Abstract
Ex vivo expanded peripheral blood progenitor cells (PBPCs) have been proposed as a source of hematopoietic support to decrease or eliminate the period of neutropenia after high-dose chemotherapy. CD34 cells were selected from rhG-CSF mobilized PBPCs from patients with breast cancer and were cultured for 10 days in defined media containing 100 ng/mL each of rhSCF, rhG-CSF, and PEG-rhMGDF in 1 L Teflon bags at 20 000 cells/mL. After culture the cells were washed and reinfused on day 0 of transplantation. On day +1, cohort 1 patients (n = 10) also received an unexpanded CD34-selected PBPC product. These patients engrafted neutrophils (absolute neutrophil count, >500/μL) in a median of 6 (range, 5-14) days. Cohort 2 patients (n = 11), who received expanded PBPCs only, engrafted neutrophils in a median of 8 (range, 4-16) days. In comparison, the median time to neutrophil engraftment in a historical control group of patients (n = 100) was 9 days (range, 7-30 days). All surviving patients are now past the 15-month posttransplantation stage with no evidence of late graft failure. The total number of nucleated cells harvested after expansion culture was shown to be the best predictor of time to neutrophil engraftment, with all patients receiving more than 4 × 107 cells/kg, engrafting neutrophils by day 8. No significant effect on platelet recovery was observed in any patient. These data demonstrate that PBPCs expanded under the conditions defined can shorten the time to engraftment of neutrophils compared with historical controls and that the rate of engraftment is related to the dose of expanded cells transplanted.
Introduction
Transplantation of mobilized peripheral blood progenitor cells (PBPCs) after high-dose chemotherapy has resulted in decreased time to neutrophil and platelet engraftment, compared to the engraftment resulting from bone marrow transplantation.1,2However, clinically significant periods of neutropenia and thrombocytopenia after transplantation of mobilized PBPCs still exist. Recent studies in normal baboons demonstrated that the use of ex vivo expanded PBPCs could greatly reduce, and in some animals eliminate, neutropenia after lethal total body irradiation.3 In these animal studies,3,4 CD34+ PBPCs were cultured in defined media (Amgen, Thousand Oaks, CA) containing recombinant human stem cell factor (rhSCF), recombinant human granulocyte colony-stimulating factor (rhG-CSF), and recombinant human megakaryocyte growth and development factor (PEG-rhMGDF) for 10 days in Teflon (American Fluoroseal, Gaithersburg, MD) bags. Animals that received expanded PBPCs and posttransplantation growth factor support engrafted neutrophils by day 3, whereas control animals engrafted neutrophils on day 13. Animals transplanted with ex vivo expanded cells that did not receive growth factors after transplantation had engraftment equivalent to that of animals transplanted with unexpanded cells. No effect was observed on platelet engraftment with the expanded cells.3
Ex vivo expansion has also been shown to be an effective strategy for purging bone marrow harvests or PBPC autografts for patients with chronic myelogenous leukemia,5,6 acute myelogenous leukemia,7 and non-Hodgkin lymphoma.8 Because it is extremely difficult to demonstrate the clonogenic growth of primary breast cancer cells in liquid culture,9 we postulated that ex vivo expansion might be an effective way to eradicate or reduce breast cancer cells contained in PBPC autografts. Numerous clinical studies10-13 have been reported using ex vivo expanded cells generated under a range of culture conditions that differ with respect to the growth factor regimens, the culture media, and, in some studies, the addition of fetal calf serum. The results of these studies have confirmed the safety of infusion of ex vivo expanded cells but have shown little, if any, clinical benefit with respect to improved rates of engraftment or purging of tumor cells. The aim of the current study was to evaluate, in patients with breast cancer receiving high-dose chemotherapy, the culture conditions that were effective in reducing the period of neutropenia in lethally irradiated baboons,3 to determine whether they would provide a product capable of rapid engraftment and purged of tumor cells.
Patients, materials, and methods
Patients
Study patients.
The study protocol was approved by the Combined Multiple Institutional Review Board at the University of Colorado Health Sciences Center, and all patients gave written informed consent before study enrollment. Patients with stage II or III breast cancer involving 4 or more axillary lymph nodes or with stage IV disease were eligible for this study. Normal vital organ function and a Karnofsky performance status of 80% or more were enrollment requirements, as previously described.14
Control patients.
The control group included 100 breast cancer patients treated within 2 years of the study patients, matched for stage of disease, prior therapy, phase of trial (I vs II), and high-dose regimen. The comparability of study and control patients is summarized in Table1. All control patients were mobilized with rhG-CSF and received systemic rhG-CSF after transplantation until engraftment (absolute neutrophil count [ANC] > 500/μL). Mobilization and posttransplant doses of rhG-CSF were identical to those used in the study patients, described below.
Study design
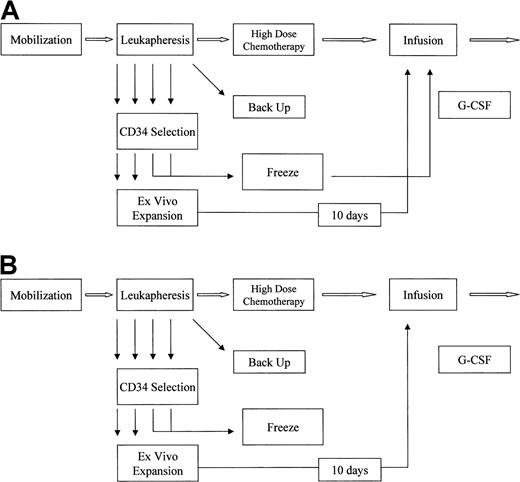
Collection phase.
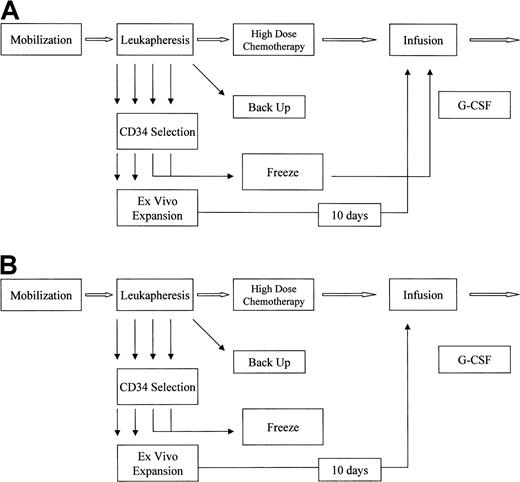
Eligible patients received rhG-CSF 10 μg/kg per day by subcutaneous injection for 9 consecutive days (Figure1A,B). Leukapheresis began on day 5 of growth factor administration and was performed daily for 5 consecutive days. Each leukapheresis processed 2.8 to 4 times the patient's blood volume (approximately 12 to 18 L) using a Cobe Spectra apheresis device (Cobe Laboratories, Lakewood, CO). The first 4 leukapheresis products were CD34-selected using the Isolex-300i device (Nexell, Irvine, CA), following the manufacturer's recommended procedures, and the selected cells were cryopreserved. The CD34 selection and cryopreservation procedures were performed on the day of collection for all products. Five leukapheresis products were collected for each patient. The first 4 apheresis products were CD34-selected, and the fifth was cryopreserved as a backup.
Schemas for patients.
(A) Ex vivo expansion, cohort 1. (B) Ex vivo expansion, cohort 2.
Schemas for patients.
(A) Ex vivo expansion, cohort 1. (B) Ex vivo expansion, cohort 2.
Transplantation and follow-up.
Within 2 to 10 days of completion of the leukapheresis procedures, patients were admitted to the hospital and treated with high-dose chemotherapy. Study and control patients enrolled on phase II chemotherapy protocols received cyclophosphamide, 1875 mg/m2 per day, given intravenously over 1 hour on each of 3 days (days −5 through −3); cisplatin, 55 mg/m2 per day, given by continuous intravenous infusion for 3 days (days −5 through −3); and carmustine, 600 mg/m2 per day, given intravenously over 2 hours on day −2 (cyclophosphamide-cisplatin-BCNU [CCB]), or taxol 725 mg/m2 as a continuous intravenous infusion for 24 hours on day −7, followed by cyclophosphamide and cisplatin in the doses and schedule used for the previous regimen (days −5 through −3) (cyclophosphamide-cisplatin-taxol [CCT]). Study and control patients enrolled on phase I chemotherapy protocols received taxotere at 250 or 350 mg/m2 given intravenously over 2 hours on day −7, melphalan 50 mg/m2 intravenously over 1 hour on each of 3 days (days −5 through −3), and carboplatin 1 g/m2 as a continuous intravenous infusion for 72 hours (days −5 through −3) (taxotere-carboplatin [TCM]).
After a 48-hour rest period, study patients received the ex vivo expanded cells on day 0. Patients in cohort 1 also received uncultured CD34+ PBPCs on day +1 (Figure 1A). Beginning on day 0, all patients received rhG-CSF 10 μg/kg per day, either by subcutaneous injection or intravenous infusion. RhG-CSF therapy was continued until the ANC was 5000/μL or greater for 3 consecutive days or 10 000/μL or greater on one determination. Antibiotics, blood products, and intravenous fluids were administered according to institutional protocols. Complete blood counts were obtained daily until the ANC was 5000/μL or greater and the platelets (unsupported) were 20 000/μL or greater, and 3 times per week thereafter until the platelet count was 50 000/μL or greater on 2 determinations separated by a minimum of 48 hours. All patients were eligible for discharge from the hospital if they were afebrile and able to maintain adequate oral intake. Control patients received unexpanded PBPCs on days 0, +1, and—if they had more than 3 pheresis products—day +2. Beginning on day 0, control patients received rhG-CSF 10 μg/kg per day either by subcutaneous injection or intravenous infusion. The time to neutrophil and platelet engraftment was measured from the day the first infusion was administered (day 0) for study patients and control patients.
Ex vivo expansion
On day −10 of treatment, 2 apheresis products were thawed and placed into ex vivo expansion culture. The cells were diluted to 20 000 cells/mL in 800 mL in defined media (Amgen) supplemented with 100 ng/mL each of rhSCF, PEG-rhMGDF, and rhG-CSF (all growth factors were supplied by Amgen) and then transferred to Teflon bags (American Fluoroseal). The bags were incubated at 37°C for 10 days in a 5% CO2 incubator. On day 0 of high-dose therapy administration (day 10 of ex vivo culture), the cultured cells were harvested using a cell washer (Cobe), and the media and growth factors were removed with washing.
Immediately before transplantation, an aliquot of each day 10 PBPC culture was removed for the following analyses: complete blood count and differential, CD34+ cell count, breast cancer cell immunohistochemistry, and microbial culture (aerobic and anaerobic bacteria, fungi, and Mycoplasma).
Megakaryocytic cell analysis
Cytospins of the day 10 cultures were prepared and stained with anti CD41 for immunohistochemistry, and the megakaryocyte content was enumerated by the collaborating pathologists.
Progenitor cell assays
Myeloid progenitor cells were evaluated on apheresis products, CD34-selected products, and ex vivo expanded cells by flow analysis of CD34 expression using the ISHAGE analysis procedure.15
Breast cancer cell assays
A sample from every unmanipulated, CD34+, and cultured PBPC fraction was evaluated for breast cancer. For the CD34-selected fractions, the limited number of cells available precluded extensive evaluation. Mononuclear cells from the unmanipulated fraction and the CD34+ and day 10 cultured cells were washed with phosphate-buffered saline containing 10% fetal bovine serum and adjusted to a concentration of 5.0 × 106 cells/mL. Two hundred microliters of the cell suspension were added to cytocentrifuge chambers, and the cells were centrifuged at 500 rpm for 5 minutes onto silane-coated slides. Ten slides (with a total of 10 × 106 cells) prepared with cells from the apheresis products and the ex vivo expanded cells were stained with a panel of monoclonal antibodies previously shown to be effective for identifying breast tumor cells among hematopoietic cells16 (Bre-3; donated by Dr Roberto Ceriani) using a previously described APAAP technique.17 Immunostained slides were counterstained with hematoxylin and microscopically examined in a blinded fashion. The stained cells were systematically scanned with a conventional light microscope using a low-power (10 ×) objective. Immunoreactive cells identified at scanning magnification were scrutinized at high-power magnification to confirm the presence of malignant histologic features. These features included large cell size, high nuclear/cytoplasmic ratio, active-appearing nuclear chromatin, prominent nucleoli, and cell clustering.
Study end points and statistical analyses
Primary efficacy end points for this study included the number of days from the first day of infusion of cells (day 0) to neutrophil engraftment (500/μL or more) and the number of days until platelet engraftment (20 000/μL or more), independent of platelet transfusions. Statistical analysis of the time to neutrophil and platelet engraftment of cohorts 1 and 2 compared to the historical group was performed using the Kruskal-Wallis nonparametric analysis of variance from SAS PROC NPAR1WAY. The secondary end points included the magnitude of breast cancer cell depletion and myeloid progenitor cell expansion.
Results
Twenty-one patients with breast cancer were enrolled in this study. The demographic data and the high-dose chemotherapy regimens the patients received are summarized in Table 1. Twelve patients were enrolled on phase II chemotherapy protocols in the adjuvant setting with either 4 to 9 (n = 3) or 10 or more (n = 7) positive axillary lymph nodes or inflammatory cancer (n = 2). The remaining patients with metastatic disease were enrolled on phase II chemotherapy trials with no evidence of disease (n = 5) or disease responding to induction therapy (n = 2), or they were enrolled on phase I chemotherapy trials for refractory disease (n = 2). The high-dose chemotherapy regimens for patients enrolled in cohort 1 or 2 are summarized in Table 2. The first 10 patients enrolled into the study were assigned to cohort 1 and received both expanded and uncultured CD34+ PBPCs. Six of these 10 patients received CCB, 2 patients received CCT, and 2 patients received TCM. The subsequent 11 patients were assigned to cohort 2 and received CCB (n = 10) or CCT (n = 1), followed by the expanded CD34+ PBPCs as their sole hematopoietic support.
Selection and ex vivo culture
For cohort 1, the median total number of CD34+cells collected in 4 apheresis products was 8.4 (range, 2.5 to 23.9) × 106 CD34+ cells/kg. The median number of CD34+ cells/kg in the 2 expanded apheresis products was 4.4 (range, 1.1 to 13.3) × 106CD34+ cells/kg. The 2 apheresis products used for expansion in cohort 2 contained a median of 4.6 (range, 1.8 to 7.6) × 106 CD34+ cells/kg.
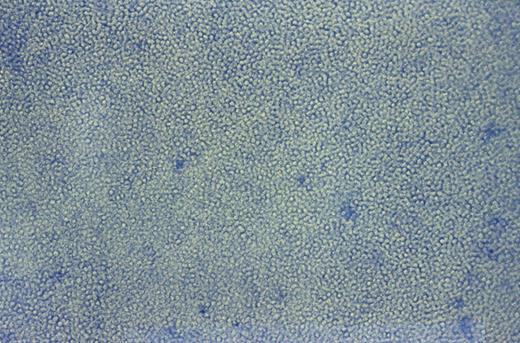
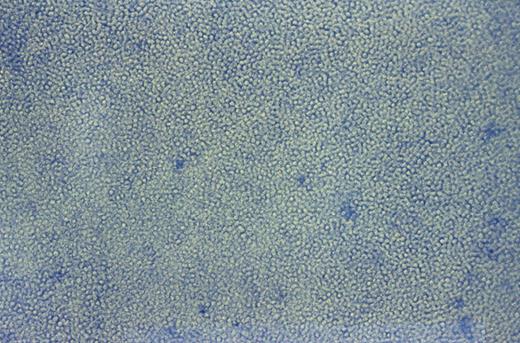
After leukapheresis the number of cells available for selection and expansion were a median of 8 × 1010 total nucleated cells (TNC) and 1.2 × 1011 TNC for cohorts 1 and 2, respectively (Table 3). The median total CD34+ cells, available for selection, was 3.0 × 108 (range, 1 to 9 × 108) and 3.4 × 108 (range, 1 to 6 × 108) for cohorts 1 and 2, respectively (Table 4). Overall the median recovery of CD34+ cells after selection was 57% with a median purity of 83% CD34+ cells. The CD34+ cell products were cultured in Teflon (American Fluoroseal) bags at a cell density of 20 000 cells/mL to a maximum of 10 bags. Cultured cells formed a monolayer of cells on the lower surface of the bags, as shown in a typical day 10 culture presented in Figure 2. The median TNC harvested after ex vivo expansion was 4.4 (range, 0.6 to 7) × 109 cells (Table 3). There was a median 15-fold (range, 1.3 to 37) expansion of TNC. The median number of CD34+ cells harvested from the expansion cultures was 3.9 × 108 CD34 cells (Table 4), with a median expansion of CD34+ cells of 1.8-fold (range, 0.7 to 4.5).
Typical day 10 culture of ex vivo expanded PBPCs.
Culture photographed (400 ×) in Teflon bags before harvesting for reinfusion.
Typical day 10 culture of ex vivo expanded PBPCs.
Culture photographed (400 ×) in Teflon bags before harvesting for reinfusion.
Bags were inspected for visible microbial contamination before harvest by microscopy, and no contamination was observed in any cultures. Microbial analyses were negative for bacteria, fungus, andMycoplasma for all patients. The average viability of the cultured cells, as measured by trypan blue dye exclusion, was 98% (range, 97%-100%).
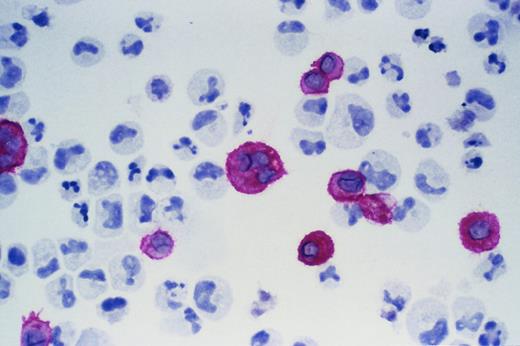
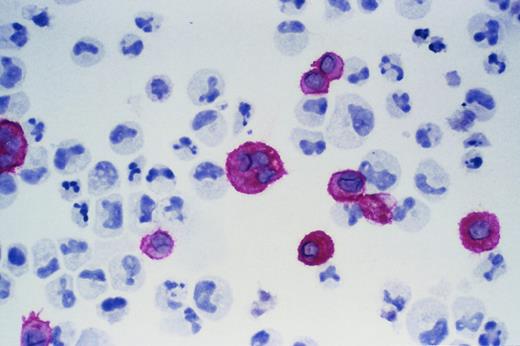
Immunohistochemistry for CD41 was performed on expanded cells from a subset of patients, and the median percentage of CD41-expressing cells was 40%. A typical immunohistochemical stain for CD41 is shown in Figure 3.
Ex vivo expanded cells.
Cells were stained with CD41b and APAAP to identify mature megakaryocytes. A typical expanded product is shown.
Ex vivo expanded cells.
Cells were stained with CD41b and APAAP to identify mature megakaryocytes. A typical expanded product is shown.
Breast cancer cell detection
Seven of the unmanipulated PBPC products from 5 patients had detectable breast cancer cells. After CD34 selection a limited number of cells were available for culture inoculation; thus insufficient cells remained for adequate performance of the immunodetection assay. No tumor cells were detectable in the ex vivo expanded products, where adequate cell numbers were assayed for tumor cells, which was consistent with a lack of clonogenic growth of breast cancer cells in in vitro culture.9 There might have been a reduction in tumor cells during the culture period; however, our inability to analyze sufficient cells from the CD34-selected fractions precluded any evaluation of this issue.
Clinical results
The median number of expanded TNC reinfused into patients was 72 (range, 12 to 91) × 106 TNC/kg and 52 (range, 7 to 125) × 106 TNC/kg for cohorts 1 and 2, respectively. The median number of expanded CD34+ cells infused for cohort 1 was 3.8 (range, 0.9 to 13.0) × 106CD34+ cells/kg, and the total CD34+ cells infused (expanded plus unexpanded products) was a median of 8.5 (range, 2.3 to 24.6) × 106 CD34+ cells/kg. Cohort 2 patients received a median of 6.6, with a range of 1.5 to 22.7 × 106, CD34+ cells/kg. There was no toxicity associated with the infusion of expanded PBPCs. Engraftment data for patients in both cohorts are presented in Table5. The median time to neutrophil engraftment, defined as the time to achieve an ANC of 500/μL or greater for 3 consecutive days, was 6 days and 8 days for cohorts 1 and 2, respectively. The time to achieve a platelet count of 20 000/μL or greater was 18.5 days and 15 days, respectively, for cohorts 1 and 2 and was not significantly different from the time to platelet engraftment of the control patients (15 days). There was no difference in the requirements for red blood cell and platelet transfusions between the 2 cohorts.
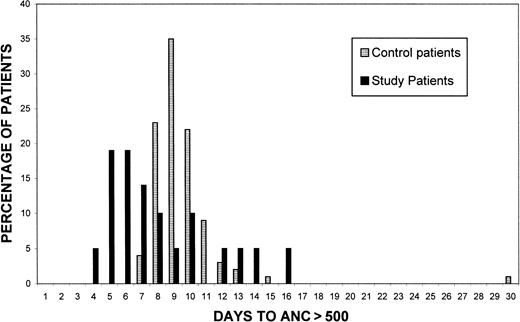
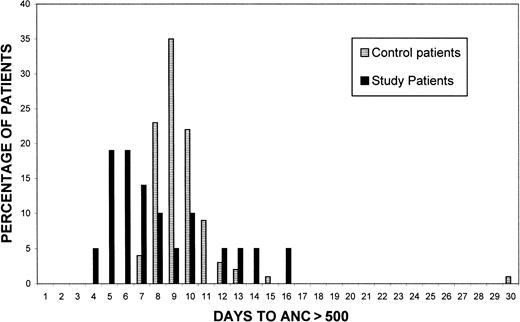
Engraftments for the historical group of patients (n = 100) are presented for comparison in Figure 3. The median time to an ANC greater than 500/μL was 9 days, with a range of 7 to 30 days. Neutrophil recovery resulting from the transplantation of the expanded cells resulted in a 3- to 4-day earlier engraftment for a number of the study patients compared with this historical control group (Figure 3), in which the earliest engraftment occurred at day 7. Statistical analysis demonstrated a significant difference in the time to neutrophil engraftment between cohort 1 (P = .02) and cohort 2 (P = .02) and the historical group. No significant difference resulted between cohorts 1 and 2 (P = .55).
Long-term follow-up
Adjuvant/inflammatory and stage IV patients with no evidence of disease remain in remission at 4 to 10 months of follow-up. Most have received chest wall radiation therapy without clinically significant myelosuppression. One patient in cohort 2 experienced delayed platelet recovery. She had a platelet count of 30 000 on day +40, when the posttransplantation radiation therapy to the chest wall was scheduled to begin. None of the other cohort 2 patients experienced delayed platelet engraftment. Patients with responsive metastatic disease remain in remission, whereas 1 of the 2 patients with refractory disease had a relapse after a short-lived partial response to high-dose therapy. Patients in cohort 2 have continued to maintain peripheral blood counts, and all patients are past the 12-month posttransplantation stage and have maintained durable engraftment. No unusual opportunistic infections were documented in any of the study patients.
Discussion
These studies have demonstrated that PBPC products from patients with breast cancer can be cultured ex vivo using these culture conditions and can be safely transplanted after high-dose chemotherapy. Expanded PBPC autografts resulted in more rapid median time to engraftment of neutrophils (P = .02 for cohorts 1 and 2 versus the historical group), with a number of patients engrafting between days 4 and 6, compared to the earliest time of engraftment of day 7 in our historical controls (n = 100, Figure 4). Analysis of the engraftment data of study and control patients by chemotherapy regimen demonstrated that the conditioning regimen did not influence the time to neutrophil engraftment. Similarly improved rates of neutrophil engraftment have been reported by Reiffers et al,18 with the same conditions used in this study to culture the autologous PBPC fractions of patients with myeloma.18
Engraftment of study patients compared to control patients.
Times to neutrophil engraftment greater than 500/μL of historical control patients (n = 100) and study patients (n = 21) treated with identical high-dose chemotherapy regimens, as described in “Patients, materials, and methods.”
Engraftment of study patients compared to control patients.
Times to neutrophil engraftment greater than 500/μL of historical control patients (n = 100) and study patients (n = 21) treated with identical high-dose chemotherapy regimens, as described in “Patients, materials, and methods.”
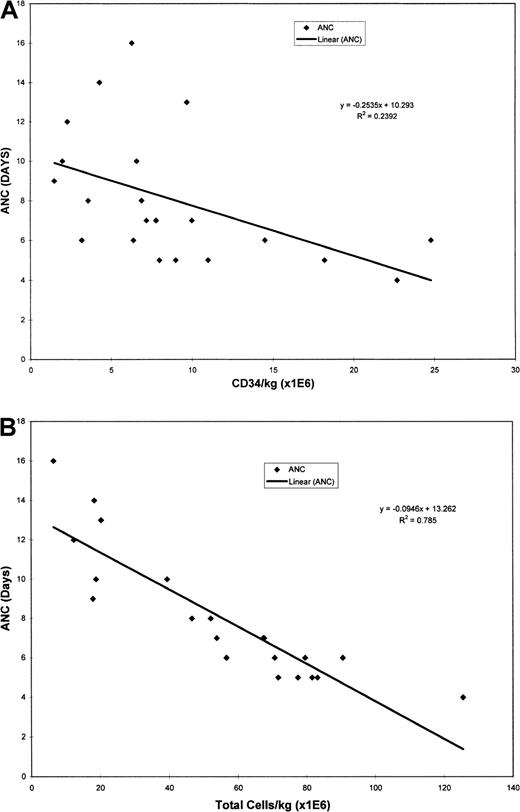
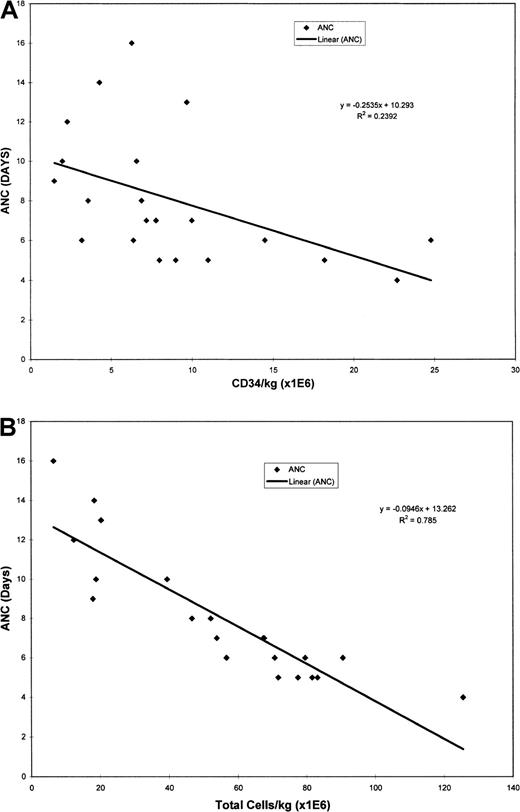
To date the major predictor of the time to engraftment for patients receiving nonexpanded PBPCs has been the number of CD34+cells per kilogram transplanted. Several studies19-21using nonexpanded products have demonstrated that there is a correlation between the time to engraftment and the number of CD34 cells per kilogram infused up to a threshold level, above which even a 10-fold higher dose of CD34+ cells does not result in faster recovery. For neutrophil recovery, doses of CD34+cells per kilogram from 2 to 2.5 × 106 up to 20 × 106 CD34+ cells/kg result in recovery of neutrophils at day 7 at the earliest.19-21 We therefore evaluated the numbers of CD34+ cell per kilogram from the expanded products reinfused in this study, and a median of 3.8 × 106 CD34 cells/kg and 6.6 × 106CD34+ cells/kg were transplanted for cohorts 1 and 2, respectively. The total CD34+ cells infused (expanded plus unexpanded products) for cohort 1 was a median of 8.5 × 106 CD34+ cells/kg. No significant correlation was obtained between the time to ANC greater than 500/μL and the dose of total CD34+ cell per kilogram infused (r2 = 0.24; Figure5A). Similarly, the dose of expanded CD34+ cells per kilogram infused showed little correlation to the time to neutrophil engraftment (r2 = 0.24). However, comparison of the total expanded nucleated cells per kilogram to the time to ANC recovery resulted in a highly significant correlation (r2 = 0.79; Figure 5B). In our study, the correlation of the number of CD34+ cells to time to recovery of ANC was poor (r2 = 0.24); however, all patients who received a minimum of 40 × 106 TNC per kilogram engrafted neutrophils in 8 days or less. Patients who received less than 40 × 106 TNC per kilogram all had slower neutrophil recovery (9 to 16 days). This level of TNC is lower than the minimal cell numbers recommended for unmanipulated bone marrow transplantation (2 × 108 MNC/kg) and suggests that the expanded cell products contain a higher frequency of cells capable of providing rapid neutrophil engraftment. Alternatively, ex vivo culture regenerates these cells, which are killed during the freezing of bone marrow or PBPCs used for autologous transplantation. These cells may be committed mature neutrophil precursors, which may be killed during freezing along with mature neutrophils. It will be of interest to evaluate the engraftment potential of ex vivo expanded allogeneic PBPC products where a direct comparison could be made to bone marrow or PBPCs that has not been cryopreserved.
Correlation of time to dose in neutrophil engraftment.
(A) Correlation between total CD34/kg and time to ANC greater than 500/μL. (B) Total number of nucleated cells from the expansion cultures per kilogram transplanted.
Correlation of time to dose in neutrophil engraftment.
(A) Correlation between total CD34/kg and time to ANC greater than 500/μL. (B) Total number of nucleated cells from the expansion cultures per kilogram transplanted.
The effect of tumor cell depletion was evaluated in all patients. There were 7 phereses (5 patients) with tumor cells in the unmanipulated PBPC fractions. No tumor cells were detected in the expanded products, but the assay did not have the sensitivity to determine whether the CD34+ preculture fraction contained tumor cells. Additionally, because the expansion cultures result in expansion of total cells there may be a dilution effect of tumor cells, and more extensive analysis is needed to determine the exact effects of ex vivo culture on purging of breast cancer cells. Previously reported studies22 have been unable to eradicate breast cancer cells completely with the CD34 selection of bone marrow or PBPC autografts. Preliminary results of this study suggest that expansion may result in important elimination of tumor cells. Because many purging procedures used to date result in a significant loss of normal CD34+ progenitor cells, the expansion procedure may compensate for these losses by expanding the committed progenitors while potentially providing additional tumor depletion benefit.
Recent data from Holmberg et al23 have suggested that selection and infusion of CD34+ cells from autologous PBPC grafts result in an increased incidence of cytomegalovirus disease. The patients reported in this study did not experience cytomegalovirus or other opportunistic infections after transplantation.
The results of this study raise several issues that remain to be resolved:
The effect of the expansion culture on long-term engrafting cells. The fate of stem cells during the expansion cultures has not been determined. Cohort 2 patients who received expanded cells as the sole source of hematopoietic support will provide supportive data on the long-term durability of engraftment. All patients in cohort 2 are now past the 12-month posttransplantation stage and continue to experience durable engraftment. The potential of residual stem cells in the patients (endogenous autologous recovery) to provide the long-term hematopoiesis will confound the issue of the effect of expansion on stem cells, and this may only be answered in a definitive manner by gene marking of the expanded cells and showing marked cells long-term in these patients. At a practical level, whether the long-term hematopoiesis comes from the expanded cells that were infused or from residual stem cells in the patient is less important than the ability of the patients to maintain long-term blood cell production with the high-dose chemotherapy regimens used. Expanded cells from the patients in cohort 2 have also been simultaneously transplanted into NOD/SCID mice24 to assay for human SCID repopulating cells (SRC). These studies have demonstrated the presence of SRC in the expanded products25 and should provide some insight into the primitive nature of the expanded cell population.
No significant difference in platelet recovery was observed with expanded cells. Immunohistochemical analysis of CD41 expression of the expanded cells demonstrates the presence of a large number of mature megakaryocytes in the expanded cell fraction; however, this is not reflected in the time to platelet recovery. There are several possible explanations for the lack of effect obtained on platelet recovery—the megakaryocytes generated in vitro may not have the capacity to generate platelets, or, more likely, the expanded cells require pharmacologic levels of thrombopoietin or other platelet growth factors after transplantation to drive platelet development.
Is it possible to eliminate neutropenia in these patients?The results presented in this study demonstrate the effect of expanded cells on improving neutrophil engraftment; however, it is possible that if more CD34+ cells are available for expansion, even more rapid engraftment may occur. Alternatively, daily reinfusion of expanded cells on days 0 through 7 may provide mature neutrophils such that patients never have neutrophil counts lower than 500/μL. Another possibility is the infusion of expanded cells at day −1 or −2 to prevent a patient from becoming neutropenic at any stage.
The potential application of expanded cells for cord blood allogeneic transplantation is also being explored at this institution. Initial data suggest that cord blood progenitors, expanded under the same culture conditions used in the current study, enable engraftment of adults with fewer total nucleated cell per kilogram of patient weight than reported with unexpanded cord blood.26 27
In summary, this study demonstrates the potential of ex vivo expanded PBPCs to provide more rapid engraftment than historical controls transplanted with unmanipulated PBPCs after high-dose chemotherapy. Ongoing analysis may provide more insight into the definitive cell types capable of providing rapid neutrophil and platelet engraftment and the growth factor requirements of these cells. Further studies are warranted to define the optimal timing for reinfusion and possible further improvements in the expansion culture conditions.
Acknowledgments
We thank Dr R. Ceriani for his generous supply of the Bre3 antibody for the breast cancer cell detection assay. We also thank Robert Briddell, Dr Anthony Gringeri, and Dr Graham Molineux (Amgen) for their support in conducting this study. Finally, we thank Nexell Therapeutics for supplying the selection columns for this study.
Supported in part by National Institutes of Health/National Cancer Institute grant RO1-CA61508 (E.J.S.) and by Amgen (I.M.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Ian McNiece, BMT Program B-116, University of Colorado Health Sciences Center, 4200 E Ninth Ave, Denver, CO 80262; e-mail: ian.mcniece@uchsc.edu.