Abstract
Like cellular transplantation, gene therapy is often limited by immune rejection of the newly expressed antigen. In a model of gene transfer in muscle, delivery of the influenza hemagglutinin (HA) membrane protein by adeno-associated virus (AAV) is impaired by a strong immune response that leads to a rapid rejection of the transduced fibers. We show here that injection of HA-specific CD4+CD25+ T cells from T-cell receptor (TCR)-transgenic animals, concomitant with gene transfer, down-regulates the anti-HA cytotoxic and B-lymphocyte responses and enables persistent HA expression in muscle. This demonstrates for the first time that adoptive transfer of antigen-specific CD4+CD25+ regulatory T cells can be used to induce sustained transgene engraftment in solid tissues. (Blood. 2003;102:4326-4328)
Introduction
Successful treatment of genetic disorders by gene therapy requires long-term transgene expression, which is often impaired by immune rejection. We observed that upon gene transfer into skeletal muscles by adeno-associated virus (AAV) vectors, intracytoplasmic non-self-transgene products such as βgalactosidase are weakly immunogenic, in contrast to membrane-bound transgene products that are rapidly rejected.1 Intramuscular injection of recombinant AAV vectors coding for the influenza hemagglutinin transmembrane protein (HA) results in T-cell priming and muscle fiber destruction likely due to efficient presentation of HA by dendritic cells.2 We have previously observed that this immune response can be prevented by blocking the CD40/CD40L pathway2 or by transferring large numbers of anergic T cells derived from a tolerant donor expressing both HA and anti-HA T-cell receptor (TCR).3
To induce antigen-specific tolerance in gene therapy protocols, the immunoregulatory CD4+CD25+ T cells are now particularly attractive. These cells are implicated in peripheral self-tolerance,4 as they were shown to regulate autoreactive T cells in mouse models of diabetes5 or inflammatory bowel disease6 and to interfere with deleterious immune response arising after transplantation.7,8 Here we demonstrate that transfer of HA-specific CD4+CD25+ T cells from a nontolerant donor down-regulates both B- and T-cell responses against HA and prolongs transgene engraftment in the skeletal muscle.
Study design
Mice, vectors, antibodies, and histology
Purification of CD4+CD25+ T cells
Splenocytes and lymph node cells were incubated with biotinylated anti-CD25 Ab (7D4) and streptavidin microbeads, followed by magnetic cell separation using LS columns (Miltenyi Biotec, Paris, France). Cells were further stained with anti-CD4-CyChrome and streptavidin-phycoerythrin (PE), sorted on a MoFlow (DakoCytomation, Freiburg, Germany) and injected into the tail vein in 0.1 to 0.2 mL phosphate-buffered saline (PBS).
Cytotoxic assay
At indicated time points, 5 × 107 splenocytes were stimulated in vitro with HA512-520 peptide (1 μM) in RPMI 1640 medium supplemented with 10% fetal calf serum (FCS), 2 mM l-glutamine, 50 μM 2β-ME, and antibiotics (complete medium [CM]). After 6 days, the bulk responder populations were tested in a 4-hour cytotoxic assay of chromium release against P815 target cells.
Interferon γ (IFNγ) enzyme-linked immunospot (ELISPOT) assay
Freshly isolated splenocytes (3 × 106/well and serial dilutions) were cultured in CM with or without 10 μM HA512-520. For each assay, concanavalin A (ConA) was added (5 μg/mL) as a positive control. After 20 hours, spots were revealed10 and counted using a Bioreader 2000 (BIO-SYS, Karben, Germany).
Measurement of anti-HA Abs
Enzyme-linked immunosorbent assay (ELISA) was done using influenza virus PR/8/34 as antigen. Serum samples and purified anti-HA Ab standard of immunoglobulin G (IgG) isotype (H37/38, 1.4 mg/mL) were serially diluted, detected with peroxidase-conjugated goat anti-mouse IgG (Vector Laboratories, Burlingame, CA), and revealed with TMB solution (Kirke-gaard-Perry, Gaithersburg, MD).
Results and discussion
Upon transfer of AAV-HA into muscles of BALB/c mice, the immune response leads to destruction of all transduced cells by 2 to 3 weeks.2 Indeed, we detected at day 14, which is the peak of the response, a high frequency of IFNγ-secreting splenocytes against the Kd/HA512-520 epitope (Figure 1A). In an attempt to diminish the cellular response to HA, AAV-HA-transduced mice were injected twice at a 4-day interval with 106 HA-specific CD4+CD25+ T cells (HA-Tregs) from TCR-HA transgenic mice, which express an I-Ed/HA110-120-specific TCR.9 Here, compared with untreated mice, injection of HA-Tregs induced a dramatic decrease in the frequency of transgene-specific cytotoxic T lymphocytes (CTLs) at day 14 (Figure 1A).
HA-specific CD4+CD25+ cells suppress anti-HA B- and T-cell immune responses. At day 0, anesthetized BALB/c mice were injected into the tibialis anterior with 25 μL AAV-HA (6 × 1011 physical particles (pp)/mL) and were either untreated (No cells) or intravenously injected twice at days 0 and 4 with 106 CD4+CD25+ cells from TCR-HA mice (HA-Tregs). Their splenocytes were tested at day 14 in a standard IFNγ-ELISPOT assay against the HA512-520 epitope, and spot-forming units (SFU) are represented after subtraction of background spots obtained with unpulsed splenocytes (A). To monitor the specificity of the response, AAV-HA-transduced mice were untreated (No cells), or injected twice with 106 CD4+CD25+ cells from TCR-HA mice (HA-Tregs), CD4+CD25-cells from TCR-HA mice (HA-Th), or CD4+CD25+ cells from BALB/c mice (Tregs). Splenocytes were tested at day 35 by IFNγ-ELISPOT assay (B), restimulated in vitro for 6 days with HA512-520, and tested in cytotoxic assay (C), and mouse sera were assayed for the presence of anti-HA IgG (D). For ELISPOT and ELISA assays, results represent the mean of 3 mice per group and are expressed as mean ± standard error of the mean (SEM). For cytotoxic assays, the percentage of specific lysis was calculated as the difference in lysis between HA512-520-pulsed (1 μM) and unpulsed P815 targets cells. Results from one representative mouse per group are shown. Comparison of SFU and IgG titers were performed using Mann-Whitney t test. Statistically significant P values less than .01 were found between HA-Tregs and each other group (**), and less than .05 between HA-Th and No cells (*).
HA-specific CD4+CD25+ cells suppress anti-HA B- and T-cell immune responses. At day 0, anesthetized BALB/c mice were injected into the tibialis anterior with 25 μL AAV-HA (6 × 1011 physical particles (pp)/mL) and were either untreated (No cells) or intravenously injected twice at days 0 and 4 with 106 CD4+CD25+ cells from TCR-HA mice (HA-Tregs). Their splenocytes were tested at day 14 in a standard IFNγ-ELISPOT assay against the HA512-520 epitope, and spot-forming units (SFU) are represented after subtraction of background spots obtained with unpulsed splenocytes (A). To monitor the specificity of the response, AAV-HA-transduced mice were untreated (No cells), or injected twice with 106 CD4+CD25+ cells from TCR-HA mice (HA-Tregs), CD4+CD25-cells from TCR-HA mice (HA-Th), or CD4+CD25+ cells from BALB/c mice (Tregs). Splenocytes were tested at day 35 by IFNγ-ELISPOT assay (B), restimulated in vitro for 6 days with HA512-520, and tested in cytotoxic assay (C), and mouse sera were assayed for the presence of anti-HA IgG (D). For ELISPOT and ELISA assays, results represent the mean of 3 mice per group and are expressed as mean ± standard error of the mean (SEM). For cytotoxic assays, the percentage of specific lysis was calculated as the difference in lysis between HA512-520-pulsed (1 μM) and unpulsed P815 targets cells. Results from one representative mouse per group are shown. Comparison of SFU and IgG titers were performed using Mann-Whitney t test. Statistically significant P values less than .01 were found between HA-Tregs and each other group (**), and less than .05 between HA-Th and No cells (*).
At day 35, 3 weeks after the peak of the response, HA-Treg injections still severely impaired the cellular response compared with nontreated mice (Figure 1B). We analyzed the specificity of this suppressive effect by comparing the activity of HA-Tregs with unspecific CD4+CD25+ cells from wild-type BALB/c mice (Tregs) or with helper HA-specific CD4+CD25- cells (HA-Th). We found that the CTL response was abolished only by HA-Tregs (P < .01), whereas HA-specific T-helper cells enhanced this response (P = .04).
Next, we determined whether the HA-specific cytotoxic response was also suppressed. Consistent with the IFNγ ELISPOT assay, the cytolytic activity assayed after 6 days of in vitro restimulation was uniquely impaired in mice treated with HA-Tregs (Figure 1C). As the humoral B-cell response can also interfere with engraftment of the transmembrane HA protein, we looked for the presence of anti-HA Abs at day 35 and found that HA-Tregs decreased the concentration of circulating anti-HA IgG by 10-fold (P < .01). Nonspecific Tregs had no effect and the CD4+CD25- HA-specific helper T cells even enhanced the IgG response (Figure 1D). Altogether, these results demonstrate that HA-specific B- and T-cell responses are uniquely impaired by the injection of HA-Tregs. Similar conclusions were reached from results obtained at day 14 (data not shown). Whether HA-Tregs inhibit the function of antigen-presenting cells or directly recognize HA110-120-loaded I-Ed molecules on B lymphocytes is still not known.
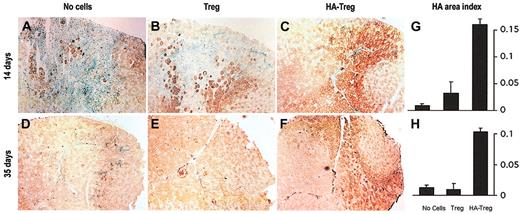
As expected, in mice treated with unspecific Tregs or untreated mice, all the transduced muscles were inflamed, infiltrated by numerous cells identified by methyl blue nuclear staining, and HA-positive fibers were destroyed at the peak of the response at day 14 (Figure 2A-B). In marked contrast, HA-Treg injection decreased local cellular infiltration and allowed sustained HA expression in muscle fibers in all treated mice (Figure 2C). As for the B-cell response, HA-specific helper T cells exacerbated this rejection (data not shown). Computer-assisted image analysis revealed that whereas less than 3% of the tibialis anterior area was stained in control groups, all HA-Treg-treated mice harbored up to 16% area of HA-transduced fibers (Figure 2G). At day 35, Figure 2D-E show that in control mice and in mice treated with unspecific Tregs, all transduced fibers were rejected and replaced by regenerating non-HA-expressing muscle fibers. In contrast, we found that HA-Treg-treated mice accepted HA-transduced muscle cells as shown by immunostaining detection and HA expression measurement (Figure 2F,H). Despite an absence of inflammation, we consistently observed a lower percentage of HA expression at day 35 than at day 14. Repetitive infusions of HA-Tregs over 1 month were unable to prolong HA engraftment beyond 50 days, excluding the hypothesis of insufficient Treg lifetime (data not shown). It is possible that a toxic effect of HA on muscle is responsible for the observed decrease in HA engraftment.
HA-specific CD4+CD25+ cells allow transgene engraftment in transduced muscle. BALB/c mice were injected intramuscularly at day 0 with AAV-HA, and were either untreated (A,D) or injected intravenously at days 0 and 4 with 106 CD4+CD25+ cells from BALB/c mice (B,E) or CD4+CD25+ cells from TCR-HA mice (C,F). At days 14 (A-C) and 35 (D-F), muscles were frozen and HA expression was assayed by immunohistochemistry using horseradish peroxidase (HRP)/diaminobenzidine (DAB) staining in brown on sections counterstained with methyl green, which stains the nuclei of muscle and infiltrating lymphoid cells in blue/green. Images are representative of 3 mice per group. Original magnification × 40. Quantification of HA expression was assessed by computer-assisted image analysis (Histolab; Microvision Instruments, Evry, France). For each mouse in each condition, 5 to 10 entire transverse sections of tibialis anterior were measured. The total section and HA-positive areas were determined by image texture and HRP/DAB color analysis, respectively. The reproducibility of image analysis was controlled using normal muscle sections as a standard on each slide. Results are expressed as an index of HA-positive area over the total tibialis anterior area and represent the mean ± SEM of 3 mice per group, at days 14 (G) and 35 (H).
HA-specific CD4+CD25+ cells allow transgene engraftment in transduced muscle. BALB/c mice were injected intramuscularly at day 0 with AAV-HA, and were either untreated (A,D) or injected intravenously at days 0 and 4 with 106 CD4+CD25+ cells from BALB/c mice (B,E) or CD4+CD25+ cells from TCR-HA mice (C,F). At days 14 (A-C) and 35 (D-F), muscles were frozen and HA expression was assayed by immunohistochemistry using horseradish peroxidase (HRP)/diaminobenzidine (DAB) staining in brown on sections counterstained with methyl green, which stains the nuclei of muscle and infiltrating lymphoid cells in blue/green. Images are representative of 3 mice per group. Original magnification × 40. Quantification of HA expression was assessed by computer-assisted image analysis (Histolab; Microvision Instruments, Evry, France). For each mouse in each condition, 5 to 10 entire transverse sections of tibialis anterior were measured. The total section and HA-positive areas were determined by image texture and HRP/DAB color analysis, respectively. The reproducibility of image analysis was controlled using normal muscle sections as a standard on each slide. Results are expressed as an index of HA-positive area over the total tibialis anterior area and represent the mean ± SEM of 3 mice per group, at days 14 (G) and 35 (H).
In preclinical transplantation models, adoptive transfer of donor regulatory T cells was proven useful for long-term graft acceptance.11 For instance, CD4+CD25+ T cells from either naive or tolerant donor mice were shown to suppress skin graft rejection in lymphopenic recipients reconstituted with a limited number of normal CD4+ T cells.12 These reports however have not fully addressed the importance of the TCR specificity of Tregs or the role of the tolerance state of the donor. Here, infusion of transgene-specific CD4+CD25+ cells arising from a nontolerant antigen-free donor abolishes the antitransgene CTL and Ab immune responses and allows sustained transgene engraftment. Moreover, compared with nonspecific Tregs, the same dose of HA-Tregs leads to suppression, clearly showing the importance of the TCR specificity. Consistently, dose-response experiments showed that infusion of 10 times less HA-Tregs still impaired the immune response (data not shown), pointing out the role of TCR specificity in CD4+CD25+-based suppression.
A variety of approaches have been proposed to induce specific regulatory T cells, including the use of dendritic cells13-15 or ectopic expression of the Foxp3/Scurfin transcription factor.16-18 This, together with the enhanced transgene engraftment that we report here, may provide novel tolerization opportunities in gene therapy.
Prepublished online as Blood First Edition Paper, July 31, 2003; DOI 10.1182/blood-2003-05-1454.
Supported by the Association Française contre les Myopathies (AFM) and by a grant Action Thématique Incitative from Génopole Evry (ATIGE).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We wish to thank Benoît Salomon for valuable advice. We also thank Christophe Georger, Julien Picot, Philippe Rameau, Thibaut Marais, and Laetitia Van Wittenberghe-Baudry for immunohistology, cell sorting, and mice preparation; Claudine Rousseau and Jean-Claude Manuguerra (Institut Pasteur, Paris, France) for their invaluable help with ELISA; Patrick Gonin for statistical analysis; and Terence Partridge and Anne Galy for critical reading of the manuscript.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal