Abstract
Subsets of natural killer (NK) cells are characterized by the expression of inhibitory and/or stimulatory receptors specific for major histocompatibility complex (MHC) class I determinants. In mice, these include the Ly49 family of molecules. One mechanism by which tumor cells may evade NK cell killing is by expressing the appropriate MHC class I and binding inhibitory Ly49 receptors. Therefore, the question of whether blocking the interaction between the Ly49 inhibitory receptors on NK and MHC class I cells on tumor cells augments antitumor activity was investigated. Blockade of Ly49C and I inhibitory receptors using F(ab′)2 fragments of the 5E6 monoclonal antibody (mAb) resulted in increased cytotoxicity against syngeneic tumors and decreased tumor cell growth in vitro. The effect of 5E6 F(ab′)2 was specific for the MHC of the tumor, as the use of F(ab′)2 of the mAb against Ly49G2 failed to increase NK activity. Treatment of leukemia-bearing mice with 5E6 F(ab′)2 fragments or adoptive transfer of NK cells treated ex vivo with the F(ab′)2 resulted in significant increases in survival. These results demonstrate that blockade of NK inhibitory receptors enhances antitumor activity both in vitro and in vivo, suggesting that NK inhibitory receptors can be responsible for diminishing antitumor responses. Therefore, strategies to block inhibitory receptors may be of potential use in increasing the efficacy of immunotherapy.
Introduction
The ability of neoplastic cells to evade the immune system remains a formidable barrier limiting the success of immunotherapy. Tumor cells can employ various mechanisms to escape detection by immune cells. These can include down-regulation of major histocompatibility complex (MHC) class I expression,1-4production of immunosuppressive cytokines such as transforming growth factor-β,1,5 up-regulation of Fas ligand,6 and deregulation of zeta chain on T cells.7 In both mouse and human, natural killer (NK) cells are composed of different subsets, which are characterized by the expression of inhibitory and/or activating receptors specific for MHC class I determinants.8-11 In mice, these receptors belong to the family of Ly49 receptors, which are lectinlike molecules.12 The human counterpart, killer immunoglobulin-like receptors, belongs to the immunoglobulin superfamily.11 A small percentage of T cells in mice also express Ly49 receptors.13 It has been shown that binding of the inhibitory receptors by the appropriate class I molecules results in generation of negative signals leading to inactivation of NK cell functions.13-15 This inhibitory signal has been shown to dominate over activating stimuli.15 Furthermore, the rapid rejection of tumors lacking the expression of MHC class I by NK cells demonstrates the pivotal role MHC plays in regulating NK function.16-18 In spite of these studies demonstrating the functions of the inhibitory receptors in vitro, the in vivo functions of these receptors on either NK or T cells remain to be elucidated.
One potential means for tumor escape may be by expressing MHC class I determinants at a level that allows sufficient binding of the Ly49 inhibitory receptors and thus escape from NK-mediated killing. In H2b strains of mice, approximately 35% to 60% of NK cells express inhibitory Ly49C and I receptors that recognize MHC H2b.19 These NK cells would then be turned off or inactivated by tumors bearing MHC H2b. It has been demonstrated that suppression of inhibitory signals in T cells by blockade of cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4), results in optimal antitumor effects.20 Therefore, although NK cells from H2b strains of mice can kill syngeneic tumors with varying efficiency, greater antitumor activity may be achieved by blocking the interaction between the Ly49 inhibitory receptor family members (ie, Ly49C and I) and their ligand (ie, H2b) present on the tumor.
To examine the effects of blockade of the inhibitory receptors on antitumor activity, we have used a C1498 mouse leukemia model and F(ab′)2 fragments of 5E6 monoclonal antibody (mAb),21 which binds to Ly49C and I receptors, for in vitro as well as in vivo studies. The use of F(ab′)2fragments allowed us to examine the responses that are due to blocking the Ly49 receptors without depletion of the subset in vivo. The results from these studies demonstrate that blockade of Ly49 inhibitory receptors augments NK cell–mediated antitumor effects and that strategies to block NK inhibitory receptor interactions may be of potential use in cancer therapy.
Materials and methods
Mice
C57BL/6 (B6, H2b) mice were obtained from the Animal Production Area (National Cancer Institute at Frederick [NCI-Frederick], MD), and B6 severe combined immunodeficient scid/scid (SCID) mice were generously provided by Dr Robert H. Wiltrout (NCI-Frederick). All mice were kept in a specific pathogen-free condition and used at 8 to 12 weeks of age.
Antibodies and generation of F(ab′)2 fragments
Antimouse FcγR (2.4G2, rat immunoglobulin [Ig]–G2a), fluorescein isothiocyanate (FITC)–conjugated anti-NK1.1 (PK136, mouse IgG2a), and biotinylated anti-Ly49C and I (5E6, mouse IgG2a) were purchased from Pharmingen (San Diego, CA). Phycoerythrin (PE)-conjugated streptavidin and F(ab′)2 fragments of normal mouse IgG (NMG) were purchased from Jackson ImmunoResearch (West Grove, PA). F(ab′)2 fragments of anti-Ly49C and I (5E6) and anti-Ly49G2 (4D11, rat IgG2a; the hybridoma was a gift from Dr John Ortaldo, NCI-FCRDC) mAbs were prepared as previously described.21 Briefly, the antibodies were purified from ascites fluid by affinity column purification, concentrated to 5 mg/mL, digested with pepsin, and neutralized with 2 M Tris base solution. The neutralized digestion mixture was dialyzed against phosphate-buffered saline (PBS) overnight. The efficiency of digestion and purity of the resulting F(ab′)2 fragments were checked by 4%- to 20%-gradient sodium dodecyl sulfate– polyacrylamide gel electrophoresis.21
Cell lines
All cell lines were obtained from American Type Culture Collection (Rockville, MD). C1498 (H2b) is a murine leukemia, and EL4 (H2b) is a murine T-cell lymphoma. P815 (H2d) is a murine mastocytoma. Frozen stocks of the cell lines were thawed every 2 months for in vitro assays.
SCID NK cell culture and cell sorting
Single-cell suspensions of splenocytes and bone marrow cells from B6 SCID mice were prepared with red cell lysis. Cells were cultured in NK cell media (RPMI 1640 supplemented with 10% fetal bovine serum [FBS], 100 U/mL penicillin/streptomycin, 2 × 103 μM l-glutamine, 10 mM Hepes, 1 mM nonessential amino acids, 1 mM sodium pyruvate, 2.5 × 10−5 M 2-ME, and 1 μg/mL indomethacin) containing 5000 IU/mL recombinant human interleukin-2 (rhIL-2) (Biological Response Modifiers Program, NCI-FCRDC) at 0.5 to 1 × 106 cells per milliliter for 5 to 7 days. For cytotoxicity assays, a pure population of NK1.1+5E6+ and NK1.1+5E6− NK cell subsets were sorted from B6 SCID splenocytes and cultured in NK media containing 5000 IU/mL rhIL-2 for 5 to 7 days as previously described.21
Cytotoxicity assay
We incubated 1.5 to 2 × 106 C1498 or EL4 targets with 150 to 250 μCi sodium chromate (51Cr) (Amersham Life Science, Arlington Heights, IL) for 1.5 hours at 37°C. Radiolabeled cells were washed and diluted to an appropriate concentration. Various numbers of NK1.1+5E6+ or NK1.1+5E6− effectors were added first to the wells of V-bottom 96-well microtiter plates in triplicates. For assays determining the effect of 5E6 F(ab′)2, the effectors were preincubated with 40 to 60 μg/mL 5E6 F(ab′)2 for 30 to 60 minutes at 37°C and then cocultured with the targets for 4 hours.51Cr activity in the culture supernatant was then measured in a liquid scintillation counter, and the percentage of specific lysis was calculated as previously described.21
Clonogenic assays
Various numbers of B6 SCID NK cells activated with rhIL-2 for 5 to 7 days were plated in U-bottom 96-well microtiter plates to achieve NK-to-tumor ratios of 100:1, 50:1, 10:1, 5:1, 2:1, or 1:1 and pretreated with media alone or 25 μg/mL F(ab′)2 fragments of NMG, 5E6, or 4D11 for 2 to 3 hours at 37°C in complete Iscoves modified Dulbecco medium (IMDM) (supplemented with 10% FBS, 100 U/mL penicillin/streptomycin, 2 × 103 μM l-glutamine, 5 × 10−5M 2-ME, and 5000 IU/mL IL-2). Then 100, 50, or 25 C1498, EL4, or P815 cells, respectively, were added per well, and the cells were cocultured for 48 hours. The cocultured cells were collected and transferred into the colony assay media (prepared the same as complete IMDM except for 1.1% methyl cellulose [wt/vol] and no rhIL-2) and plated in 35-mm petri dishes in triplicates. Cultures were incubated for 6 to 7 days in humidified atmosphere at 37°C with 5% CO2. Colonies were enumerated on a stereo microscope (Nikon, Melville, NY).
Survival studies
C1498 leukemia cells were freshly thawed 7 days prior to in vivo administration and kept in log phase until use. In some experiments, B6 mice were treated with either 5% normal mouse serum (NMS) or 180 μg 5E6 F(ab′)2 per mouse (intraperitoneally [ip]) 2 days prior to the injection of tumor cells. At day 0, mice were injected (intravenously [iv]) with a lethal dose of C1498 (1 × 105 cells), and beginning on the day of tumor injection, mice were treated with 5E6 F(ab′)2 twice a week for 3 to 4 weeks. In the experiments indicated, 10 to 12 × 106 IL-2–activated NK cells were preincubated with 300 μg 5E6 or 4D11 F(ab′)2 or 5% NMS for 2 hours at 37°C and further cocultured with 1 to 1.2 × 106 C1498 leukemia cells in 5 mL total volume in 6-well culture plates for 24 hours. As controls, 1 to 1.2 × 106 C1498 cells were cultured alone. After the coculture, mice were injected with the cocultured cells at 1 × 105 C1498 cells and 1 × 106 NK cells per mouse (iv), a dose based on the cell concentration at the initiation of the cocultures. In some experiments, adoptive transfer of NK cells was performed in mice that were injected with the cocultured NK and tumor cell mixtures described above. At days 18 and 25 post–initial NK plus tumor cell injection, 6 × 107 IL-2–activated NK cells were preincubated with 500 μg 5E6 or 4D11 F(ab′)2 or 5% NMS for 2 hours at 37°C, and without washing, the cells were diluted in PBS at 1 × 107/mL. The ex vivo–treated NK cells were then transferred into tumor-bearing mice at 5 × 106 per mouse (iv), and all mice were treated with 5 × 104 IU rhIL-2 (ip) for 3 consecutive days beginning on the day of adoptive transfer. For all in vivo studies, 6 to 8 mice per group were used in each experiment, and 2 to 3 independent experiments were performed for the various conditions.
Statistics
The statistical analyses were performed by means of the Student t test to determine the significance of the differences between experimental and control groups for in vitro assays. The P values for the survival studies were obtained with the log-rank test.
Results
Stable binding of 5E6 F(ab′)2 to Ly49C and I receptors enhances NK cell cytotoxicity
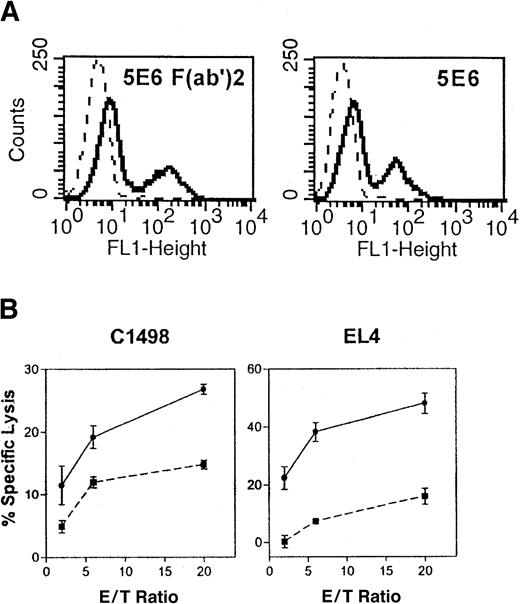
To assess the effects of blocking NK cell inhibitory receptors with F(ab′)2 fragments of 5E6 mAb, we first examined whether stable binding of 5E6 F(ab′)2 fragments on IL-2–activated NK cells can be maintained. We used SCID mice as a source of NK cells since they lack T and B cells and since culture of SCID splenocytes in IL-2 gives rise to a relatively pure population of NK cells.1 As shown in Figure1A, binding of 5E6 F(ab′)2could be detected at 37°C, and the level of expression was comparable to 5E6+ subset detected by whole antibody. In addition, binding of the F(ab′)2 fragments to Ly49C and I receptors was maintained over a 24- to 48-hour culture period (data not shown). We then determined if blocking the interaction of MHC class I expressed on C1498 (H2b) leukemia or EL4 (H2b) lymphoma cell lines and Ly49C and I receptors on NK cell subsets can result in greater cytotoxicity. In these studies, the 5E6+ and 5E6− subsets were sorted from B6 (H2b) SCID splenocytes. The sorted cells were activated with rhIL-2 for 5 to 7 days and used as effectors against C1498 or EL4 cells in a standard 4-hour cytotoxicity assay. The results show that C1498 and EL4 cells could be killed by the 5E6− subset at various levels at an effector-to-target ratio of 20:1 (18.4% ± 1.2% and 49.8% ± 1.8% specific lysis for C1498 and EL4, respectively). In contrast, both tumor cells were relatively resistant to cytotoxicity mediated by the 5E6+ NK subset (Figure 1B), and when 5E6+ NK cells were pretreated with 5E6 F(ab′)2, cytotoxicity against both targets was significantly increased (Figure 1B) to levels comparable to or higher than that mediated by the 5E6− subset. However, pretreatment of the 5E6+ subset with the F(ab′)2 fragment did not affect the level of cytotoxicity against an NK-sensitive target, YAC-1 [70.8% ± 1.7% vs 75.1% ± 6.5% specific lysis with vs without 5E6 F(ab′)2]. These results demonstrate that negative signals induced via the inhibitory receptors suppress the killing ability of NK cell subsets and that blocking these inhibitory signals augments cytotoxicity of this subset.
Effect of 5E6 F(ab′)2 fragments on 5E6+ NK cells.
The 5E6 F(ab′)2 fragments bind 5E6+ NK cells and increase cytotoxicity mediated by the 5E6+ NK cell subset. (A) IL-2–activated NK cells (5 × 106) were incubated with F(ab′)2 fragments of 5E6 (solid histogram) at 1 × 106/mL or with normal mouse IgG (dashed histogram) at 25 μg/mL for 2 hours at 37°C and stained with FITC goat antimouse IgG specific for F(ab′)2 fragments (left panel). As controls, NK cells were incubated alone and stained with biotinylated 5E6 and secondary antibody, FITC-streptavidin (right panel, solid histogram) or the secondary antibody only (dashed histogram). (B) The NK1.1+5E6+ subset was sorted from B6 SCID splenocytes by flow cytometry, activated with rhIL-2, and used at day 5 as effectors against C1498 or EL4 targets in standard 4-hour cytotoxicity assay as described previously.21 Various numbers of NK1.1+5E6+ effectors were pretreated with media (▪) or 5E6 F(ab′)2 (●), and the effectors were then cocultured with the targets for 4 hours, after which51Cr activity was measured in a liquid scintillation counter. A representative of 3 independent experiments is shown.
Effect of 5E6 F(ab′)2 fragments on 5E6+ NK cells.
The 5E6 F(ab′)2 fragments bind 5E6+ NK cells and increase cytotoxicity mediated by the 5E6+ NK cell subset. (A) IL-2–activated NK cells (5 × 106) were incubated with F(ab′)2 fragments of 5E6 (solid histogram) at 1 × 106/mL or with normal mouse IgG (dashed histogram) at 25 μg/mL for 2 hours at 37°C and stained with FITC goat antimouse IgG specific for F(ab′)2 fragments (left panel). As controls, NK cells were incubated alone and stained with biotinylated 5E6 and secondary antibody, FITC-streptavidin (right panel, solid histogram) or the secondary antibody only (dashed histogram). (B) The NK1.1+5E6+ subset was sorted from B6 SCID splenocytes by flow cytometry, activated with rhIL-2, and used at day 5 as effectors against C1498 or EL4 targets in standard 4-hour cytotoxicity assay as described previously.21 Various numbers of NK1.1+5E6+ effectors were pretreated with media (▪) or 5E6 F(ab′)2 (●), and the effectors were then cocultured with the targets for 4 hours, after which51Cr activity was measured in a liquid scintillation counter. A representative of 3 independent experiments is shown.
Blockade of Ly49C and I receptors inhibits tumor growth in vitro
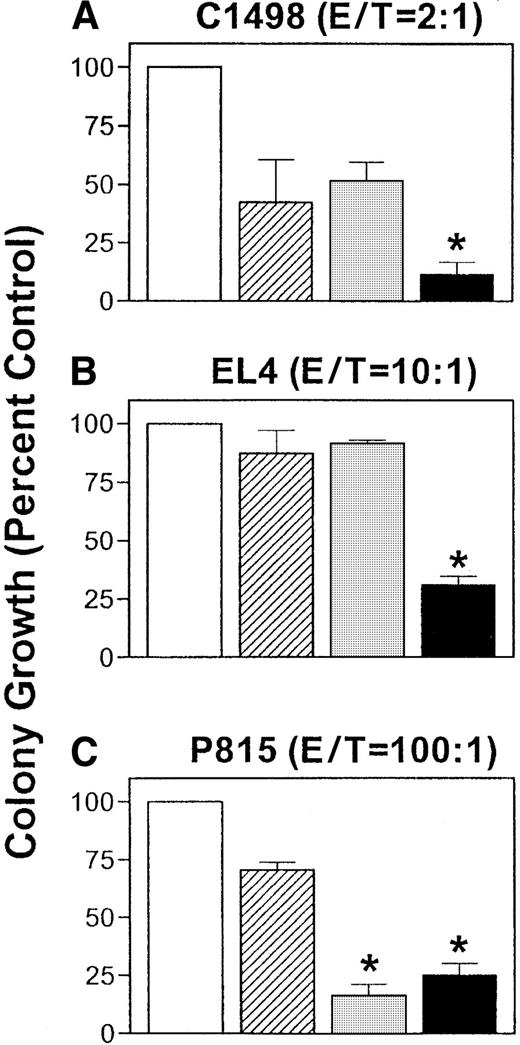
To determine whether blockade of Ly49C and I receptors increases the NK-mediated inhibition of tumor growth in vitro, IL-2–activated NK cells from B6 SCID mice were preincubated with F(ab′)2fragments of either 5E6 or 4D11, a mAb against Ly49G2 specific for H2Dd used as a control for specificity, for 2 to 3 hours. Only the 5E6 F(ab′)2 should have an effect on NK cells with tumors expressing H2b. NK cells were then incubated with syngeneic tumors, C1498 or EL4 (both H2b), or an allogeneic tumor, P815 (H2d), all of which express neither Ly49C and I nor Ly49G2 (data not shown), at different NK-to-tumor ratios for 48 hours. After coculture with NK cells, viable tumor cell counts were assessed in clonogenic assays. As shown in Figure2A, clonogenic growth of C1498 leukemia cells was inhibited by co-incubation with NK cells compared with the growth of untreated cells, and this growth inhibition was further increased when 5E6 F(ab′)2 was added (P < .05). Although the growth of EL4 was not affected by NK cells, pre-incubation with 5E6 F(ab′)2 also significantly decreased the growth of EL4 (P = .00076; Figure 2B). In contrast to the effects observed with 5E6 F(ab′)2, growth of neither C1498 nor EL4 was affected by treatment of NK cells with 4D11 F(ab′)2 (Figure 2A,B). However, the growth of P815 cells, which were relatively resistant to even allogeneic NK cells, was significantly decreased in the presence of 4D11 F(ab′)2 (P < .01; Figure 2C). Interestingly, the 5E6 F(ab′)2 also exerted an effect on growth of P815 (P < .01), corroborating previous reports showing that Ly49C and I inhibitory receptors are capable of binding, albeit weakly, to H2d in vitro.22 The addition of 5E6 or 4D11 F(ab′)2 alone to the tumor cells did not have a significant effect on their growth (data not shown).
Treatment of NK cells with 5E6 F(ab′)2.
Treatment of NK cells with 5E6 F(ab′)2 results in decreased tumor growth in vitro. Various numbers of B6 SCID NK cells activated with rhIL-2 for 5 to 7 days were plated in U-bottom 96-well microtiter plates at 50 μL per well and pretreated with media alone (■) or 25 μg/mL F(ab′)2 fragments of normal mouse IgG (NMG) (▨), 5E6 (Ly49C and I) (▪), or 4D11 (Ly49G2) (░) for 2 to 3 hours at 37°C. Then 100, 50, or 25 C1498, EL4, or P815 cells, respectively, were added at 50 μL per well, and the cells were cocultured for 48 hours. As controls, tumor cells were cultured alone. After the co-incubation, the cells were transferred into a semisolid matrix and cultured for 5 to 7 days for quantification of leukemic cell colonies. (A) C1498 (H2b) cells at NK-to-tumor ratio of 2:1. (B) EL4 (H2b) at NK-to-tumor ratio of 10:1. (C) P815 (H2d) at NK-to-tumor ratio of 100:1. Data from a representative of 3 independent experiments are shown as a percentage of control cells, where tumor growth in the absence of NK and the antibody is used as 100%. The stars indicate significant differences in 5E6 or 4D11 F(ab′)2–treated groups compared with NMG controls as determined by Studentt test.
Treatment of NK cells with 5E6 F(ab′)2.
Treatment of NK cells with 5E6 F(ab′)2 results in decreased tumor growth in vitro. Various numbers of B6 SCID NK cells activated with rhIL-2 for 5 to 7 days were plated in U-bottom 96-well microtiter plates at 50 μL per well and pretreated with media alone (■) or 25 μg/mL F(ab′)2 fragments of normal mouse IgG (NMG) (▨), 5E6 (Ly49C and I) (▪), or 4D11 (Ly49G2) (░) for 2 to 3 hours at 37°C. Then 100, 50, or 25 C1498, EL4, or P815 cells, respectively, were added at 50 μL per well, and the cells were cocultured for 48 hours. As controls, tumor cells were cultured alone. After the co-incubation, the cells were transferred into a semisolid matrix and cultured for 5 to 7 days for quantification of leukemic cell colonies. (A) C1498 (H2b) cells at NK-to-tumor ratio of 2:1. (B) EL4 (H2b) at NK-to-tumor ratio of 10:1. (C) P815 (H2d) at NK-to-tumor ratio of 100:1. Data from a representative of 3 independent experiments are shown as a percentage of control cells, where tumor growth in the absence of NK and the antibody is used as 100%. The stars indicate significant differences in 5E6 or 4D11 F(ab′)2–treated groups compared with NMG controls as determined by Studentt test.
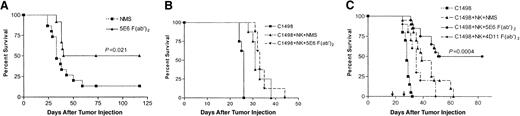
Treatment of leukemia-bearing mice with 5E6 F(ab′)2 or adoptive transfer of NK cells treated ex vivo with F(ab′)2 increases the survival rate
To address whether inhibitory receptor blockade can also result in greater antitumor activity in vivo, the C1498 acute leukemia model was employed. B6 mice were treated with 5E6 F(ab′)2 or NMS 2 days prior to injection of a lethal dose of C1498. The animals were further treated with the antibody or the control twice a week for 3 weeks post–tumor injection and monitored for survival. As shown in Figure 3A, injection of C1498 leukemia cells resulted in death of 87% of the controls in which extensive tumor growth was observed in the liver, bone marrow, and central nervous system. Treatment of mice with the 5E6 F(ab′)2resulted in a significant increase in survival (P = .021), with 50% of mice remaining disease-free up to 100 days post–tumor injection. In contrast, treatment of mice with 5E6 whole antibody to deplete the 5E6+ NK cell subset did not have any effect on the survival of mice compared with the NMS control even though 5E6+ cells decreased from 36.2% to 7.3% of NK cells after the treatment (data not shown). No toxicities, effects on hematologic parameters, or changes in the pattern of tumor growth were observed in mice receiving 5E6 F(ab′)2 (data not shown).
Effect of 5E6 F(ab′)2 on mice injected with a lethal dose of C1498.
5E6 F(ab′)2 treatment of mice injected with a lethal dose of C1498 results in increased survival rate. (A) B6 mice were treated with 180 μg 5E6 F(ab′)2 or 5% NMS (ip) 2 days prior to injection with 1 × 105 C1498 cells (iv). The animals were then treated with 180 μg 5E6 F(ab′)2 per dose or NMS twice a week for 3 weeks and monitored for survival. Pooled data from 2 independent experiments (n = 15 and 12 for NMS and 5E6 F(ab′)2 groups, respectively) is shown. (B) IL-2–activated NK cells (12 × 106) were preincubated with 300 μg 5E6 F(ab′)2 or 5% NMS for 2 hours at 37°C and were further cocultured with 1.2 × 106 C1498 leukemia cells for 24 hours. As controls, 1.2 × 106 C1498 cells were cultured alone. After the coculture, cells were washed and mice were injected with 1 × 105 C1498 and 1 × 106 NK cells per mouse (iv), a dose based on the cell concentration at the initiation of coculture (n = 8 per group). A representative of 3 independent experiments is shown. (C) B6 mice were injected with cocultured NK and C1498 cell mixture as in panel B. In addition, a group of mice were injected with NK and C1498 cell mixture that was cocultured in the presence of 300 μg 4D11 F(ab′)2. At days 18 and 25 post–initial tumor plus NK cell injection (indicated by arrows), mice in the appropriate group were injected with NK cells treated with NMS or 5E6 or 4D11 F(ab′)2(5 × 106 per mouse, iv) followed by IL-2 injection (5 × 104 IU per mouse, ip) of all mice for 3 consecutive days. Pooled data from 2 independent experiments (n = 20 per group except for 4D11 F(ab′)2–treated group in which n = 10) are shown. The P value indicates a significant difference between groups injected with NK cells treated with 5E6 or 4D11 F(ab′)2 as determined by log-rank test.
Effect of 5E6 F(ab′)2 on mice injected with a lethal dose of C1498.
5E6 F(ab′)2 treatment of mice injected with a lethal dose of C1498 results in increased survival rate. (A) B6 mice were treated with 180 μg 5E6 F(ab′)2 or 5% NMS (ip) 2 days prior to injection with 1 × 105 C1498 cells (iv). The animals were then treated with 180 μg 5E6 F(ab′)2 per dose or NMS twice a week for 3 weeks and monitored for survival. Pooled data from 2 independent experiments (n = 15 and 12 for NMS and 5E6 F(ab′)2 groups, respectively) is shown. (B) IL-2–activated NK cells (12 × 106) were preincubated with 300 μg 5E6 F(ab′)2 or 5% NMS for 2 hours at 37°C and were further cocultured with 1.2 × 106 C1498 leukemia cells for 24 hours. As controls, 1.2 × 106 C1498 cells were cultured alone. After the coculture, cells were washed and mice were injected with 1 × 105 C1498 and 1 × 106 NK cells per mouse (iv), a dose based on the cell concentration at the initiation of coculture (n = 8 per group). A representative of 3 independent experiments is shown. (C) B6 mice were injected with cocultured NK and C1498 cell mixture as in panel B. In addition, a group of mice were injected with NK and C1498 cell mixture that was cocultured in the presence of 300 μg 4D11 F(ab′)2. At days 18 and 25 post–initial tumor plus NK cell injection (indicated by arrows), mice in the appropriate group were injected with NK cells treated with NMS or 5E6 or 4D11 F(ab′)2(5 × 106 per mouse, iv) followed by IL-2 injection (5 × 104 IU per mouse, ip) of all mice for 3 consecutive days. Pooled data from 2 independent experiments (n = 20 per group except for 4D11 F(ab′)2–treated group in which n = 10) are shown. The P value indicates a significant difference between groups injected with NK cells treated with 5E6 or 4D11 F(ab′)2 as determined by log-rank test.
While in vivo administration of 5E6 F(ab′)2 demonstrates that blockade of Ly49C and I inhibitory receptors increases antitumor activity, it does not distinguish NK-specific activity from that of the minor population of T cells also expressing the inhibitory receptors.13 To rule out the involvement of this T-cell subset, mice were injected with the mixture of C1498 and NK cells that were cocultured with or without 5E6 F(ab′)2 for 24 hours. Reduction in tumor growth that results from the coculture of NK and tumor cells in the presence of 5E6 F(ab′)2 was not sufficient to affect survival compared with the control group that received NK and C1498 cocultures without 5E6 F(ab′)2(Figure 3B). Our preliminary observation on the kinetics of C1498 growth in vivo suggested that the leukemia cells appear to remain dormant for 2 to 3 weeks, after which rapid tumor growth is detected in the animal (data not shown). Therefore, we examined whether adoptive transfer of NK cells preincubated ex vivo with the F(ab′)2into the tumor-bearing mice can result in increased antitumor effects. Adoptive transfer of NK cells that were treated with NMS, 5E6, or 4D11 F(ab′)2 was performed at days 18 and 25 after the initial injection of the animals with the tumor and NK cell mixture that was cocultured for 24 hours. Figure 3C demonstrates that adoptive transfer of IL-2–activated NK cells treated with 5E6 F(ab′)2 ex vivo resulted in a significant increase in the survival of mice, with 50% long-term survivors (P = .0004). In contrast, no significant difference in survival was observed between mice injected with NK cells treated with NMS or 4D11 F(ab′)2. Taken together, these results demonstrate that immunotherapy using NK cells with blockade of Ly49C and I receptors using 5E6 F(ab′)2fragments augments antitumor effects in vivo.
Discussion
The concept of removing inhibitory signals to optimize immune responses has been receiving increased attention with regard to cancer therapy. It has been demonstrated that CTLA-4 blockade results in enhancement of antitumor immunity against poorly immunogenic tumor cells and increased memory responses.20 Similarly, blocking NK inhibitory receptors may be necessary for optimal antitumor effects mediated by NK cells, even those activated with stimulatory cytokines, such as IL-2. In this study, we have shown that blockade of NK inhibitory receptors can promote antitumor responses both in vitro and in vivo.
Previous studies have demonstrated that modulation of MHC class I expression on various tumor cells influences the susceptibility of these cells to NK-mediated cytotoxicity.23 The inability of the 5E6+ NK cell subset to effectively lyse C1498 or EL4 tumor cells bearing H2b demonstrates that class I expression by tumor cells can play an important role in evasion from detection by NK cell subsets. In spite of comparable levels of class I expression between C1498 and EL4 cells, the extent of resistance to NK killing exhibited by C1498 is different from EL4 (Figure 1B). NK cells may recognize other tumor-specific determinants via activating receptors9,24 25 or other receptors that contribute to tumor cells' susceptibility to lysis. However, the increase in cytotoxicity that is mediated by the 5E6+ subset as a result of the blockade of Ly49C and I receptors indicates that inhibition of the negative signals induced via the inhibitory receptors enhances antitumor effects.
Whereas the 4-hour cytotoxicity assays show the effects of 5E6 F(ab′)2 on the sorted NK cell subset, the same effect could not be observed if a mixed population of NK cells was used (data not shown). This may be due to the sensitivity of a short-term cytotoxicity assay to detect the differences in the subset of NK cells. However, we have demonstrated that blockade of Ly49C and I receptors resulted in a significant inhibition of tumor growth in vitro even if a mixed population of NK cells was used in clonogenic assays. More importantly, the specificity of the suppressive effects on tumor growth was demonstrated with the use of F(ab′)2 fragments of both 5E6 and 4D11. Blockade of Ly49C and I receptors, which have been shown to bind H2b as well as H2d,22decreased the growth of tumors bearing MHC class I of either haplotype. However, blockade of Ly49G2 resulted in decreased growth of P815 (H2d) only, demonstrating the specificity of the inhibitory receptor blockade for the Ly49 determinants binding the appropriate MHC.
Recently, it has been reported that activation and recruitment of NK cells to the sites of tumor growth depend on the expression of MHC class I by the tumor.26 However, the relationship between MHC class I expressed by the tumor and particular NK subsets was not assessed. In this study, increased survival of tumor-bearing mice treated with 5E6 F(ab′)2 (Figure 3A) demonstrates that this subset is responsible for decreased antitumor activity against the syngeneic tumor and that blockade of Ly49C and I receptors increases antileukemia effects. We have observed that culturing C1498 with NK cells in the presence of 5E6 F(ab′)2 prior to injection does not have a significant effect on the survival of mice compared with the control cocultures without the F(ab′)2 fragments (Figure 3B). Our data also show that adoptive transfer of 5E6 F(ab′)2–treated NK cells is more effective in promoting antitumor effects compared with control-treated NK cells when mice were challenged with a reduced lethal dose of tumor cells by prior exposure to NK cells; however, when mice were injected with a higher dose, increased antitumor effects mediated by 5E6 F(ab′)2–treated NK cells could not be observed (data not shown). These results suggest that there may be a threshold at which the animals succumb to tumor. While tumor growth measured in vitro is significantly reduced by blockade of Ly49C and I during the coculture (Figure 2), the coculture alone may not be sufficient to reduce the tumor burden below the threshold level in vivo. However, in vivo studies indicate that continual blockade of NK inhibitory receptors by 5E6 F(ab′)2 treatment of animals or multiple injections of NK cells that are treated ex vivo with the antibody augments antitumor effects and can reduce the tumor burden below the threshold level.
As certain subsets of NK cells express inhibitory receptors that recognize self-MHC, it is possible that autoreactivity may result from the blockade of these inhibitory receptors. In vitro studies using cocultures of activated NK and bone marrow cells with or without F(ab′)2 fragments of the mAbs as well as in vivo studies, such as bone marrow transplantation with NK cells treated with F(ab′)2 fragments of mAbs against Ly49 inhibitory receptors, indicated no adverse effects of Ly49C and I blockade on growth of normal hematopoietic progenitors (manuscript in preparation).
It has been suggested that NK cells are responsible for controlling a low tumor burden at an initial stage until the adaptive arm of the immune system plays a major role in mediating antitumor responses.1,27 Therefore, blocking the inhibitory receptors expressed on a major subset of NK cells can be a powerful means to eradicate tumors when the tumor burden is minimal as that occurs after cytoreductive therapy. The significant effects observed with blockade of a subset representing 35% to 60% of NK cells also suggest that the combination of antibodies against multiple subsets may lead to even more potent antitumor responses. The effectiveness of a blockade of Ly49 inhibitory receptors in a purging model, in which animals are transplanted with bone marrow cells contaminated with tumors and F(ab′)2-treated NK cells, is currently being investigated. The results from our studies also suggest that the NK inhibitory receptor blockade may be applied to enhance immune responses to viral infections, such as murine cytomegalovirus, which encodes an MHC class I homologue to evade the immune system.28 29
Taken together, these results demonstrate for the first time that Ly49 receptors expressed on NK cell subsets can be responsible for diminishing antitumor responses and that blockade of these receptors augments antitumor effects. Thus, blockade of NK inhibitory receptors can be of potential use in increasing the efficacy of immunotherapy for cancer.
We thank Drs Robert H. Wiltrout and Scott K. Durum for critically reviewing the manuscript and Steve Stull and De Ming Zhou for their excellent technical expertise.
Funded in whole or in part with federal funds from the National Cancer Institute, National Institutes of Health (NIH), under contract No. N01-CO-56000 and supporting grants NIH R01 CA 72669 and CA 70134.
Both senior authors, W.J.M. and M.B., contributed equally to this work.
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
William J. Murphy, SAIC-Frederick, Bldg 567, Rm 210, Frederick, MD 21702; e-mail: murphyw@ncifcrf.gov.