD score greater than 2.76. A maximal 2-point LOD score of 3.41 was obtained with the marker D22S683 at a recombination fraction of 0.00. Recombination analysis placed the disease-causing gene in a 3.37-Mb interval between the markers D22S284 and D22S693. The disease-causing gene interval in these 3 syndromes is similar to the interval described recently in an Israeli family with a slightly different Fechtner syndrome than the one described here. Recombination analysis of these 3 syndromes refines the interval containing the disease-causing gene from 5.5 Mb to 3.37 Mb. The clinical likeness and the similar interval containing the disease-causing gene suggest that the 3 different syndromes may arise from a similar genetic defect.
Introduction
Autosomal-dominant giant platelet disorders are rare. The most prevalent diseases that belong to this entity are May-Hegglin anomaly, Fechtner syndrome, Sebastian platelet syndrome, and Epstein syndrome. Fechtner syndrome, first described in 1985 by Peterson et al,1 is an autosomal-dominant variant of Alport syndrome manifested by nephritis, sensorineural hearing loss, cataract formation, macrothrombocytopenia, and polymorphonuclear inclusion bodies. Two other large families were described so far with this syndrome. The second Fechtner family was described by Gershoni-Baruch2 in 1988. In this family, the affected members had impaired liver function and hypercholesterolemia in addition to the other ailments. The third Fechtner family was described by Rocca et al3 in 1993.
In 1990, Greinacher et al4 described the Sebastian platelet syndrome (SPS), a new variant of hereditary, autosomal-dominant macrothrombocytopenia combined with the presence of neutrophil inclusions that differed from those found in patients with May-Hegglin anomaly,5 Chediak-Higashi syndrome, and Dohle bodies found in patients with sepsis.6,7 They are similar to those found in patients with Fechtner syndrome.1-3However, other features of Alport syndrome, including high-frequency deafness, congenital cataracts, and chronic interstitial nephritis, are absent in patients with SPS.
In 1972, Epstein described 2 families with a syndrome of macrothrombocytopenia, nephritis, and high-frequency sensorineural hearing loss inherited in an autosomal-dominant mode.8Renal and hearing abnormalities were indistinguishable from those seen in classic Alport syndrome.
Because the disease-causing gene of the Israeli Fechtner syndrome was recently located by us on the long arm of chromosome 229and because the gene for the May-Hegglin anomaly (macrothrombocytopenia and inclusion bodies in the neutrophils, which differ from those found in Fechtner syndrome) was recently located to the same area,10 11 we used markers from that area to establish a genetic linkage of the same interval to the Italian Fechtner, Sebastian platelet, and Epstein syndromes.
Patients and methods
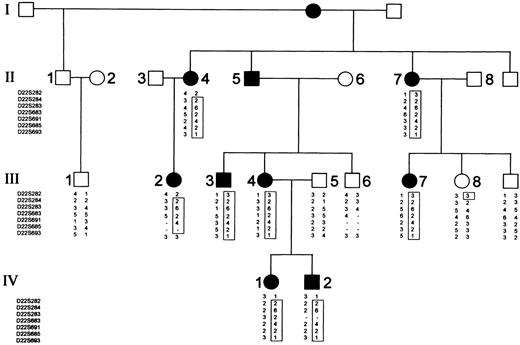
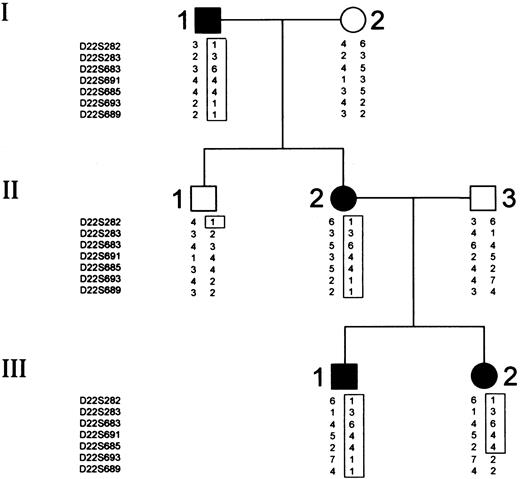
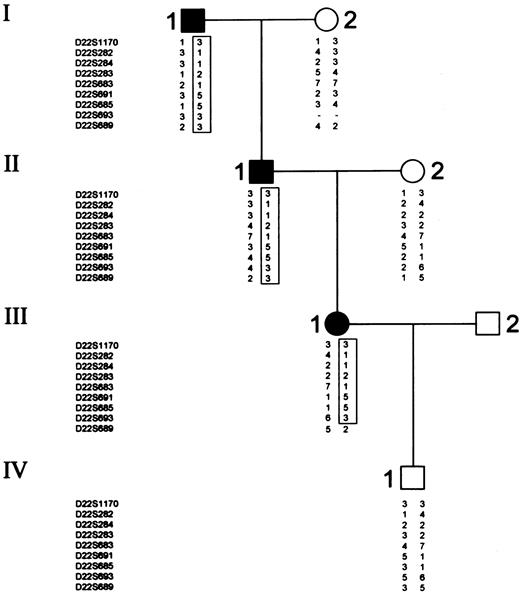
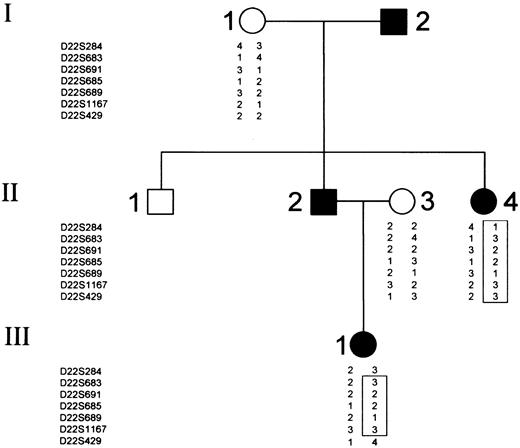
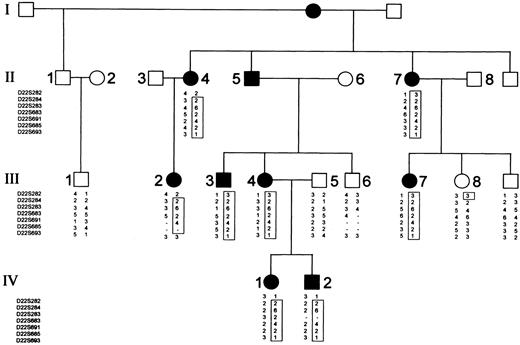
The study included 4 families affected by Fechtner syndrome, SPS, and Epstein syndrome. The first family (Figure1) is the original family described by Rocca et al3 in 1993. The second family (Figure2) is the originally described family with SPS syndrome,4 and the third family (Figure3) is new. The fourth family (Figure4) is the original family described by Epstein in 1972.8 All the affected patients in the first family with Fechtner syndrome had macrothrombocytopenia, polymorphonuclear inclusion bodies, and various combinations of nephropathy, eye abnormalities, and sensorineural hearing loss. Some patients from this family were recruited in Italy; peripheral blood smears were the source for DNA analysis in others.
Italian Fechtner family pedigree and typing for 8 chromosome 22 markers.
Circles represent females, and squares represent males. Open symbols denote unaffected family members; closed symbols denote affected family members. Critical recombinations in family members II-4, III-2, III-8, IV-1, and IV-2 define a 2-6-2-4-2-1 haplotype that is coinherited with the disease and that is not shared by the unaffected family members.
Italian Fechtner family pedigree and typing for 8 chromosome 22 markers.
Circles represent females, and squares represent males. Open symbols denote unaffected family members; closed symbols denote affected family members. Critical recombinations in family members II-4, III-2, III-8, IV-1, and IV-2 define a 2-6-2-4-2-1 haplotype that is coinherited with the disease and that is not shared by the unaffected family members.
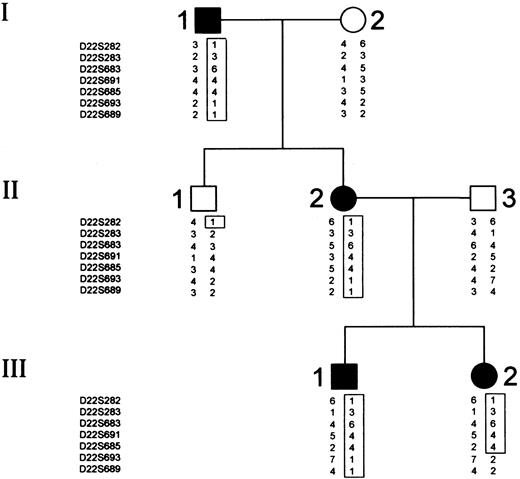
Sebastian A family pedigree and typing for 8 chromosome 22 markers.
Circles represent females, and squares represent males. Open symbols denote unaffected family members; closed symbols denote affected family members. Critical recombinations in family members II-1 and III-2 define a 3-6-4-4 haplotype that is coinherited with the disease and that is not shared by the unaffected family members.
Sebastian A family pedigree and typing for 8 chromosome 22 markers.
Circles represent females, and squares represent males. Open symbols denote unaffected family members; closed symbols denote affected family members. Critical recombinations in family members II-1 and III-2 define a 3-6-4-4 haplotype that is coinherited with the disease and that is not shared by the unaffected family members.
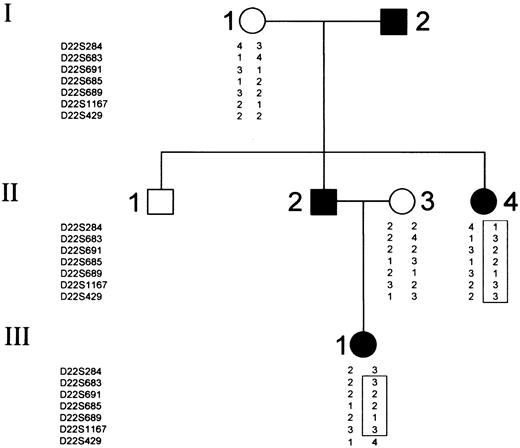
Sebastian B family pedigree and typing for 10 chromosome 22 markers.
Circles represent females, and squares represent males. Open symbols denote unaffected family members; closed symbols denote affected family members. Critical recombination in family member III-1 define a 3-1-1-2-1-5-5-3 haplotype that is coinherited with the disease and that is not shared by the unaffected family members.
Sebastian B family pedigree and typing for 10 chromosome 22 markers.
Circles represent females, and squares represent males. Open symbols denote unaffected family members; closed symbols denote affected family members. Critical recombination in family member III-1 define a 3-1-1-2-1-5-5-3 haplotype that is coinherited with the disease and that is not shared by the unaffected family members.
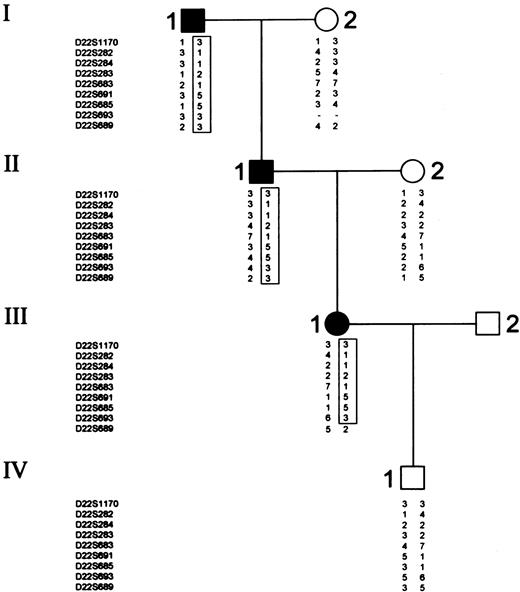
Epstein family pedigree and typing for 8 chromosome 22 markers.
Circles represent females, and squares represent males. Open symbols denote unaffected family members; closed symbols denote affected family members. Critical recombinations in family members III-1 define a 3-2-2-1-3 haplotype that is coinherited with the disease and that is not shared by the unaffected family members.
Epstein family pedigree and typing for 8 chromosome 22 markers.
Circles represent females, and squares represent males. Open symbols denote unaffected family members; closed symbols denote affected family members. Critical recombinations in family members III-1 define a 3-2-2-1-3 haplotype that is coinherited with the disease and that is not shared by the unaffected family members.
All the affected patients in families 2 and 3 had macrothrombocytopenia and polymorphonuclear inclusion bodies. There were no nephropathy or eye abnormalities in the families. However, as described in the original report, one patient has a hearing problem, possibly acquired from work in a noisy factory. The patients were recruited in Germany.
All the affected patients in the Epstein family had macrothrombocytopenia, nephritis, and deafness. The patients were recruited in the United States.
The study was approved by the institutional review board, and informed consent was obtained from all participants. Each subject underwent complete physical and ophthalmologic examinations, hearing test, complete blood count, kidney and liver function tests, and Giemsa staining under a light microscope for the study of polymorphonuclear inclusion bodies.
Genotyping
DNA was extracted from whole blood according to a standard phenol-chloroform protocol12 or from buffy coat using QIAamp blood kit (Qiagen, Hilden, Germany). DNA was extracted from peripheral blood smears using the QIAamp DNA blood mini kit (Qiagen). We used the CHLC/Weber Human Screening set 8/8RG (Research Genetics, Huntsville, AL), of polymorphic markers. Markers specifically described in this study include D22S1170, D22S282, D22S284, D22S283, D22S683, D22S691, D22S685, D22S693, D22S689, and D22S429. Polymerase chain reactions (PCR) were carried out in a 15-μL reaction volume containing 150 ng genomic DNA, 10 pmol each unlabeled primer, 1.5 mmol/L dNTP (dCTP depleted), 0.1 μCi dCTP,321.5 mmol/L MgCl2, 0.5 U Taq polymerase (Bioline, UK), and PCR buffer containing 160 mmol/L (NH4)SO4, 670 mmol/L Tris HCl (pH 8.8), and 0.1% Tween 20. After an initial denaturation of 5 minutes at 94°C, 35 cycles were performed (94°C for 30 seconds, 55°C for 30 seconds, and 72°C for 30 seconds) followed by a final extension time of 5 minutes at 72°C. Samples were mixed with 10-μL loading buffer, denatured at 94°C for 3 minutes, and electrophoresed on 6% denaturing polyacrylamide gel.
Linkage analysis
Linkage was calculated with the LINKAGE package of computer programs (version 5.1).13 Patients with macrothrombocytopenia and inclusion bodies in the polymorphonuclears[AUr] were considered affected. The trait was assumed to be autosomal dominant, with a disease-allele frequency of 0.001 and a penetrance of 1.00.
Results
The markers used for linkage analysis in the study were those that were found to be linked with Fechtner syndrome on chromosome 22q11-13.9 Figure 1 shows typing results for the Italian Fechtner family, with 8 chromosome 22 markers. Recombinant events in patients II-4, III-2, III-8, IV-1, and IV-2 established D22S693 and D22S282 as the centromeric and telomeric boundaries of the interval containing the disease-causing gene, respectively. Figure 2 shows typing results for SPS family A, with 8 chromosome 22 markers. Figure 3shows typing results for SPS family B, with 10 chromosome 22 markers. Two recombinant events in affected family members III-2 in family A and III-1 in family B, and one such recombination in a healthy member II-1 in family A, established D22S693 and D22S282 as the centromeric and telomeric boundary of the interval, respectively. Figure 4 shows typing results for the Epstein family. Two recombination events were noted in the Epstein family, one in marker D22S429 in patient III-1. This marker is centromeric to D22S693, which is the centromeric boundary of the interval according to linkage analysis of the Fechtner and SPS families and, therefore, does not refine the interval. Another recombination was noted in D22S284, which is centromeric to D22S282, found to be the telomeric boundary of the interval according to linkage analysis in both Fechtner and SPS syndromes.
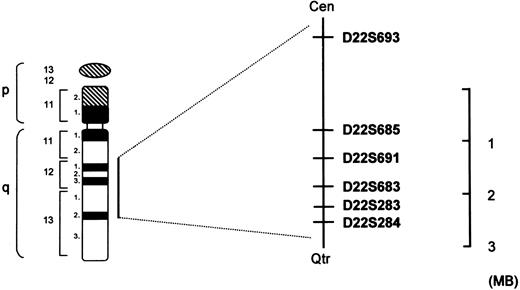
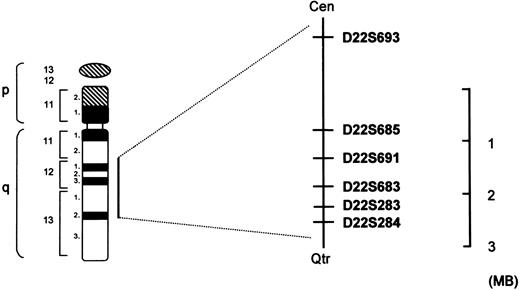
An arithmetic summary of the 2-point LOD scores, calculated separately according to the typing of the 4 different families, is shown in Table 1. Four markers showed a LOD score of more than 2.76. A maximal 2-point LOD score (Zmax) of 3.41 was obtained with the marker D22S683 at a maximal recombination fraction of 0.00. Thus, the disease-causing gene maps to a 16-cM interval between markers D22S284 and D22S693. According to established physical maps, this interval spans 3.37 Mb (Figure 5).
Schematic map of the interval containing the disease-causing gene on chromosome 22 in the autosomal-dominant giant platelet syndromes.
Schematic map of the interval containing the disease-causing gene on chromosome 22 in the autosomal-dominant giant platelet syndromes.
Discussion
Autosomal-dominant giant platelet syndromes have similar clinical characteristics and an autosomal-dominant mode of inheritance. This prompted us to look first at the markers on the interval on chromosome 22q11-13 that were recently found by us9 and others10 11 to be linked with a high LOD score to Fechtner syndrome as candidate markers for genetic linkage with these diseases. We analyzed Italian Fechtner, Sebastian platelet, and Epstein syndromes together for the same reasons.
In the families described above, we demonstrated that the disease-causing gene maps to chromosome 22q11-13. Four markers on the long arm of chromosome 22 yielded a LOD score greater than 2.76. One marker conveyed a maximal LOD score of 3.41. Haplotype analysis placed the disease-causing gene in a 3.37-Mb interval between D22S284 and D22S693. The high LOD score and the clinical similarity between these syndromes support the notion that this interval indeed contains the disease-causing gene in all 3 syndromes.
Our work sheds more light on the genetics of giant platelet syndromes that are actually a part of the Alport-like syndromes. An updated comparison between the Alport-like families—the X-linked and recessive forms of Alport syndrome—is illustrated in Table2.
The fact that all giant platelet syndromes map to the same area and probably stem from the same genetic defect may theoretically be explained in 3 ways: the interval may contain more than one gene or it may contain contiguous genes that may be mutated or deleted in these diseases; different mutations may occur in the same gene; different modifier genes may be affected that modulate the effect of the same mutation.
Among the most attractive candidate genes to be mutated in the giant platelet syndromes is the gene encoding for glycoprotein 1b-β, recently found to be deleted in another macrothrombocytopenic state, Bernard-Soulier syndrome.14 However this gene is located a few million bases from the area containing the disease-causing gene in our families.
Another possible candidate gene to be mutated in the giant platelet syndromes is a collagen type IV gene because this is a structural gene that governs the composition of the basement membrane in the glomerulus, lens capsule, and inner ear, known to be the tissues involved in Alport syndrome. However, several of the syndromes mentioned (SPS and May-Hegglin) have no clinical features in common with Alport syndrome, and the role of basement membrane in the maturing process of megakaryocytes and platelet biogenesis is not established.
A gene that affects platelet biogenesis is more attractive. That this candidate gene is sometimes involved in tissue alterations may be explained, for example, by mutations that lead to deleterious accumulation of the mutated protein in renal epithelial cells, lens capsule, or inner ear and in megakaryocytes, whereas mutations leading to the absence of protein would affect platelet biogenesis only.
The cloning of the gene involved in the autosomal-dominant giant platelet syndromes may deepen our understanding with regard to genetic and nongenetic diseases of the tissues involved in these syndromes. Moreover, these syndromes comprise the biologic model to study the linkage between megakaryocytopoiesis and platelet production, a still unresolved question in hematopoiesis.
Acknowledgment
This work was performed in partial fulfillment of the requirements for a PhD degree of Amos Toren, Sackler Faculty of Medicine, Tel-Aviv University.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Amos Toren, Pediatric Hemato-Oncology Department and the Institute of Hematology, The Chaim Sheba Medical Center, Tel-Hashomer, 52621, Israel; e-mail:amost@post.tau.ac.il.